Gingival Enlargement and Medication Use
In order to effectively address this type of gingival overgrowth, clinicians must be up to date on which drugs increase its risk.
This course was published in the September 2013 issue and expires September 2016. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the different types of drugs that may cause gingival enlargement.
- Identify the clinical features of gingival enlargement.
- Explain the etiology of and risk factors for drug-induced gingival enlargement.
- List the treatment options available for gingival enlargement.
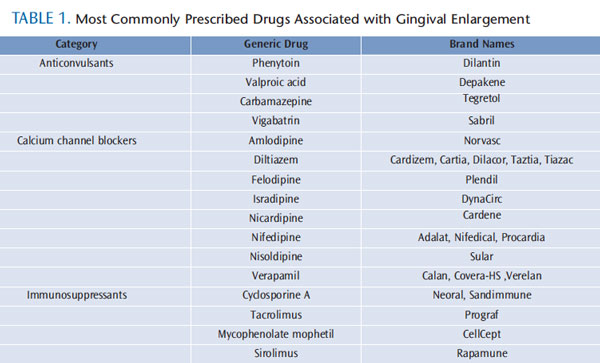
Gingival health can be negatively affected by bacteria, viruses, neoplasms, and certain drugs. Gingival enlargement, defined as an increase in the growth of the gingival tissue, raises the risk of infection, caries, and periodontal diseases, and negatively affects the esthetics of the smile. Initiated by both systemic and inflammatory factors, gingival enlargement is often caused by the use of commonly prescribed medications. These drugs—which can be divided into three categories: anticonvulsants, calcium channel blockers (CCBs), and immunosuppressants—promote changes in fibroblast function, which lead to an increase in the extracellular matrix of the gingival connective tissue (Table 1). In order to restore normal fibroblast function and gingival health, substitution of the offending drug by a medical provider is required. When substitution is not a feasible option, surgical excision of gingival tissue may provide temporary relief to patients affected by drug-induced gingival enlargement.
ANTICONVULSANTS

The discovery of the drug phenytoin in 1938 by Merritt and Putnam provided a major breakthrough in the management of patients with epilepsy around the world.1 Shortly after its introduction, however, reports linking phenytoin to gingival overgrowth began to surface.2 Susceptibility to this drug is not universal, as the prevalence of benign enlargement varies among population subsets. Gingival enlargement induced by anticonvulsants is significantly higher among children and institutionalized patients. For noninstitutionalized patients, the prevalence of gingival overgrowth caused by phenytoin is approximately 50%, and most often affects the maxillary anterior teeth (Figure 1).3 Gingival enlargement typically appears 2 months to 3 months after the first dose of phenytoin is taken, reaching its maximum severity approximately 12 months to 18 months later.
Since 1938, several anticonvulsant agents have been introduced to the market—including valproic acid, carbamazepine, phenobarbital, and vigabatrin—in an attempt to overcome the adverse effects of phenytoin. Cases of gingival enlargement have been noted with these agents as well, but such reports are rare and poorly documented. Due to its effectiveness in controlling convulsive seizure disorders, as well as its low cost and wide availability, phenytoin is still the drug of choice for the treatment of epilepsy—particularly grand mal, temporal lobe, and psychomotor seizures. Many patients are reluctant to substitute it with a new class of anticonvulsants, making it imperative that oral health professionals be aware of the increased risk of gingival enlargement associated with the use of phenytoin and prepared to address it in these patient populations.
CALCIUM CHANNEL BLOCKERS
CCBs are widely used for managing hypertension, angina, and supraventricular cardiac arrhythmias. This class derives its main therapeutic effects by preventing calcium ion influx through cell membranes. According to Intercontinental Medical Statistics Health Canada (a company that provides data, services, and technology to health care providers), CCBs rank eighth in prescription sales in the United States. Not all CCBs affect the gingiva in the same way. Nifedipine is the most frequently implicated CCB in drug-induced gingival overgrowth (Figure 2 through Figure 4).4
Lederman et al were first to report its negative oral effects in 1984, and subsequent studies showed that the prevalence of these adverse effects varied from 14% to 83%.5–7 The prevalence of negative gingival effects is significantly lower with verapamil and amlodipine—4.2% and 3.3%, respectively.8,9 Numerous reports have also associated gingival enlargement with the new generation of CCBs, such as felodipine, nicardipine, manidipine, and diltiazem. Gingival hyperplasia caused by CCBs is rarely seen in children, as these drugs are more commonly used in adult populations.
IMMUNOSUPPRESSANTS

