
A Cost-Effective Solution for Dental Caries Treatment
Silver diamine fluoride offers a practical, affordable, and minimally invasive option to arrest dental caries.
This course was published in the March 2024 issue and expires March 2027. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 010
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the significance of untreated dental caries and its impact on various populations, especially those with limited access to dental care due to socioeconomic factors.
- Discuss the mechanism of action of silver diamine fluoride (SDF) in arresting dental caries, including its antimicrobial properties and remineralization effects.
- List the research demonstrating the efficacy of SDF and note contraindications to its use.
Dental caries is one of the most prevalent chronic diseases in the United States.1 Despite continuous efforts, such as increases in funding and the number of oral health professionals, the prevalence of dental caries still remains high. In 2016, 45.8% of youth aged 2 to 19 had experienced caries, while 13% had untreated caries.2 Untreated dental caries in permanent teeth is also one of the most common health conditions among adults in low, middle, and even economically developed countries.2
Caries is often left untreated, especially in low-income regions, due to financial burdens and barriers to accessing professional dental care.1 This lack of treatment can result in further issues, such as negative impacts on quality of life and systemic health.
Because cost is a barrier to dental care, affordable treatments should be implemented. Silver diamine fluoride (SDF) is one of these options, providing a practical, affordable, and minimally invasive option for the arrest of caries.2 All 50 states allow dental hygienists to administer SDF, with restrictions based on each state.3,4
Cost-Effective Option
In traditional restorative therapy, dental handpieces are used, tooth structure is altered, and patients leave with a new form of the tooth they once had. Some populations are able to afford these costly dental treatments; however, not all individuals have the ability to absorb these costs.
Patient populations that often struggle to access dental treatment include, but are not limited to: children, people with intellectual and developmental disabilities (IDD), older adults, those with physical impairments, patients from low socioeconomic regions, and minority patients.5 These populations may experience more difficulty accessing dental care due to transportation issues, cost, lack of insurance, absence of providers who treat patients with disabilities, and reduced knowledge of the importance of primary teeth.6–8 Patients with these limitations may prolong or neglect recommended dental treatment.
Traditional restorative approaches may not always be financially, mentally, or physically possible. SDF is a cost-effective option, as preliminary models suggest that SDF could eliminate 80% of caries and cost less than 20% of the current Medicaid children’s oral health spending.2 Although the implementation of SDF cannot fix the systemic issues within low-income communities, it can provide a more affordable approach to treatment.5
SDF may reduce the burden of untreated dental caries in various populations.9 SDF provides a more equitable yet effective alternative to people in populations struggling to afford more costly treatments such as composite restorations.10 Low-income individuals or the uninsured may want to consider SDF. Additionally, state funding programs may make applying SDF even more affordable for vulnerable patients.11
SDF can serve as a temporary fix while patients await a dental appointment, especially in the public health field, where wait times may be extensive.12 Additionally, SDF may be the best option for people with IDD who have difficulty receiving dental care.
Mechanism of Action
In the 1960s, Nishino and Yamaga13,14 developed the first SDF product by combining the actions of fluoride and silver. They discussed the effects of SDF on prevention and cessation of the dental caries progression, as well as SDF’s desensitization properties.
