
Explore the Interplay Between Periodontal Infections and Systemic Health
A better understanding of this association can help improve patient care and health outcomes.
This course was published in the March 2024 issue and expires March 2027. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 490
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the multifactorial nature of periodontal diseases, including the roles of bacterial infections, host inflammatory responses, and associated risk factors.
- Identify the pivotal role of subgingival microbes in the development and progression of periodontal diseases.
- Note the bidirectional relationship between periodontal inflammation and chronic systemic diseases, emphasizing the importance of dental hygienists in educating patients and promoting overall health awareness.
Periodontal diseases are a significant public health concern, affecting 42% of the United States population aged 30 or older.1 Internationally, periodontal diseases affect at least one tooth in 80% of adults, yet many patients are unaware of the long-term effects on their health.2 Periodontitis is associated with a variety of systemic disorders including cardiovascular diseases, diabetes mellitus, respiratory problems, preterm birth, autoimmune disorders, and cancer.2
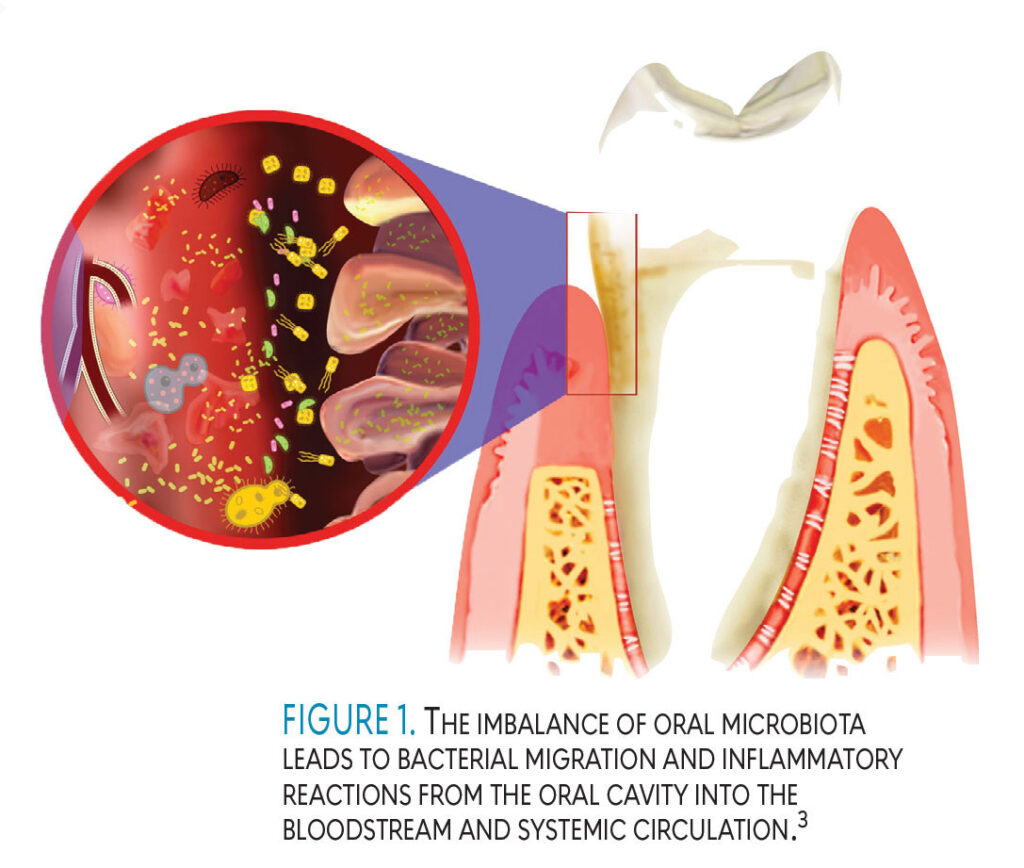
Periodontal diseases manifest as localized infections. When systemic mediators and metabolic products from these periodontal pathogens enter the bloodstream, they can contribute to the development of systemic disorders (Figure 1).2,3 Dental hygienists are well positioned to educate patients on this interplay between systemic and periodontal diseases in order to help them improve their overall health.
