Strategies for Effective Interpretation of Radiographs
Redefining diagnostic skills and refreshing their knowledge of anatomy will help dental hygienists recognize the most common variations in normal radiographs, as well as the most frequently encountered incidental findings.
This course was published in the September 2013 issue and expires September 2016. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the classifications of findings in dental radiography.
- List the factors that affect a clinician’s ability to make a diagnosis through dental radiography.
- Identify the most frequently should encountered findings in dental radiographs.
The views expressed in this article are those of the authors and do not reflect the official policy of the United States Air Force, the US Department of Defense, or the US Government.
Oral radiology has transformed the practice of dentistry and broadened the horizons of all dental specialties, molding the dental profession into an ever-changing, dynamic field. Clinicians must refine their diagnostic skills and general knowledge of anatomy in order to recognize the most common variations of normal in dental radiographs, as well as the most frequently encountered incidental findings.
CLASSIFICATIONS

In general, findings in dental radiographs are classified as radiolucent, radiopaque, or mixed density—depending on their appearance when compared to the adjacent bone. One of the most common clinical observations seen among radiolucent lesions is the pericoronal radiolucency around unerupted teeth. The majority of these cases represent hyperplastic dental follicles. Patient age, degree of root formation, size of the follicle, and tooth location are important factors when forming a differential diagnoses for a pericoronal radiolucency.
The width of the follicular space is dependent on the radiographic modality used. Differences in technique and the geometry of an X-ray beam between the panoramic and the intraoral radiation units must also be taken into account.
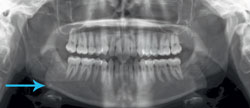
Panoramic imagery is magnified 20% to 25%, and is notorious for distortion. Intraoral imagery has about 4% magnification, but it can be affected by a variety of technicalities related to placement of the sensor and angulation of the X-ray beam. Anatomical features can alter the perception of the viewer and mimic pathology, as well. When a pericoronal space of an unerupted tooth is greater than 5 mm and the roots are fully formed, the lesion is most likely a dentigerous cyst or other odontogenic cyst, rather than a hyperplastic dental follicle (Figure 1). Some lesions appear completely radiolucent, while a small number present with a residual trabecular pattern of bone within the lesion.
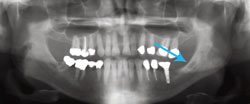
A notable example of this finding is the focal osteoporotic bone marrow defect (Figure 2). This lesion is usually diagnosed with panoramic radiographs, and is often found in previous extraction sites. Radiographically, it appears as an ill-defined but localized radiolucency and, therefore, may be confused with an intraosseous neoplasm. Careful evaluation of periapical radiographs often reveals fine central trabeculations.
A few cases have been associated with pain and swelling, although most are found in the posterior mandible of women age 40 and older.1–3 An osteoporotic bone marrow defect may represent aberrant bone regeneration after tooth extraction, or it may suggest bone marrow hyperplasia in cases where increased demand of erythrocytes is noted. While the radiographic findings are suggestive of a diagnosis, incisional biopsy is necessary to rule out other potentially serious conditions. Microscopically, normal hematopoietic or fibro-fatty marrow is observed. After establishing the diagnosis, no further treatment is indicated.
STAFNE DEFECTS
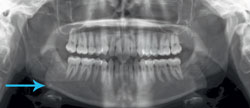
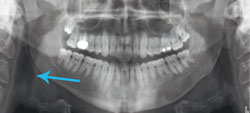
In certain circumstances, the location of radiolucencies provides important clues regarding the diagnosis—as is the case for Stafne defects, which are characteristically located unilaterally in the posterior region of the mandible, between the mandibular angle and the third molar, and below the inferior alveolar canal (Figure 3). First reported by Edward C. Stafne, DDS, in 1942,4 these radiolucencies are often found unexpectedly on panoramic radiographs. The distinctive location of this radiolucency is often highly suggestive of the diagnosis. Complementary techniques, such as cone beam-computed tomography or an occlusal radiograph, aid in establishing the diagnosis.