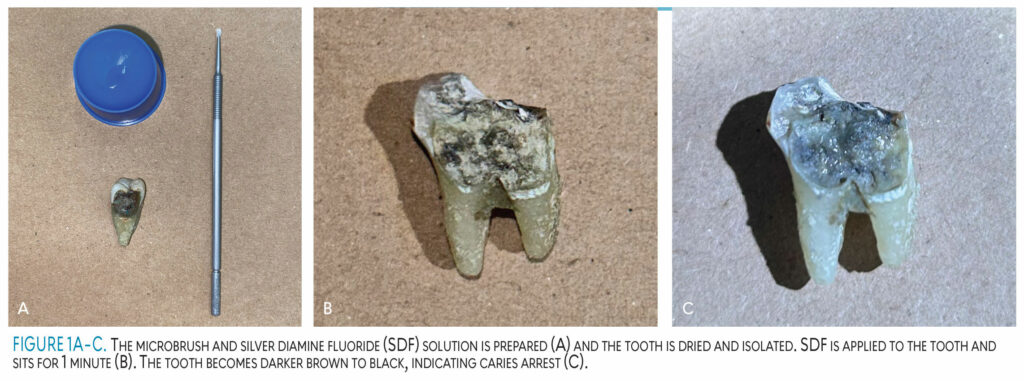
SDF is a painless, minimally invasive solution that is able to arrest caries from progressing further. SDF contains silver, ammonia, and fluoride. The silver acts as an antimicrobial agent, the fluoride remineralizes the tooth structure, and the ammonia stabilizes the reaction. The products yielded in this solution are silver phosphate and silver oxide, which result from the contact of hydroxyapatite crystals.2,15,16 Once the tooth is dried and isolated, the solution is applied to the tooth for 1 minute. When this colorless solution contacts the tooth, it becomes darker brown to black and arrests caries immediately, preventing it from becoming a larger problem (Figure 1).15,17,18
 One meta-analysis investigated the effects of SDF on cariogenic bacteria and dental hard tissues.19 Eleven studies found that SDF was bactericidal to cariogenic bacteria, including Streptococcus mutans, and effectively inhibited the growth of cariogenic biofilms on dentition. Twenty-nine studies reported the remineralization of demineralized enamel or dentin by SDF and found that after SDF treatment, demineralization of enamel or dentin was reduced.
One meta-analysis investigated the effects of SDF on cariogenic bacteria and dental hard tissues.19 Eleven studies found that SDF was bactericidal to cariogenic bacteria, including Streptococcus mutans, and effectively inhibited the growth of cariogenic biofilms on dentition. Twenty-nine studies reported the remineralization of demineralized enamel or dentin by SDF and found that after SDF treatment, demineralization of enamel or dentin was reduced.
After the application of SDF on caries lesions, a highly mineralized surface rich in calcium and phosphate is formed. Four studies examined the effects of SDF on dentin collagen and found that SDF inhibited collagenase and protected dentin collagen from destruction. This concise review concluded that SDF is a bactericidal agent that reduces cariogenic bacteria, inhibits demineralization, promotes remineralization, and hinders the degradation of dentin collagen.19
SDF (38%) is able to arrest dental caries and reduce bacteriral colony-forming units (CFOs), such as Streptococcus mutans and Actinomyces naeslundii.20 The reduction of CFOs gives this solution an antimicrobial function, which can help to combat oral bacteria. SDF also increases the rate of calcium absorption, helping to prevent tooth decay.20 Those surfaces treated with SDF have a greater microhardness in previously cavitated lesions than those surfaces not treated with SDF.21
The antimicrobial properties of SDF have been shown to be effective against certain bacteria, such as lactobacillus.18 The antimicrobial aspects inhibit replication of bacterial DNA and biofilm formation by binding to bacterial cellular components and influencing enzymes related to both carbohydrate metabolism and sugar uptake. In addition, matrix metalloproteinases (MMPs) and cathepsins (CCs) are proteolytic enzymes that contribute to dentin and collagen degradation as well as caries progression. MMPs and CCs are also inhibited by SDF, decreasing caries risk.18 SDF also has remineralization effects on enamel and dentin caries. A chemical reaction between SDF and hydroxyapatite creates silver phosphate and calcium fluoride, which then elevates the pH and formation of fluoride reservoirs.