Immune and Inflammatory Responses
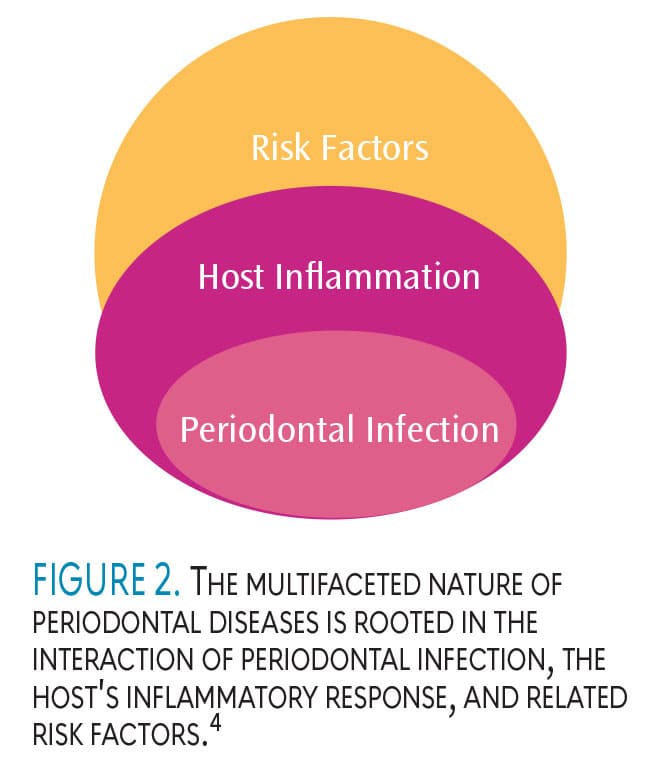
Periodontal diseases arise from bacterial infections in which subgingival pathogens play a crucial role in the disease process. However, the presence of this subgingival infection alone is not enough to cause tissue destruction. The manifestation of periodontal diseases requires not only an escalated host inflammatory response to the bacterial infection but also specific risk factors that influence the host’s inflammatory response. This interplay between periodontal infection, host inflammatory response, and associated risk factors constitutes the fundamental basis of the multifaceted nature of periodontal diseases (Figure 2).4
Bacterial plaque and its byproducts in a susceptible host are key to the development of periodontal diseases.1 The host-mediated inflammatory response is responsible for the progressive destruction of the supporting structures in the periodontium, including the alveolar bone. Research demonstrates that periodontal diseases are not just simple bacterial infections, but complex disorders in which multiple factors interplay with the subgingival microbes and host-immune and inflammatory responses.1
The relationship between periodontal health and overall health is bidirectional. Infections such as endocarditis; systemic conditions including diabetes, preterm birth, and cardiovascular diseases; brain or lung abscesses; and septicemias may be related to oral bacteria introduced into the blood stream through the periodontal pockets.5 However, the presence of microorganisms among individuals with no evidence of periodontal disease progression suggests that the resultant systemic problem is the effect of the immune response, not just the presence of the bacteria.6,7 In other words, there is an association between periodontal and systemic health rather than cause and effect.8
Subgingival Microbes
The oral cavity consists of complex microbial flora. The ecological balance between microbes and host response determines the state of health or disease. In symbiosis where a mutually beneficial relationship exists between the host and the microorganisms, health is achieved. But when a microbial imbalance — called dysbiosis — occurs, certain species of microbes in the biofilm become dominant, causing disease.8 Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia are the anaerobic microbial species strongly associated with periodontal diseases.
P. gingivalis lipopolysaccharides (LPS) contribute to periodontal inflammation and are associated with some inflammatory processes in systemic diseases, including initiating vascular and atherosclerotic changes in those with cardiovascular disease.9,10
Prevotella intermedia and Fusobacterium nucleatum are associated with a chronic form of periodontitis and Aggregatibacter actinomycetemcomitans is related to an aggressive form of periodontitis.1 P. intermedia is known to increase gingival inflammation during the second trimester of pregnancy.8 The microbes present in the dental plaque biofilm initiate the host-inflammatory response, which can lead to tissue destruction.1
Subgingival plaque biofilms provide a large and persistent source of periodontal pathogens to the host.8 Bacteria and their byproducts are introduced into the bloodstream during toothbrushing, flossing, and subgingival irrigation. Infections in periodontal pockets disseminate inflammatory mediators to the blood stream, triggering significant systemic inflammation.7
Host Response
The initial inflammation in periodontal tissues is the physiologic defense mechanism to protect the tissues against the Gram-negative bacteria in the biofilm. The body’s reaction to these bacteria is called the host response.8
Bacteria alone are not sufficient to cause the tissue destruction seen in periodontal diseases but the body’s response to the bacteria is. Inflammation plays a dual role in periodontal diseases. If the plaque is removed at an early stage, inflammation is resolved and tissue health is maintained. But if inflammation persists and the host is unable to resolve the inflammation, chronic inflammation ensues, leading to damage of the periodontal tissues.8
There are four histological stages in the development of periodontal diseases: initial lesion, early lesion, established lesion, and advanced lesion. In the initial, early, and established lesion stages, the host response can control the bacterial pathogens. In the advanced lesion histological stage, irreversible damage to the periodontium occurs, leading to periodontitis.8
Genetic, environmental, and acquired factors may affect the host-immune response.8 Variations in genes that control the formation of biochemical mediators may impact the immune response to plaque biofilm. Environmental factors, such as smoking, can modify both the host and inflammatory response. Tobacco smoking decreases the vascularity of the gingival tissue, reduces the phagocytic activity of the polymorphonuclear neutrophil (PMN), and affects the lymphocyte response to periodontal pathogens, hindering the immune response.8 Acquired factors, such as diabetes, impact the host response by reducing PMN function.10
Periodontal Inflammation and Chronic Disease
When pathogenic bacteria infect the periodontium, the body mobilizes its defense immune cells and releases mediators to fight the infection.10 The first response to bacterial biofilm is periodontal inflammation.