Immunosuppressants reduce the incidence and severity of allograft rejection following the transplant of major organs (liver, pancreas, heart, and lung), as well as for the management of autoimmune conditions, such as rheumatoid arthritis. Cyclosporine A, since its discovery by Borel et al in 1977, has become the most commonly prescribed drug for the prevention of organ rejection.10 Cyclosporine A, however, can exert serious side effects that include: nephrotoxicity, induction of a diabetic state, chronic headaches, and disfiguring gingival enlargement (Figure 5). The first publication of gingival overgrowth was reported in kidney transplant patients 4 weeks to 6 weeks following the initial dose.11 The enlargement was more pronounced on the labial aspect of the gingiva, and was associated with significant bleeding. When teeth were surgically extracted, however, the enlargement was permanently eliminated. The prevalence of cyclosporine A-associated gingival enlargement has a very wide range—from 8% to 81%—with children and adolescents at the greatest risk.12,13
New immunosuppressant drugs, such as tacrolimus, mycophenolate mophetil, and sirolimus, have provided alternative options for managing organ transplant patients without the risk of gingival overgrowth.14
CLINICAL FEATURES

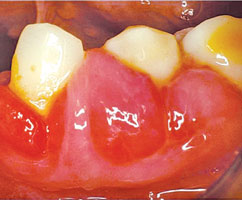
The oral manifestation of each type of drug-induced gingival enlargement is very similar, but is not a diagnostic factor. Keeping a detailed patient medical history will help dental professionals reach an accurate diagnosis. In their initial stages, lesions may appear as firm nodular enlargement of the interdental papillae, and can be located throughout the oral cavity. Gingival overgrowth more commonly affects the anterior region of the mouth, with greater pronouncement on the facial/buccal surfaces than the palatal/lingual surfaces.15 The enlargement may be localized or generalized, may affect the entire mouth, and can range from a mild increase of the interproximal gingival papillae to severe enlargement of both marginal and papillary tissues. In severe cases, the entire papillae and surrounding tissues are enlarged, giving the gingival tissues a lobulated appearance (Figure 6).
The enlargement may extend coronally and interfere with mastication and speech, and, in cases involving anterior teeth, create esthetic problems. Overgrown tissue creates pockets that harbor pathogenic bacteria beyond the reach of a toothbrush or dental floss. These negative changes impair optimal oral hygiene and can lead to an increased host susceptibility to oral infection, caries, and periodontal diseases.
Though these drugs do not directly affect the underlying alveolar bone, the gingival enlargement may become superimposed among patients with preexisting periodontitis, or patients may acquire it concomitantly. Gingival enlargement can present with different forms, ranging from noninflamed, firm, and fibrous gingiva to gingival tissue dominated by edema, erythema, and bleeding. The latter form is especially seen in patients with poor oral hygiene.
DIFFERENTIAL DIAGNOSIS

Drug-induced gingival overgrowth lacks a distinctive clinical marker to aid oral health professionals in reaching a proper diagnosis. These lesions mimic several pathologic conditions that manifest similarly. The enlargement may be localized, affecting one or few sites, or generalized—involving multiple sites. A localized gingival overgrowth may be caused by a periodontal abscess, a fibroma (benign tumor), or a pyogenic granuloma (tissue overgrowth caused by irritation, trauma, or hormonal fluctuations, such as experienced during pregnancy). The local nature of these lesions—along with the clinical signs and symptoms, and patient medical and dental history—help to differentiate them from gingival enlargement caused by medication use.
Generalized gingival enlargement poses a difficult diagnostic challenge in some patients. The most common factor involved in the majority of gingival enlargement is bacterial biofilm, which should be treated as plaque-induced gingival overgrowth via scaling and root planing coupled with good self-care. If the lesions persist 3 weeks to 4 weeks post-treatment, the patient should be referred to a health care provider in order to rule out systemic disease as a causative factor. Undiagnosed or poorly controlled diabetes is a major culprit, causing generalized inflammatory gingival enlargement and a significant amount of periodontal destruction.