Effectiveness and Safety
Current research indicates SDF, especially at a 38% solution, is effective in the arrest of caries.5,15,18,20 SDF works among all age groups: children, adults, and elderly patients.2,15,22 Additionally, SDF meets the US Institute of Medicine’s six quality aims: safe, effective, efficient, timely, patient centered, and equitable.5,23
Research demonstrates the effectiveness of SDF in arresting caries and remineralizing tooth structure.15,19 Additionally, SDF has been shown to treat root caries and aid in desensitization, providing relief to patients who experience pain from eating sugary, hot, or cold foods and overall occlusal pressure with chewing.5,19
The effectiveness and safety of 38% SDF to arrest caries lesions in preschool children has also been researched.9 In this study, 72% of caries lesions treated with SDF were successfully arrested, while only 5% of caries lesions treated with the blue-tinted placebo were arrested.9 The results found that SDF may help to reduce the burden of untreated tooth decay in the studied population.
Early childhood caries has become more prevalent, especially in populations with low socioeconomic status.24 Children may benefit the most from SDF treatment due to primary carious teeth that require short-term treatment.5,22 The largest school-based intervention in the US proved that SDF was successful in preventing and arresting dental caries.25
SDF can also be very helpful for rural and urban areas with reduced access to dental care.5 Those with dental anxiety may also benefit because SDF is minimally invasive and completely painless.2 The American Dental Association (ADA) concluded that SDF is a cost- and clinically effective treatment to aid in the arrest of dental caries.16
SDF was cleared by the US Food and Drug Administration (FDA) for its desensitizing properties in 2014.5,15,16,23 The FDA also recommended a semi-annual application for sustained benefit, especially with lesions located in primary teeth. SDF also reduces caries lesions adjacent to teeth that have already received SDF application. SDF was overall more effective when applied once per year than traditional sodium fluoride, which is generally applied twice per year.16
Contraindications
Oral health professionals should be aware of contraindications to using SDF prior to recommending the treatment. These contraindications include but are not limited to pregnancy, allergies to silver, significant desquamative gingivitis, peri-implant mucositis, restorations or caries in the esthetic zone, and both clinical and radiographic signs or symptoms of periapical pathology.18
One consistent drawback to SDF is the dark discoloration due to the precipitation of silver byproducts in the dental tissues.5,15 Though its darker brown to black color is not ideal for the anterior portions of tooth structure, it can be used on most surfaces of dentition, especially in posterior regions.18,22
SDF can be used on surfaces similar to amalgam restoration sites, where esthetics are not a concern. However, with the proper education and consent, it can be used anteriorly. Parents and caregivers of children should be educated on the benefits of SDF on primary teeth, as opposed to restorations due to children eventually losing their primary teeth. This cost-effective option may help prevent children’s permanent teeth from developing caries.
Clinicians should be careful to apply SDF directly on tooth surfaces while avoiding the gingiva, mucosa, and skin due to staining.14,16 Clinicians can protect the gingiva from staining by applying petroleum jelly.17,22,23
Conclusion
Evidence-based research has found 38% SDF to be a successful, minimally invasive treatment in arresting dental caries and is recommended by the ADA.2,5,9,16,18-20,25 Awareness of SDF should be more widespread as an effective option to arrest dental caries, for all ages and populations, especially those that lack the funds needed to obtain dental care. SDF can be an additional resource for many different populations, such as those with limited financial means, patients with dental anxiety, older adults at risk for root caries, and children who still have their primary dentition.
References
- World Health Organization. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030. Available at: who.int/publications/i/item/9789240061484. Accessed February 27, 2024.
- Bridge G, Martel AS, Lomazzi M. Silver diamine fluoride: transforming community dental caries program. Int Dent J. 2021;71:458–461.
- American Dental Hygienists’ Association. State Specific Information on Silver Diamine Fluoride. Available at: adha.org/wp-content/uploads/2022/12/Silver_Diamine_Fluoride_State_by_State_Information.pdf. Accessed February 27, 2024.
- Oral Health Workforce Research Center. Application of Silver Diamine Fluoride (SDF) by Dental Hygienists. Available at: oralhealthworkforce.org/silver-diamine-fluoride-SDF. Accessed February 27, 2024.
- Crystal YO, Niederman R. Evidence-based dentistry update on silver diamine fluoride. Dent Clin North Am. 2019;63:45–68.