Periodontal diseases result when periodontal inflammation fails to resolve in susceptible individuals. An essential goal of intervention in inflammatory disease is the return of tissue to homeostasis, or the absence of inflammation.9 There are two types of mediators: pro-inflammatory mediators and anti-inflammatory mediators.
Pro-inflammatory mediators are related to tissue destruction, while anti-inflammatory mediators limit periodontal disease progression.6 The pro-inflammatory mediators produced locally in inflamed periodontal tissues disseminate into the bloodstream. For example, in chronic periodontitis, bacterial antigens are processed and presented to the body’s immune system and recognized by lymphocytes. Host-immune cells secrete pro-inflammatory mediators leading to increased circulating tumor necrosis factor-alpha (TNF-α), an inflammatory cytokine associated with obesity, diabetes, and periodontitis.
The inflammatory cascade initiated by the mediators in periodontal diseases may cause oral microbes, lipopolysaccharides, and proinflammatory molecules to gain access to different parts of the body, thus contributing to chronic systemic conditions and infectious diseases.5 Pro-inflammatory mediators, such as matrix metalloproteinases (MMPs), TNF-α, interleukin -6, and prostaglandin E2, are related to tissue destruction, while anti-inflammatory mediators, such as tissue inhibitors of MMPs and interleukin-4 and -10, often limit periodontal disease progression.10 When this switch does not happen, uncontrolled and chronic infection results.2
In typical circumstances, infection is neutralized by phagocytic cells engulfing the microorganism. This shifts back signals from pro-inflammatory to anti-inflammatory, thus restoring tissue integrity. When immune cells are unable to control pathogenic bacteria growth, chronic inflammation occurs. This chronic inflammation is the link to the bidirectional relationship between systemic and periodontal diseases. The association between oral inflammation in periodontal diseases and systemic inflammation is essential to understanding the long-term detrimental effects of periodontal inflammation on a multitude of organs.5
Chronic periodontal diseases may worsen systemic disease via direct and indirect routes. The direct route is through ulceration in the lining of periodontal pockets, from which bacteria can pass into the systemic circulation, leading to bacteremia. This allows periodontal pathogens to settle in distant organs, aggravating existing disease conditions.1
The indirect route is via chronic periodontal diseases that provide a significant and constant source of inflammation, exacerbating other disease conditions in which inflammation is a major component.1 For example, periodontal infection heightens systemic inflammation, initiates the host-immune response, and increases levels of fibrinogen among those with atherosclerosis. In addition, periodontitis may elevate serum cholesterol, hinder glycemic control, and increase the risk of pneumonia.11 Patients may not be aware of this association, which emphasizes the importance of dental hygienists as educators.
Role of the Dental Hygienist
Dental hygienists play an important role in supporting both the oral and systemic health of their patients. Because oral health is related to a variety of systemic health problems, dental hygienists need to remain up-to-date on the oral-systemic connection.11 This association should be considered during patient assessment, diagnosis, treatment planning, and referral to dental specialists and medical providers.11
Strong self-care regimens are key to maintaining health in patients with systemic diseases, in addition to understanding the impact of oral health on their specific health conditions. Patients with diabetes may experience slower wound healing, xerostomia, and fungal infections, which should be addressed during the dental appointment. Educating and motivating patients to quit tobacco use is helpful in the prevention of periodontal diseases and heart disease.12
Dental hygienists should educate pregnant patients on the importance of maintaining oral health and the fact that dental care is appropriate at any time during pregnancy. All women should be aware of the association between periodontal infection and adverse pregnancy outcomes, such as low-birth weight.8
Poor nutrition is not only a risk factor for poor oral health but also for diabetes and cardiovascular disease. Therefore, nutritional counseling is important in the dental setting. Specific dietary counseling may reduce the risk for diabetes, cardiovascular disease, periodontal diseases, and caries. Nutritional counseling can be done in collaboration with other healthcare professionals. This type of intervention may be particularly beneficial for patients at risk for diabetes, cardiovascular disease, stroke, osteoporosis, cancer, eating disorders, and other systemic conditions.12
 Motivational interviewing (MI) offers a patient-centered approach aimed at empowering individuals to make positive changes in their behavior.13 This collaborative style fosters patient motivation, making it effective for managing chronic diseases, preventing illnesses, and minimizing the risk of additional health issues.174,15 Its core elements include partnership, acceptance, compassion, and evocation, while essential skills encompass asking open-ended questions, affirmation, reflection, paraphrasing, and seeking permission before offering advice (Table 1).4 By employing MI, dental hygienists can address barriers to healthy habits and improve patient compliance.