Because patients with diabetes have impaired immunity, they are more susceptible to periodontal diseases. Other systemic diseases that may cause gingival enlargement include: acute leukemia, Wegener’s granulomatosis, and scurvy. Rapid gingival overgrowth accompanied by bleeding may indicate the presence of acute myeoblastic leukemia, chronic myeloid leukemia, acute lymphocytic leukemia, or chronic lymphocytic leukemia. Among patients diagnosed with acute myeloblastic leukemia, 5% experience gingival enlargement as the first complication.16,17 Leukemia is a malignant disease, and its successful resolution depends on early diagnosis and treatment.
Oral health professionals should refer patients to their medical professional when rapid progression of overgrowth is noted.16,17 In Wegener’s granulomatosis, the gingiva is swollen and bright red, with a granular surface described as “strawberry gums.” Differential diagnosis is suspected through this characteristic clinical manifestation, but it must be confirmed by biopsy. Scurvy, the result of vitamin C deficiency, is quite rare in developed countries, although occasional cases are still reported. Patients affected by this condition may experience severe gingival swelling and bleeding, accompanied by mobile teeth. Clinicians may rely on a high dosage of vitamin C and nonsurgical periodontal therapy to resolve gingival enlargement in this patient group.
Lastly, generalized overgrowth may be due to a rare genetic condition called hereditary gingival fibromatosis, characterized by a progressive enlargement of the gingiva. These cases usually require surgical intervention to remove the excess fibrotic gingival tissue, but recurrence of the lesions is unpredictable. The fibrotic nature of these lesions, along with the patient’s medical and family history, can differentiate them from drug-induced gingival overgrowth.
ETIOLOGY
The pathogenesis of drug-induced gingival enlargement is not fully understood. Although several mechanisms have been proposed over the years, there is a lack of consensus on this issue. The enlargement could be due to a reduction of collagen degradation by collagenase or the outcome of overproduction of extracellular ground substance.18,19 Other possible pathways are the presence of a subset of gingival fibroblasts “genetically susceptible” to these medications.20 Johnson et al have reported the synergistic effect of pro-inflammatory cytokines (IL-1b and IL-6) in enhancement of collagen synthesis by human gingival fibroblasts as another possible factor involved in this enlargement.21
RISK FACTORS

Bacterial biofilm is a common risk factor for all forms of inflammatory periodontal diseases, and its presence exacerbates drug-induced gingival enlargement. Other factors may include gender, with men at three times higher risk of developing gingival overgrowth than women.22 Patient age is inversely correlated with phenytoin-and cyclosporine A-induced gingival enlargement, as children and teenagers have a higher prevalence of these lesions than adults.23
In regard to dosage, there are conflicting reports of an association between the severity of enlargement and the daily intake of any of these drug classes. The majority of the reports have failed to detect a significant relationship between drug dosage and the severity of gingival enlargement.18
TREATMENT
The most effective treatment for drug-induced gingival enlargement is the withdrawal of the offending drug, which is then substituted with a class of medication that does not negatively affect the oral cavity. Medical providers may replace CCBs with beta blockers, diuretics, or angiotensinconverting enzyme inhibitors—none of which affect the oral tissues.

