Supporting Oral Health in Patients with Breast Cancer
Supporting Oral Health in Patients with Breast Cancer Dental hygienists play a vital role in helping these patients maintain their oral health.
This course was published in the November 2015 issue and expires November 20, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the risk factors for breast cancer.
- Discuss the treatments for breast cancer and their effects on oral health.
- Explain the appropriate oral care regimen that should be provided prior to initiating breast cancer treatment and during chemotherapy.
- List the implications of antiestrogen therapy on oral health.
Breast cancer affects nearly 232,000 women annually in the United States.1 The median age of diagnosis is 61.2 The average woman has a one in eight lifetime risk of developing breast cancer.3 The majority of cases will be diagnosed in post-menopausal women, and approximately 70% of these cancers express the estrogen receptor and/or the progesterone receptor and can be treated with antiestrogen therapy.4
Established risk factors for breast cancer include gender, increasing age, family history of breast cancer, early menarche, late menopause, long-term hormone replacement therapy, breast density, ethnicity, and genetics.5 Research suggests that consuming one alcoholic drink a day increases the risk of breast cancer by 7% and consuming two or three drinks per day raises the risk by 20%.6
TREATMENT
Breast cancer treatment is based on prognostic and predictive factors, including the histological grading (tumor severity); staging (how far cancer cells have spread); tumor cell responsiveness to various hormones or drugs; and patient’s age, overall health, and preferences.7,8 Breast cancer surgery provides tissue for the purposes of grading, staging, and assessing biomarkers. Depending on the cancer stage and the histologic and molecular profile of the tumor, systemic adjuvant therapy may be recommended to decrease the risk of developing distant metastases.9,10 Systemic therapies may include chemotherapy, targeted therapies such as trastuzumab, or antiestrogen therapy.7,11 These therapies may be considered either before or after surgery, based on the patient’s needs. Radiation therapy to the breast, chest wall, and/or local lymph node regions may be administered, but it does not replace surgery—the foundation of early-stage breast cancer management.
Approximately 75% of breast cancers express estrogen and/or progesterone receptors (ER, PR).12,13 Breast cancer can depend on ER/PR signaling for tumor growth and survival.14 Targeting these receptors with antiestrogen therapies decreases the risk of breast cancer recurrence.10 In premenopausal women, surgery, radiation, or chemical therapies with luteinizing hormone-releasing hormone inhibitors (goserelin, leuprolide, or triptorelin) may ablate ovarian estrogen. The use of oral adjuvant systemic antiestrogens, such as tamoxifen, is common. Post-menopausal women may be prescribed either tamoxifen or an aromatase inhibitor (anastrozole, exemestane, or letrozole).15 While breast cancer occurs in approximately 1% of men, nearly 90% of their tumors are ER positive. Treatment for male breast cancer patients is similar to female patients and includes surgery followed by systemic therapy (chemotherapy and/or antiestrogen therapy). The need for radiation treatment is based on the tumor stage and biomarkers.16
