 ERAXION / ISTOCK
ERAXION / ISTOCK
Tips for Administering the Inferior Alveolar Nerve Block
Tips for Administering the Inferior Alveolar Nerve Block Providing sufficient pain control to patients is critical to dental hygiene care.
This course was published in the November 2015 issue and expires November 20, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the anatomic locations of the inferior alveolar nerve.
- Discuss the administration of the inferior alveolar nerve block.
- Explain the important role dental hygienists play in administering local anesthesia.
Dental hygienists often need to provide profound local anesthesia to ensure patient comfort during periodontal instrumentation. The IANB is considered a true nerve block because solution is deposited near a large nerve trunk, resulting in regional anesthesia. In light of the dense cortical bone in molar areas, the IANB is often a better choice than local anesthetic infiltration when it comes to achieving appropriate mandibular anesthesia.2 Unfortunately, this frequently used approach continues to challenge clinicians because mandibular blocks are sometimes incomplete, likely the result of varying patient anatomies or poor technique.
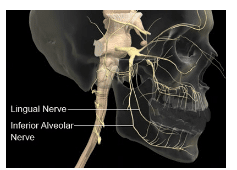
The mandibular division (V3) of the trigeminal nerve exits the skull through the foramen ovale and divides into posterior and anterior divisions. The anterior division is primarily motor, enabling the muscles of mastication; however, the buccal nerve is a mostly sensory branch. It is anesthetized when soft tissue anesthesia of the buccal aspects of the mandibular molars and premolars is desired.3 The posterior division of the mandibular nerve is mainly sensory and includes the lingual, inferior alveolar, and auriculotemporal nerves (Figure 1). The inferior alveolar nerve further divides into two terminal branches inside the mandibular canal near the premolars: the mental and incisive nerves.3
MEDICAL IMAGES, UNIVERSAL IMAGES GROUP/SCIENCE PHOTO LIBRARY
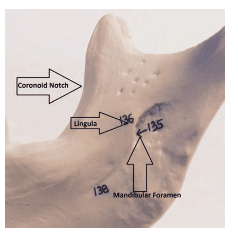
The inferior alveolar nerve travels through the infratemporal space, medial to the lateral pterygoid muscle, and passes through the pterygomandibular space next to the sphenomandibular ligament and the medial surface of the mandibular ramus.4 Here, the inferior alveolar nerve enters the mandibular foramen, which is bordered by the lingula—a bony protuberance that serves as an attachment for the sphenomandibular ligament.5 Once inside the canal, the nerve innervates each tooth through the root apices.2 Moving anteriorly in the mandibular canal, it divides further into the mental and incisive nerve branches. The former innervates the anterior teeth to the midline, the latter provides sensory innervation to the lower lip on the same side.5 A typical IANB also anesthetizes the lingual nerve.4 The IANB provides anesthesia to the mandibular teeth up to the midline, body of the mandible, inferior to the ramus, buccal mucoperiosteum anterior to the mental foramen, anterior two-thirds of the tongue, floor of the oral cavity, and lingual soft tissues and periosteum.6 The maxillary artery also travels along the path of the IANB in the infratemporal and pterygomandibular spaces. A terminal branch of the carotid artery, the inferior alveolar artery, and inferior alveolar vein can also be found in this space.4
LANDMARKS
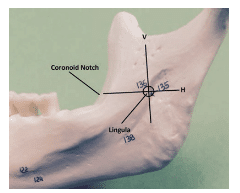
Understanding the location of the mandibular foramen is important for effective administration of the IANB. The target area is the inferior alveolar nerve as it travels on the medial aspect of the ramus, prior to its entry into the mandibular foramen and located inferior to the lingula (Figure 2).6 The optimal location varies between patients, but depositing the anesthetic near the nerve just before it enters the mandibular foramen is key.3 Thus, it is important to adhere to specific anatomical landmarking for successful administration. Two important anatomical landmarks are the coronoid notch and the pterygomandibular raphe. The coronoid notch (Figure 3) is a bony landmark that is the deepest part of the ramus on the anterior border. The coronoid notch extends inferiorly from the external oblique ridge, on the lateral surface of the mandible, to the superior aspect of the coronoid process. Anteriorly, the buccinator and superior pharyngeal constrictor muscle of the pharynx form the pterygomandibular raphe.7 The raphe, a tendinous thickening, is an important soft tissue anatomical landmark and represents the medial extent of the penetration area. Thus, penetration must be made slightly lateral to the raphe.4,5 The patient must open wide so the operator can adequately view the raphe and properly locate the coronoid notch. The pterygomandibular space contains not only the inferior alveolar nerve, but also the inferior alveolar artery and vein, lingual nerve, nerve to the mylohyoid, and sphenomandibular ligament and fascia (Figure 4).8