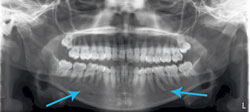
Stafne defects are asymptomatic lingual bone depressions of the mandible (Figure 4). The pathogenesis is still unknown, although it is widely believed these concavities develop due to localized pressure resorption of the lingual surface of the mandible from adjacent salivary gland tissue.5 Once evidence of a depression of the lingual cortex is obtained through additional radiographs, the diagnosis is established with radiographic means; typically, no surgery is indicated. If the area is biopsied, microscopic benign salivary gland or fibrovascular connective tissue is found. Stafne defects can be bilateral in rare cases, and an anterior variant has also been described. Diagnosing an anterior Stafne defect can be challenging, and it should always be part of the differential diagnosis for a radiolucent lesion of the anterior mandible.
RADIOPACITIES
Radiopacities are generally considered benign—with few exceptions—and are classified as homogenously radiopaque (Figure 5), or radiopacities with a surrounding radiolucent halo (Figure 6). Focal areas of radiopacity within the jaws, but without surrounding radiolucent halos, are common incidental findings. Studies estimate the prevalence of radiopacities to be between 5.4% and 6.1%,6,7 with the most common location being the posterior mandible in the molar region.7,8 These areas of radiopacity are not unique to the jaws. Similar lesions have been found in other bones. In the absence of any inflammatory cause or other identifiable pathology, these radiopaque foci are termed idiopathic osteosclerosis—or dense bone island (Figure 5). Similar lesions resulting from a pulpal inflammatory process are called condensing osteitis (Figure 7).


ANTRAL PSEUDOCYSTS
Antral pseudocysts are common incidental findings on panoramic radiographs, and affect 1.4% to 9.6% of the general population.9–11 Characteristically presenting as a dome-shaped radiopacity on the floor of the maxillary sinus (Figure 8), these lesions are generally asymptomatic and do not require surgical treatment. These sessile soft tissue elevations of the floor of the maxillary sinus are caused by the accumulation of inflammatory exudates, surrounded by loose connective tissue. The fluid is located between the bony floor and the sinus mucosa.12 The inflammatory trigger may be related to a sinus infection or allergy, although many cases arise secondary to odontogenic inflammation of the adjacent teeth. Therapy focuses on eliminating all foci of odontogenic infection in the area. In the absence of odontogenic-related inflammation, no treatment is necessary, unless significant symptoms are noted. Because antral pseudocysts typically do not require intervention, proper recognition is necessary to avoid overtreatment.
SIALOLITHS
Occasionally, calcified structures superimpose the ramus or the body of the mandible, a condition known as sialoliths—or calcified structures that develop within the salivary ductal system. The prevalence in the general population is approximately 1% (Figure 9).13,14 Theoretically, sialoliths arise from deposition of calcium salts around a nidus of debris within the duct lumen.15 Most salivary stones are found in the submandibular gland, and appear as radiopaque masses—typically superimposed over the mandible, which warrants careful evaluation and, in some cases, additional radiographs so as not to be confused with intrabony pathology.16 Occasionally, a concentric pattern of calcification is radiographically evident in well-calcified sialoliths. Obstruction of the excretory ducts of the salivary glands is common among patients with sialoliths, with episodic pain and swelling—especially around meal times—being regular complaints. For this reason, removal of the calcified structure is indicated,17 as obstruction of the major salivary glands is associated with chronic sialadenitis. In addition, the inability of the salivary gland secretions to flush out the excretory ductal system favors the retrograde bacterial colonization from the oral flora into the excretory ducts, which may result in the development of acute sialadenitis that may produce acute symptoms and purulent discharge from the gland.