EFFECTS OF TREATMENT
Lymphedema may result during or following breast cancer treatment. It manifests as a swelling that occurs when protein-rich lymph fluid accumulates in the interstitial tissue. Both the arm and the breast area may be affected. Although the etiology is unknown, the removal of lymph nodes and radiation of the breast may contribute to this condition. Patients with breast cancer should take preventive steps to reduce their risk of developing or exacerbating lymphedema, such as vigilant skin care, including avoiding needle punctures or blood draws; taking blood pressure readings on the unaffected arm; and using compression garments.17,18 Patients who have had a mastectomy and their lymph nodes removed should have their blood pressure monitored on the unaffected side. Patients who have undergone a bilateral axillary node dissection may need to have a blood pressure reading on their wrist or calf. Leg readings, however, can be lower than those taken on the arm due to peripheral vascular disease.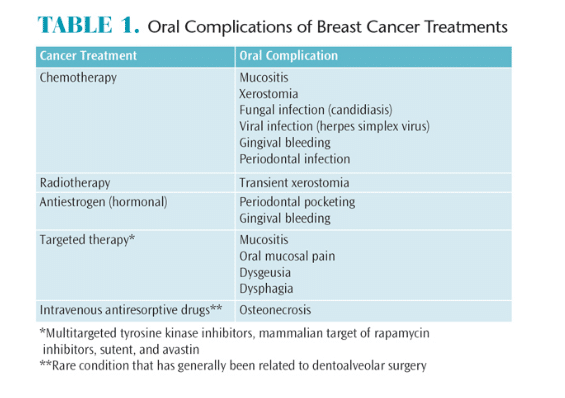
PRETREATMENT DENTAL CARE
Guidelines for the provision of oral care to patients with cancer have been developed by the National Institute of Dental and Craniofacial Research.20 These guidelines suggest patients receive a dental visit prior to beginning cancer treatment and provide suggestions for care during chemotherapy and radiation.20 However, there is no universally accepted precancer therapy dental protocol at this time. Regardless, poor oral health is associated with increased incidence and severity of oral complications among patients with cancer.21 As such, the involvement of the dental team may reduce the risk of oral complications.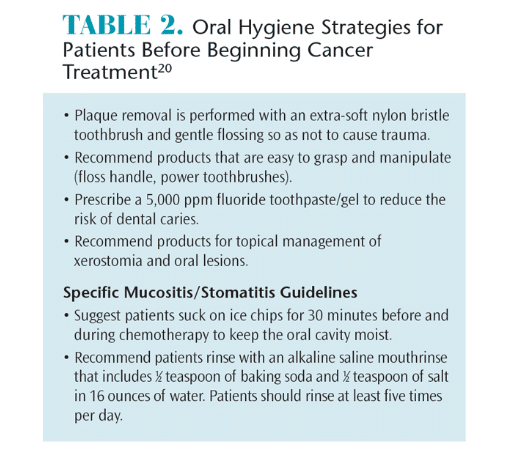
The pretreatment dental examination enables clinicians to determine a patient’s oral health status and to decide whether care should be initiated. If possible, this visit should take place as long as possible (at least 1 month) before the start of cancer treatment. Patients requiring oral surgery must have at least 2 weeks for healing before radiation therapy begins. Healing of oral surgical sites requires 7 days to 10 days prior to beginning myelosuppressive chemotherapy. Medical consultation is always indicated before performing invasive procedures.22
The dental team should develop a comprehensive oral care plan that eliminates potential sites of infection that could produce complications during cancer treatment. Specific areas to address include necrotic teeth, mucosal lesions, dental caries, periodontal diseases, ill-fitting dentures or orthodontic appliances, temporomandibular dysfunction, and xerostomia.