There are three parameters that must be determined to correctly locate the anatomical landmarks: the height of injection, the anterior/posterior placement of the needle/barrel, and the depth of penetration.6 The height of injection is first ascertained by placing the index finger or thumb of the nondominant hand in the coronoid notch. An imaginary horizontal line is made from the notch to the pterygomandibular raphe. This line is parallel to the occlusal plane of the mandibular teeth and will lie 6 mm to 10 mm above the occlusal plane.6 A vertical intersection of this line will determine the precise entry point of the needle (Figure 5). This insertion point lies between the coronoid notch and pterygomandibular raphe and is located three-quarter distance from the coronoid notch or one-quarter distance from the deepest part of the pterygomandibular raphe (Figure 2).5
Next, the aspirating syringe barrel should be positioned above the second premolar on the contralateral side of the mouth for best access and precise angulation. The third parameter is the depth of penetration. A 32 mm-long needle is advanced into the pterygomandibular space until bone is contacted superior to the mandibular foramen where the IANB enters into bone at approximately a depth of 20 mm to 25 mm or three-quarters of the needle’s length, depending on the shape of the mandible.9 The operator then will withdraw the needle 1 mm away from the periosteum. Two aspirations will usually ensure the needle is not in a blood vessel. If no blood is aspirated, the operator will typically administer three-quarters of the anesthetic over 1 minute.6 If blood is aspirated, the operator needs to change both the needle and the cartridge and begin again. The onset of anesthesia is approximately 3 minutes to 5 minutes. Articaine may be faster with an onset of 1 minute to 3 minutes.6 The operator should confer with the patient regarding his or her symptoms of numbness and wait the recommended amount of time to ensure anesthesia is successful before beginning the therapeutic procedure or considering readministration of anesthetic.
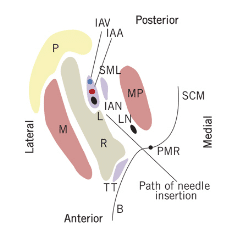
COURTESY OF KHOURY JN, MIHAILIDIS S, GHABRIEL M, TOWNSEND G. APPLIED ANATOMY OF THE PTERYGO – MANDIBULAR SPACE: IMPROVING THE SUCCESS OF INTERIOR ALVEOLAR NERVE BLOCKS. AUST DENT J. 2011:56:112–121.
CONCERNS
While the IANB is the most commonly administered injection, it continues to challenge clinicians. According to Basset, the failure rate of the IANB is 10% to 31%, whereas Khalil estimates the injection’s failure rate at 20% to 25%.3,4 Various reasons contribute to IANB failure rates, but two of the most common are poor operator technique and anatomical variability.2,3,7–10
When administering the IANB, if the bone is contacted too soon, deposition of the anesthetic may not reach the target point, causing inadequate anesthesia. The operator should withdraw the needle slightly and move the barrel of the syringe more anteriorly over the canine/first premolar area to angle the needle more posteriorly. Consequently, if bone is not contacted, the needle may be located too far posteriorly, which may result in anesthetizing the facial nerve (CN VII), causing temporary unilateral paralysis of facial muscles.11 To avoid this pitfall, the needle must always contact bone at the suggested 20 mm to 25 mm depth. Injecting while the needle tip is touching bone prevents facial anesthesia.4,6 The operator should withdraw the needle slightly, reposition the barrel of the syringe more posteriorly, angling the needle more anteriorly toward the target point.11 If all guidelines are followed but anesthesia is not achieved, the operator should repeat the procedure, administering an additional three-quarters of a cartridge. If failure is experienced again, anatomical variations and poor operator technique must be considered.