TONSILLITHS
Dystrophic calcifications in the tonsils are called tonsilliths or tonsilloliths (Figure 10). The pharyngeal tonsils have numerous deep, epitheliumlined crypts, which provide greater surface area for interaction between the oral environment and the underlying lymphoid tissue. In some patients, these crypts become engorged with desquamated epithelial cells or debris that obstructs the crypts. If these plugs remain for extended periods, they typically undergo calcification. Tonsilliths are easily misinterpreted on panoramic radiographs because they cast radiopaque shadows over the middle portion of the ascending mandibular ramus. Therefore, tonsillolithiasis should be kept in mind during the differential diagnoses of radiopaque lesions in this region. Tonsilliths are a common incidental finding in clinical practice,18 and usually are of little clinical significance.19 Those tonsilliths that achieve large size, however, may result in oral malodor, sensation of a lump in the throat, dysgeusia, sore throat, or dysphagia.19,20 The most common radiographic presentation is that of a cluster of distinct radiopacities superimposed over the ramus of the mandible. Single large lesions have been described.21,22 A few cases have been bilateral,23 with most cases being asymptomatic. Tonsilliths, which are typically discovered during evaluation of a panoramic radiograph, can present in patients of all ages and generally affect men more frequently than women. The condition often does not warrant treatment, unless associations with significant tonsillar hyperplasia, or clinical symptoms of acute or chronic tonsillitis, are present.
ODONTOMAS
Odontomas are some of the most common odontogenic lesions encountered in clinical practice (Figure 6). Typically, odontomas are identified as incidental findings when a radiograph is exposed in an area where a tooth has failed to erupt.24,25 Defined as odontogenic neoplasms in the current World Health Organization classification, odontomas likely represent hamartomas found in the jaw, rather than true neoplasms.26 Odontomas are usually associated with the coronal aspect of an unerupted tooth, presenting as amorphous radiopacities with similar radiodensity when compared to enamel or dentin. The presence of a thin, radiolucent halo surrounding the radiopacity is an important diagnostic finding (Figure 6). There are two subtypes of odontomas: the complex and the compound, distinguished by the variable organization of the radiopacity.25 Complex odontomas typically appear in the posterior mandible or maxilla, and are amorphous radiopacities without morphologic resemblance to a tooth. Compound odontomas are more common in the anterior maxilla, and are typically composed of multiple tooth-like structures with a close morphologic resemblance to small misshapen teeth (Figure 6).
STYLOHYOID COMPLEX
The calcified stylohyoid ligament (Figure 11) is commonly seen in the panoramic image as part of the stylohyoid complex—a combination of the calcified stylohyoid ligament and/or elongation of the styloid process.27 The stylohyoid complex is a radiopacity that superimposes the soft tissue of the ear, and is seen as a single, real image on the lateral edges of the panoramic image. Unlike the cervical spine, which is sometimes seen on both sides and in the center of the panoramic image, there is only one spine. When the calcified stylohyoid complex is visualized, it is bilaterally calcified—sometimes in thick segments—or partially calcified in thin, tapered segments that skip down to the lesser horn of the hyoid bone. Literature widely discusses the calcified stylohyoid complex, and its role in eagle syndrome and styloid carotid artery syndrome. Not everyone with a calcified stylohyoid complex, however, is symptomatic. Discovery of a calcified stylohyoid complex on a panoramic image should prompt the clinician to ask the patient about pain, followed by evaluation for other clinical findings associated with these syndromes.
CONCLUSION
Diagnostic imaging may present challenges in deciphering normal and incidental radiographic findings. Acquired knowledge—through literature and experience—is helpful in determining a correct diagnosis, which is vital to the oral health of patients. Clinicians are responsible for reviewing the entire panoramic image, and, when anomalies are detected, must determine the course of action. For this reason, proper technique and patient cooperation are crucial during diagnostic imaging to ensure intraoral and panoramic radiographs are accurate and free of imposition.
REFERENCES
- Barker BF, Jensen JL, Howell FV. Focalosteoporotic bone marrow defects of the jaws.An analysis of 197 new cases. Oral Surg Oral Med Oral Pathol.1974;38:404–413.
- Standish SM, Shafer WG. Focal osteoporotic bone marrow defects of the jaws. J Oral Surg Anesth Hosp Dent Serv.1962;20:123?128.
- Crawford BE, Weathers DR. Osteoporotic marrow defects of the jaws. J Oral Surg. 1970;28:600?603.
- Stafne EC. Bone cavities situated near the angle of the mandible. J Am Dent Assoc.1942;29:1969?1972.