A comprehensive oral care plan must include oral hygiene strategies that may change throughout the stages of treatment. Patients should be counseled on tobacco cessation and the importance of limiting alcohol intake. Advise patients that some types of chemotherapy may cause temporary neuropathy with resulting numbness, tingling, pain, muscle weakness, or even swelling. These symptoms may impact a patient’s ability to perform oral hygiene. Dental hygienists play important roles in educating patients about appropriate nutritional intake, effective oral hygiene practices, and early detection of oral lesions during the pretreatment visit (Table 2).20
 CHEMOTHERAPY PHASE
CHEMOTHERAPY PHASE
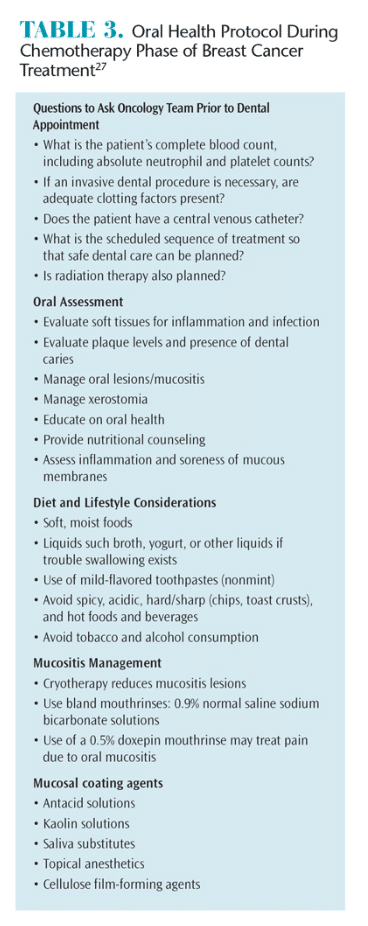
Chemotherapy drugs are used to destroy cancer cells by stopping them from growing or multiplying. Chemotherapy can decrease platelet numbers, which can increase bleeding and reduce clotting time. Furthermore, chemotherapy can lower white blood cell counts and increase the risk of infection. Blood work should be conducted 24 hours before dental treatment to determine whether the patient’s platelet count, clotting factors, and absolute neutrophil count are sufficient to prevent hemorrhage and infection. Treatment may need to be postponed if the platelet count is less than 50,000/mm3, abnormal clotting factors are present, and/or neutrophil count is less than 1,000/mm3.
Patients undergoing chemotherapy may also present with an indwelling venous access line for the administration of chemotherapy. Concerns regarding the need for antibiotic prophylaxis should be discussed with patients’ medical oncologists prior to treatment. Current guidelines do not recommend prophylactic antibiotic therapy for these patients because there isn’t evidence demonstrating that microorganisms associated with dental procedures cause infection of nonvalvular devices after implantation.23 However, clinical judgment should be used if the patient is undergoing an invasive dental procedure where Staphylococcus microbes may be present.
Oral mucositis is the inflammation of oral mucosa resulting from chemotherapeutic agents, which typically manifests as erythema or ulcerations.24 Oral mucositis presents in approximately 40% of patients receiving chemotherapy, with nearly half requiring medical intervention, including modification of the cytotoxic cancer therapy. Oral mucositis usually begins 7 days to 14 days after initiation of cytotoxic therapy and remains present for approximately 2 weeks after the therapy is complete. It often presents on the soft palate, buccal mucosa, tongue, floor of the mouth, and throat.25
Although it is difficult to predict which class of drugs may induce mucositis, some traditional chemotherapy drugs—such as fluorouracil, methotrexate, and doxorubicin—are known to cause acute mucositis. Mucositis resulting from targeted therapy may present differently from traditional chemotherapy with isolated ulcerations and mucosal pain (even in the absence of mucosal lesions).19
Topical cryotherapy may reduce mucositis caused by agents, such as 5fluorouracil and high-dose melphalan, by decreasing vascular delivery of these toxic agents.26 While it is out of the scope of this review to describe the management of oral mucositis, Table 3 provides the basic approach for the management of chemotherapy-mediated oral mucositis.27
Viral, fungal, and bacterial infections may also arise, with incidence depending on the use of prophylactic regimens, oral status prior to chemotherapy, and duration/severity of neutropenia. The frequency of infection decreases once the mucositis is resolved and the neutrophils have regenerated. Patients may remain at risk for infection, depending on the degree of immune recovery.28
ANTIESTROGEN THERAPY
Currently, there is scant evidence regarding the treatment of oral symptoms related to radiation treatment of the breast. While guidelines for dental care have been given for the pretreatment and chemotherapy phases of breast cancer treatment, little information is available about care for patients undergoing antiestrogen or hormonal therapies. The decrease in estrogen levels among post-menopausal women has been associated with reduced salivary flow unrelated to medications or periodontal diseases and tooth loss.29,30 Recently, aromatase inhibitors, which severely diminish estrogen levels, have been shown to impact periodontal health and increase levels of xerostomia among patients with breast cancer.31,32 Xerostomia can facilitate decreased salivary flow resulting in gingival bleeding and dental caries, and may be responsible for an increased prevalence of oral dysesthesia and alterations in taste sensation.29,30,33,34 Androgen deprivation therapy, used to treat prostate cancer, has been shown to negatively affect the periodontal health of some men.35 In addition, women using antiestrogen therapies may experience greater levels of depression, musculoskeletal symptoms, and fatigue, any of which may impact their abilities to achieve optimal oral hygiene. Dental hygienists should be aware of the potential changes in periodontal tissues and the risk of xerostomia and psychosocial implications in patients undergoing antiestrogen therapies.