ANATOMICAL VARIATIONS
A number of anatomic variables can interfere with achieving optimal anesthesia. For example, an accessory mylohyoid nerve, which is considered motor, sometimes carries sensory information from the mandibular teeth.2,8 It may supply at least some pulpal innervations to the mandibular first molar. If this is the case, the point at which the mylohyoid branches off the inferior alveolar nerve becomes an important factor to consider.10 The mylohyoid branches off the inferior alveolar nerve as it descends toward the mandibular foramen.6,8 The branching may occur as far as 14.7 mm superior and posterior to the lingula.10 After branching, the mylohyoid nerve courses inferiorly and anteriorly in the mylohyoid groove along the medial surface of the mandible to innervate the mylohyoid muscle.6 The conventional IANB frequently will not diffuse to the mylohyoid nerve, resulting in a lack of anesthesia to the first molar area. An alternative is to perform a Gow-Gates injection, a high mandibular block that targets the lateral anterior surface of the condylar neck just below the insertion of the lateral pterygoid muscle.12 Another strategy is to buccally infiltrate adjacent to the apices of the mandibular first molar by depositing one-quarter of the cartridge about 3 mm to 5 mm in depth.11
A bifid mandibular nerve may complicate the ability to achieve proper anesthesia in the mandibular anterior teeth.2,8 A panoramic radiograph can help locate a bifid nerve.8 Finally, a contralateral innervation of the incisors may interfere with complete quadrant anesthesia, prompting the administration of an additional injection, such as a mental nerve block, in the opposite quadrant.
Other considerations include a wide or long ramus, bulky musculature, excess adipose tissue, an infection in the area where the anesthetic solution is deposited, or an abnormal position of the mandibular foramen.12 All possibilities should be considered so that the operator can make alterations to the traditional IANB or use the IANB with alternate techniques.
OPERATOR TECHNIQUE
Because the total length and depth of penetration to reach the target for the traditional IANB is 20 mm to 25 mm, short needles should be avoided.6 A short needle will generally not reach the target area without the risk of advancing to the hub of the needle and embedding the entire needle in tissue. The stress on the hub could cause the needle to break, as the hub-needle interface is the weakest part of the needle. Furthermore, needle gauge size should be 25 or 27. Thirty-gauge needles should not be used for IANBs because they are the thinnest and least rigid, which raises the risk of deflection and breakage.13 Finally, the patient should be placed in a supine position and instructed to open wide so the operator has maximum visibility and access to the injection site. The supine position is also preferable in the event of a medical emergency.
The suggested amount of anesthetic is three-quarters of the cartridge or approximately 1.5 ml of solution. This is generally adequate to provide the appropriate diffusion through the nerve and achieve profound anesthesia. The smallest dose possible should be used to achieve clinically effective anesthesia.4 Some clinicians reserve solution on withdrawal to deposit near the lingual nerve. Proper positioning of the IANB, however, will likely ensure both inferior alveolar nerve and lingual nerve anesthesia, as these nerves generally move in close proximity to the lingula.
Positive aspiration occurs in approximately 10% to 15% of IANB administrations. Two aspirations are recommended to confirm that the lumen of a needle is not located within a blood vessel.6 While local anesthetics are relatively safe, intravascular injection of local anesthetic—especially with a vasoconstrictor—may result in toxicity of the cardiovascular and central nervous systems.14 Overdose symptoms will usually occur within the first 5 minutes after administration and dental hygienists need to know the signs and symptoms of toxicity and be prepared to react accordingly. One region should be anesthetized and treatment completed before administering additional anesthetic solution in another area. Following these guidelines will reduce the chances of systemic toxicity.15 In most patients, a vasoconstrictor may be used to reduce systemic toxicity. This is because it slows the systemic absorption of the anesthetic agent, while potentially providing hemostatic benefits to the operator.16 Finally, the administration of an entire anesthetic cartridge should take 1 minute. Slow injection is often less painful for the patient and helps to prevent an overdose of anesthetic.6
ROLE OF DENTAL HYGIENISTS
Local anesthesia has been administered safely and effectively by dental hygienists since 1971. Many dental hygienists are well educated in the administration of local anesthesia.17 While practice acts differ in each state, regulatory bodies and state boards monitor the quality of care delivered to protect patients. In a 2005 study, the majority of respondents reported no disciplinary actions for dental hygienists delivering local anesthesia.18 Most states require dental hygienists to administer local anesthesia under the direct supervision of a dentist, however six states—Arkansas, Arizona, Colorado, Idaho, Minnesota, and Oregon—allow dental hygienists to administer anesthesia under general supervision.19
Most dentist employers appreciate that dental hygienists can administer local anesthesia because it contributes to a more efficiently run practice. Anderson reports approximately 90% of dental hygienists educated in local anesthesia believe this skill set would have a positive effect on gaining employment. Approximately 95% of dentists have delegated pain control to a dental hygienist.21 In many states, dental hygienists can administer local anesthesia for dental and dental hygiene procedures.1 Research supports nonrestrictive statutory language that encourages pain control delivered by dental hygienists as integral members of the oral health care team.20
CONCLUSION
The IANB can be a challenging injection to administer. Mastery of the technique includes understanding anatomy and the ability to use alternative techniques to provide better patient outcomes and improved pain control. Proficiency in the administration of the IANB should be embraced by dental hygienists, as multiple teeth and soft tissue anesthesia—both buccally and lingually—is required when scaling and root planing. Pain management is an essential skill set needed by today’s dental hygienist.