- Hansen C, Curl C, Geddis-Regan A. Barriers to the provision of oral health care for people with disabilities. BDJ In Pract. 2021;34:30-34.
- Vujicic M, Buchmueller T, Klein R. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Aff. 2016;35:2176-2182.
- Liu HY, Chen JR, Hsiao SY, Huang ST. Caregivers’ oral health knowledge, attitude and behavior toward their children with disabilities. J Dent Sci. 2017;12:388-395.
- Milgrom P, Horst JA, Ludwig S, et al. Topical silver diamine fluoride for dental caries arrest in preschool children: A randomized controlled trial and microbiological analysis of caries associated microbes and resistance gene expression. J Dent. 2018;68:72–78.
- Nguyen TM, Tonmukayakul U, Hall M, Calache H. Cost-effectiveness analysis of silver diamine fluoride to divert dental general anaesthesia compared to standard care. Aust Dent J. 2022;67:352-361.
- Johnson B, Serban N, Griffin PM, Tomar SL. Projecting the economic impact of silver diamine fluoride on caries treatment expenditures and outcomes in young US children. J Public Health Dent. 2019;79:215-221.
- Northridge M, Kumar A, Kaur R. Disparities in access to oral health care. Annu Rev Public Health. 2020;41:513–35.
- Yamaga R, Nishino M, Yoshida S, Yokomizo I. Diammine silver fluoride and its clinical application. J Osaka Univ Dent Sch. 1972;12:1–20.
- Nishino M, Yoshida S, Sobue S, Kato J, Nishida M. Effect of topically applied ammoniacal silver fluoride on dental caries in children. J Osaka Univ Dent Sch. 1969:149–55.
- Burgess JO, Vaghela PM. Silver diamine fluoride: a successful anticarious solution with limits. Adv Dent Res. 2018;29:131–134.
- American Dental Association. Silver Diamine Fluoride. Available at: ada.org/resources/research/science-and-research-institute/oral-health-topics/silver-diamine-fluoride. Accessed February 27, 2024.
- MacLean J. A practical guide to silver diamine fluoride. Available at: dimensionsofdentalhygiene.com/eLookbook/2020/elevate/pratical-guide-silver-diamine-fluoride.html. Accessed February 27, 2024.
- Greenwall-Cohen J, Greenwall L, Barry S. Silver diamine fluoride – an overview of the literature and current clinical techniques. Br Dent J. 2020;228:831–838.
- Zhao IS, Gao SS, Hiraishi N, et al. Mechanisms of silver diamine fluoride on arresting caries: a literature review. Int Dent J. 2018;68:67–76.
- Jabin Z, Vishnupriya V, Agarwal N, Nasim I, Jain M, Sharma A. Effect of 38% silver diamine fluoride on control of dental caries in primary dentition: a systematic review. J Family Med Prim Care. 2020;9:1302–1307.
- Chu CH, Lo ECM, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002;81:767-770.
- Aly M, Yousry Y. Potential discolouration of silver diamine fluoride versus silver diamine fluoride/potassium iodide in primary teeth: a randomised clinical study. Br Dent J. 2022;1–6.
- Mei M, Lo EM, Chu CH. Clinical use of silver diamine fluoride in dental treatment. Compend Contin Educ Dent. 2016;37:93–98.
- Anil S, Anand P. Early childhood caries: prevalence, risk factors, and prevention. Front Pediatr. 2017;5:157.
- Harrison R. School dental program prevents 80 percent of cavities with one-time, non-invasive treatment. Available at:nyu.edu/about/news-publications/news/2023/february/school-dental-program-prevents-80-percent-of-cavities.html#:~:text=CariedAway%20is%20a%20randomized%20trial,ionomer%20sealants%20and%20fluoride%20varnish. Accessed February 27, 2024.
From Dimensions of Dental Hygiene. March 2024; 22(2):28-31