- Grellner TJ, Frost DE, Brannon RB. Lingual mandibular bone defect: report of three cases.J Oral Maxillofac Surg. 1990;48:288?296.
- Geist JR, Katz JO. The frequency and distribution of idiopathic osteosclerosis. OralSurg Oral Med Oral Pathol. 1990;69:388?393.
- Yonetsu K, Yuasa K, Kanda S. Idiopathic osteosclerosis of the jaws: panoramic radiog raphic and computed tomographic findings. Oral Surg Oral Med Oral Pathol OralRadiol Endod. 1997;83:517?521.
- McDonnell D. Dense bone island. A review of 107 patients. Oral Surg Oral Med OralPathol. 1993;76:124?128.
- Bohay RN, Gordon SC. The maxillary mucous retention cyst: a common incidental panoramic finding. Oral Health. 1997;87:7?8,10.
- MacDonald-Jankowski DS . Mucosal antralc ysts observed within a London inner-city population. Clin Radiol. 1994;49:195?198.
- Hadar T, Shvero J, Nageris BI, Yaniv E.Mucus retention cyst of the maxillary sinus:the endoscopic approach. Br J Oral Maxillofac Surg. 200;38:227?229.
- Mardinger O, Manor I, Mijiritsky E, Hirshberg A. Maxillary sinus augmentation in the presence of antral pseudocyst: a clinical approach. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:180?184.
- Brown JE. Interventional sialography and minimally invasive techniques in benign salivary gland obstruction. Semin Ultrasound CT MR. 2006;27:465?475.
- Escudier MP, McGurk M. Symptomatic sialoadenitis and sialolithiasis in the English population, an estimate of the cost of hospital treatment. Br Dent J. 1999;186:463?466.
- Khosla E, Kurian J, Kuriakose S. Salivary calculus: an insight into its pathogenesis–acase report of parotid sialolith in a 9 year old child. J Indian Soc Pedod Prev Dent.1999;17:122?125.
- Bamgbelu O. A giant submandibular sialolith: management and complications. Dent Update. 1989;16:399?400.
- Boffano P, Gallesio C . Surgical treatment o fa giant sialolith of the Wharton duct. J Craniofac Surg. 2010;21:134?135.
- Aghdasi MM, Valizadeh S , Amin-Tavakoli N,Bakhshandeh H. Tonsilolith in routine panoramic radiographs; is it a common incidental finding? Iran J Radiol.2012;9:109?110.
- Pruet CW, Duplan DA. Tonsil concretions and tonsilloliths. Otolaryngol Clin North Am.1987;20:305?309.
- Neshat K, Penna KJ, Shah DH. Tonsillolith: a case report. J Oral Maxillofac Surg.2001;59:692?693.
- Silvestre-Donat FJ, Pla-Mocholi A, Estelles-Ferriol E, Martinez-Mihi V. Giant tonsillolith:report of a case. Med Oral Patol Oral Cir Bucal.2005;10:239?242.
- Padmanabhan TK, Chandra Dutt GS,Vasudevan DM, Vijayakumar. Giant tonsillolith simulating tumour of the tonsil–a case report. Indian J Cancer. 1984;21:90?91.
- Ozcan E, Ural A, Oktemer TK, Alpaslan G.Bilateral tonsillolithiasis: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e17?18.
- Kulkarni VK, Deshmukh J, Banda NR,Banda VR. Odontomas—silent tormentors ofteeth eruption, shedding and occ usion. BMJ Case Rep. 2012;12:2012.
- Boffano P, Zavattero E, Roccia F, Gallesio C .Complex and compound odontomas. J Craniofac Surg. 2012;23:685?688.
- White S, Pharoah M, eds. Oral Radiology: Principles and Interpretation. 6th ed. St. Louis: Mosby; 2009.
- Gokce C , Sisman Y, Sipahioglu M. Styloid process elongation or eagle syndrome: is there any role for ectopic calcification? Eur J Dent. 2008;2:224?228.
From Dimensions of Dental Hygiene. September 2013; 11(9): 56. 59–62