REFERENCES
- The American Dental Hygienists’ Association. LocalAnesthesia Administration By Dental Hygienists State Chart. Available at: adha.org/resourcesdocs/7514_Local_Anesthesia_Requirements_by_State.pdf. Accessed October 8, 2015.
- DeSantis JL, Liebow C. Four Common Mandibular Nerve Anomalies that Lead to Local Anesthesia Failures. J Am Dent Assoc. 1996;127:1081–1086.
- Khalil H. A basic review on the inferior alveolar nerve block techniques. Anesth Essays Res.2014;8:3–8.
- Bassett KB, DiMarco AC, Naughton DK. Local Anesthesia for Dental Professionals . 2nd ed. UpperSaddle River, New Jersey: Pearson Education Inc; 2015.
- Fehrenbach MJ, Herring SW. Illustrated Anatomy of the Head and Neck . 4th ed. St. Louis: Elsevier-Saunders; 2012.
- Malamed S. Handbook of Local Anesthesia. 6th ed.St Louis: Elsevier-Mosby; 2013.
- Khoury J, Mihailidis S, Ghabriel M, Townsend G.Anatomical relationships within the human pterygomandibular space. Clin Anat. 2010:23:936–944.
- Khoury JN, Mihailidis S, Ghabriel M, Townsend G.Applied anatomy of the pterygomandibular space: improving the success of inferior alveolar nerve blocks. Aust Dent J. 2011:56:112–121.
- Thangavelu K, Kannan R, Senthil Kumar N.Inferior alveolar nerve block: Alternative technique. Anesth Essays Res. 2012;6:53–57.
- Wilson S, Johns P, Fuller PM. The inferior alveolarand mylohyoid nerves: an anatomic study and relationship to local anesthesia of the anterior mandibular teeth. J Am Dent Assoc.1984;108:350–352.
- Logothetis DD. Local Anesthesia for the Dental Hygienist. St. Louis: Elsevier-Mosby; 2012.
- Holliday R, Jackson I. Superior position of themandibular foramen and necessary alterations in the local anaesthetic technique: a case report. Br Dent J. 2011;210:207–211.
- Malamed SF. Is the mandibular nerve blockpassé? Am Dent Assoc. 2011; 142(Suppl 9):3S–7S.
- Taghavi Zenous A, Ebrahimi H, Mahdipour M,Pourshahidi S, Amini P, Batankhah M. The incidence of intravascular needle entrance during inferior alveolar nerve block injection. J Dent Res Dent Clin Dent Prospects. 2008;2:38–41.
- Becker DE, Reed KL. Essentials of local anestheticpharmacology. Anesth Prog. 2006;53:98–109.
- Hass DA. An Update on Local Anesthetics inDentistry. J Can Dent Assoc. 2002;68:546–551.
- Boynes SG, Zovko J, Bastin MR, Grillo MA,Shingledecker BD. Dental hygienists’ evaluation of local anesthesia education and administration in the United States. J Dent Hyg. 2011;85:67–74.
- Scofield JC, Gutmann ME, DeWald JP, CampbellPR. Disciplinary actions associated with the administration of local anesthetics against dentists and dental hygienists. J Dent Hyg. 2005;79:1–9.
- Boynes SG, Zovko J, Peskin RM. Local anesthesiaadministration by dental hygienists. Dent Clin North Am. 2010;54:769–778.
- Anderson JM. Use of local anesthesia bydental hygienists who completed a Minnesota CE course. J Dent Hyg. 2002;76:35-46.
From Dimensions of Dental Hygiene. November 2015;13(11):60–63.