Phenytoin may be replaced by carbamazepine, ethosuximide, or sodium valproate. 24 Cyclosporine A can be substituted with tacrolimus. Despite these options, physicians and patients are often reluctant to switch to a different regimen, especially when the disease is well-controlled or other options have already been explored. If changing medications is not an option, some lesions may be managed nonsurgically. Mild lesions of CCB-induced gingival enlargement respond favorably to scaling and root planing and antimicrobial mouthrinses.
Good oral hygiene and self-care are pivotal in preventing further inflammation and maintaining the positive results achieved with dental care, including periodic nonsurgical periodontal therapy. As for phenytoin-induced enlargement, the gingival response to scaling and root planing is not as favorable due to the high content of collagen in the lesions, which prevents any significant tissue shrinkage.
Surgical excisions of the enlarged tissue by gingivectomy can eliminate the pseudopockets—restoring tissue architecture, appearance, and function. This procedure is performed with blades, surgical knives, and electrosurgery, or with a dental laser (Figure 7). The recurrence of drug-induced gingival enlargement has been reported in both surgical and nonsurgical methods—especially if cessation of the offending drug was not an option or was temporary.
Recurrence can occur as early as 3 months to 6 months following the surgical intervention, and affects as many as 40% of patients.25 Recurrence is more common among patients with poor oral hygiene and those without access to professional dental care (Figure 8).
SUMMARY
Drug-induced gingival enlargement is commonly seen among patients in the dental practice, and can be caused by a variety of medication classes. These lesions lack distinguishable clinical markers from plaque-associated lesions, and may be difficult to diagnose. A detailed medical history will help guide clinicians regarding the etiology, diagnosis, and available treatment options for patients with drug-induced enlargement of the gingiva.
REFERENCES
- Merritt HH, Putnam TJ. Landmark article Sept17, 1938: Sodium diphenyl hydantoinate in thetreatment of convulsive disorders. JAMA.1984;251:1062–1067.
- Kimball OP. The treatment of epilepsy withsodium diphenylhydantoinate. JAMA. 1939;112:1244–1245.
- Casetta I, Granieri E, Desidera M, et al.Phenytoin-induced gingival overgrowth: Acommunity-based cross-sectional study inFerrara, Italy. Neuroepidemiology. 1997;16:296–303.
- Butler RT, Kalkwarf KL, Kaldahl WB. Druginducedgingival hyperplasia: phenytoin,cyclosporin, and nifedipine. J Am Dent Assoc.1987;114:56–60.
- Lederman D, Lumerman H, Reuben S,Freedman PD. Gingival hyperplasia associatedwith nifedipine therapy. Report of a case. OralSurg Oral Med Oral Pathol. 1984;57:620–622.
- Barak S, Engelberg IS, Hiss J. Gingivalhyperplasia caused by nifedipine.Histopathologic findings. J Periodontol.1987;58:639–642.
- Fattore L, Stablein M, Bredfeldt G, Semla T,Moran M, Doherty-Greenberg JM. Gingivalhyperplasia: a side effect of nifedipine anddiltiazem. Spec Care Dentist. 1991;11:107–109.
- Miller CS, Damm DD. Incidence of verapamilinducedgingival hyperplasia in a dentalpopulation. J Periodontol. 1992;63:453–456.
- Jorgensen MG. Prevalence of amlodipinerelatedgingival hyperplasia. J Periodontol.1997;68:676–678.
- Borel JF, Feurer C, Magnée C, Stähelin H.Effects of the new anti-lymphocytic peptidecyclosporin A in animals. Immunology.1977;32:1017–1025.
- Rateitschak-Plüss EM, Hefti A, Lörtscher R,Thiel G. Initial observation that cyclosporin-Ainduces gingival enlargement in man. J ClinPeriodontol. 1983;10:237–246.
- Friskopp J, Klintmalm G. Gingivalenlargement. A comparison betweencyclosporine and azathioprine treated renalallograft recipients. Swed Dent J. 1986;10:85–96.
- Pernu HE, Pernu LM, Huttunen KR,Nieminen PA, Knuuttila ML. Gingival overgrowthamong renal transplant recipients related toimmunosuppressive medication and possiblelocal background factors. J Periodontol.1992;63:548–553.
- Keown PA. New immunosuppressivestrategies. Curr Opin Nephrol Hypertens. 1998;7:659-663.
- Marshall RI, Bartold PM. A clinical review ofdrug-induced gingival overgrowth. Aust Dent J.1999;44:219–232.
- Demirer S, Ozdemir H, Sencan M,Marakoglu I. Gingival hyperplasia as an earlydiagnostic oral manifestation in acutemonocytic leukemia: a case report. Eur J Dent.2007;1:111–114.
- Wu J, Fantasia JE, Kaplan R. Oralmanifestations of acute myelomonocyticleukemia: a case report and review of theclassification of leukemias. J Periodontol.2002;73:664–668.
- Barclay S, Thomason JM, Idle JR, SeymourRA. The incidence and severity of nifedipineinducedgingival overgrowth. J Clin Periodontol.1992;19:311–314.
- Lucas RM, Howell LP, Wall BA. Nifedipineinducedgingival hyperplasia. A histochemicaland ultrastructural study. J Periodontol.1985;56:211–215.
- Pernu HE, Knuuttila MLE, Huttenen KRH,Tiilikainen ASK. Drug-induced gingivalovergrowth and class I1 majorhistocompatibility antigens. Transplantation.1994;57:1811:13.
- Johnson RB, Zebrowski EJ, Dai X. Synergisticenhancement of collagenous protein synthesisby human gingival fibroblasts exposed tonifedipine and interleukin-1-beta in vitro. J OralPathol Med. 2000;29:8–12.
- Ellis JS, Seymour RA, Steele JG, RobertsonP, Butler TJ, Thomason JM. Prevalence ofgingival overgrowth induced by calciumchannel blockers: a community based study.J Periodontol. 1999;70:63–67.
- Daley TD, Wysocki GP, Day C. Clinical andpharmacologic correlations in cyclosporineinducedgingival hyperplasia. Oral Surg OralMed Oral Pathol. 1986;62:417–421.
- Seymour RA, Smith DG, Turnbull DN. Theeffect of phenytoin and sodium valproate onthe periodontal health of adult epilepticpatients. J Clin Periodontol. 1985;12:413–419.
- Ilgenli T, Atilla G, Baylas H. Effectiveness ofperiodontal therapy in patients with druginducedgingival overgrowth. Long-term results.J Periodontol. 1999;70:967–972.
From Dimensions of Dental Hygiene. September 2013; 11(9): 51–55