CONCLUSION
Nearly 2.8 million women have been diagnosed with breast cancer.1 Oral complications of breast cancer treatments greatly affect quality of life both during the treatment and surveillance periods. Therefore, professional care and optimal self-care, ideally based on a pretreatment oral health assessment, can help ensure the best outcomes for patients fighting breast cancer.
REFERENCES
- Ries LAG, Young JL, Keel GE, Eisner MP, Lin YD,Horner MJ, eds. SEER Survival Monograph: Cancer Survival Among Adults: U.S. SEER Program, 1988-2001, Patient and Tumor Characteristics. National Cancer Institute, SEER Program, NIH Pub. No. 07-6215, Bethesda, Maryland: 2007.
- American Cancer Society. Causes, Risk Factors, andPrevention Topics. Available at: cancer.org/cancer/breastcancer/detailedguide/breast-cancer-riskfactors. Accessed October 16, 2015.
- American Cancer Society. Cancer Facts & Figures2013- 2014. Available at: cancer.org/cancer/breastcancer/detailedguide/breast-cancer-keystatistics. Accessed October 16, 2015.
- Anderson WF, Chatterjee N, Ershler WB, BrawleyOW. Estrogen receptor breast cancer phenotypes in the Surveillance, Epidemiology, and End Results database. Breast Cancer Res Treat. 2002;76:27–36.
- McPherson K, Steel CM, Dixon JM. ABC of breast diseases. Breast cancer-epidemiology, risk factors, and genetics. BMJ. 2000;321:624–628. Hamajima N, Hirose K, Tajima K, et al. Alcohol,tobacco and breast cancer–collaborative reanalysis of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067 women without the disease. Br J Cancer. 2002;87:1234–1245.
- Carlson RW, Allred DC, Anderson BO, et al. Invasive breast cancer. J Natl Compr Canc Netw. 2011;9:136–222.
- Carlson RW, Moench S, Hurria A, et al. NCCN TaskForce Report: breast cancer in the older woman. J Natl Compr Canc Netw. 2008;6(Suppl 4):S1–S25.
- Bedard PL, Cardoso F. Can some patients avoid adjuvant chemotherapy for early-stage breast cancer? Nat Rev Clin Oncol. 2011;8:272–279.
- EBCTCG. Effects of chemotherapy and hormonaltherapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687–1717.
- Piccart-Gebhart MJ. Adjuvant trastuzumab therapy for HER2-over expressing breast cancer: what we know and what we still need to learn. Eur J Cancer. 2006;42:1715–1719.
- Harvey JM, Clark GM, Osborne CK, Allred DC.Estrogen receptor status by immuno histochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol. 1999;17:1474–1481.
- Rastelli F, Crispino S. Factors predictive of response to hormone therapy in breast cancer. Tumori. 2008;94:370–383.
- Miller WR, O’Neill J. The importance of local synthesis of estrogen within the breast. Steroids. 1987;50:537–548.
- Burstein HJ, Griggs JJ. Adjuvant hormonal therapy for early-stage breast cancer. Surg Oncol Clin N Am. 2010;19:639–647.
- Korde LA, Zujewski JA, Kamin L, et al.Multidisciplinary meeting on male breast cancer: summary and research recommendations. J ClinOncol. 2010;28:2114–2122.
- Hayes S, Cornish B, Newman B. Comparison of methods to diagnose lymphoedema among breast cancer survivors: 6-month follow-up. Breast CancerRes Treat. 2005;89:221–226.
- Harris SR, Hugi MR, Olivotto IA, Levine M. Clinical practice guidelines for the care and treatment of breast cancer: 11. Lymphedema. CMAJ.2001;164:191–199.
- Epstein JB, Thariat J, Bensadoun RJ, et al. Oral complications of cancer and cancer therapy: from cancer treatment to survivorship. CA Cancer J Clin.2012;62:400–422.
- National Institute of Dental and Craniofacial Research. Three Good Reasons to See a Dentist BEFORE Cancer Treatment. Available at: nidcr.nih.gov/NR/rdonlyres/4FB39055-1788-4A9EADE6-FFBF2C1B6FE9/0/ThreeGoodReasons.pdf. Accessed October 16, 2015.
- Sonis ST, Woods PD, White BA. Oral complications of cancer therapies. Pretreatment oral assessment. NCI Monogr. 1990;9:29–32.
- National Institute of Dental and Craniofacial Research. Oral Complications of Cancer Treatment: What the Dental Team Can Do. Available at:nidcr.nih.gov/oralhealth/Topics/CancerTreatment/OralComplicationsCancerOral.htm. Accessed October 16, 2015.
- Hong CH, Allred R, Napenas JJ, et al. Antibiotic prophylaxis for dental procedures to prevent indwelling venous catheter-related infections. Am J Med. 2010;123:1128–1133.
- Sonis ST, Fey EG. Oral complications of cancertherapy. Oncology (Williston Park). 2002;16:680–686.
- Sonis ST. Oral mucositis in cancer therapy.J Support Oncol. 2004;2(Suppl 3):3–8.
- Rocke LK, Loprinzi CL, Lee JK, et al. A randomized clinical trial of two different durations of oral cryotherapy for prevention of 5-fluorouracilrelatedstomatitis. Cancer. 1993;72:2234–2238.
- National Institute of Dental and Craniofacial Research. Chemotherapy and Your Mouth. Available at:nidcr.nih.gov/oralhealth/Topics/CancerTreatment/ChemotherapyYourMouth.htm”.Accessed October 16, 2015.
- Hong CH, Napenas JJ, Hodgson BD, et al. A systematic review of dental disease in patients undergoing cancer therapy. Support Care Cancer.2010;18:1007–1021.
- Streckfus CF, Baur U, Brown LJ, et al. Effects of estrogen status and aging on salivary flow rates in healthy Caucasian women. Gerontology.1998;44:32–39.
- Wactawski-Wende J. Periodontal diseases and osteoporosis: association and mechanisms. Ann Periodontol. 2001;6:197–208.
- Taichman LS, Gomez G, Inglehart MR. Oral health-related complications of breast cancer treatment: assessing dental hygienists’ knowledgeand professional practice. J Dent Hyg. 2014;88:100–113.
- Taichman LS, Inglehart MR, Giannobile WV, et al.Periodontal health in women with early-stage postmenopausal breast cancer newly on aromataseinhibitors: a pilot study. J Periodontol. 2015;86:906–916.
- Lopez-Marcos JF, Garcia-Valle S, Garcia-Iglesias AA.Periodontal aspects in menopausal women undergoing hormone replacement therapy. Med Oral Patol Oral Cir Bucal. 2005;10:132–141.
- Mott AE, Grushka M, Sessle BJ. Diagnosis and management of taste disorders and burning mouth syndrome. Dent Clin North Am. 1993;37:33–71.
- Famili P, Cauley JA, Greenspan SL. The effect of androgen deprivation therapy on periodontal disease in men with prostate cancer. J Urol. 2007;177:921–924.
From Dimensions of Dental Hygiene. November 2015;13(11):54–56,59.