Motivational interviewing (MI) offers a patient-centered approach aimed at empowering individuals to make positive changes in their behavior.13 This collaborative style fosters patient motivation, making it effective for managing chronic diseases, preventing illnesses, and minimizing the risk of additional health issues.174,15 Its core elements include partnership, acceptance, compassion, and evocation, while essential skills encompass asking open-ended questions, affirmation, reflection, paraphrasing, and seeking permission before offering advice (Table 1).4 By employing MI, dental hygienists can address barriers to healthy habits and improve patient compliance.
Oral examination can reveal signs and symptoms of immunologic diseases, endocrinopathies, hematologic conditions, systemic infections, and nutritional disorders.16 For example, oral manifestations of anemia include mucosal pallor, mucosal burning, pain, candidiasis, and atrophic glossitis.16 Patients with diabetes may present not only with delayed healing and bleeding but can also atrophy of the tongue papilla, burning mouth syndrome, and taste dysfunction. Careful intra- and extraoral examination can reveal findings of an underlying systemic disease.16
Conclusion
Dental hygienists play an important role in assessing oral-systemic risks and managing those risks by providing periodontal exams, systemic risk assessments, and dental and medical referrals. This multidisciplinary approach may improve patient outcomes. In addition, educating patients regarding the oral-systemic link will help them make informed decisions about their health.
References
- Lim G, Janu U, Chiou LL, Gandhi KK, Palomo L, John V. Periodontal health and systemic conditions. Dent J. 2020;8:130.
- Jain P, Hassan N, Khatoon K, et al. Periodontitis and systemic disorder — an overview of relation and novel treatment modalities. Pharm. 2021;13:1175.
- Boynes SG, Krol DM, Deutchman M. Supporting oral-systemic health. Dimensions of Dental Hygiene. 2022;20(2):43-46.
- Lee LL. The importance of interpersonal communication skills. Dimensions of Dental Hygiene. 2018;16(9):38–41.
- Lasserre JF, Brecx MC, Toma S. Oral microbes, biofilms and their role in periodontal and peri-implant diseases. Mater. 2018;11:1802.
- Cekici A, Kantarci A, Hasturk H, Van Dyke TE. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontol 2000. 2014;64:57-80.
- Fiorillo L, Cervino G, Laino L, et al. Porphyromonas gingivalis, periodontal and systemic implications: a systematic review. Dent J. 2019;7:114.
- Gehrig JS, Shin DE, Willmann DE. Foundations of Periodontics for the Dental Hygienist. 5th ed. Burlington, Massachusetts: Jones & Bartlett Learning; 2018:206–212.
- Nazir MA, Izhar F, Akhtar K, Almas K. Dentists’ awareness about the link between oral and systemic health. J Family Community Med. 2019;26:206–212.
- Martínez-García M, Hernández-Lemus E. Periodontal inflammation and systemic diseases: an overview. Front Physiol. 2021;12:709438.
- Wilder RS, Iacopino AM, Feldman CA, et al. Periodontal-systemic disease education in U.S. and Canadian dental schools. J Dent Edu. 2009;73:38-52.
- Genco RJ, Genco FD. Common risk factors in the management of periodontal and associated systemic diseases: the dental setting and interprofessional collaboration. J Evid Based Dent Pract. 2014;14:4-16.
- Douglass JM, Clark MB. Integrating oral health into overall health care to prevent early childhood caries: need, evidence, and solutions. Pediatric Dent. 2015;37:266–274.
- Östlund AS, Kristofferzon ML, Häggström E, Wadensten B. Primary care nurses’ performance in motivational interviewing: a quantitative descriptive study. BMC Family Prac. 2015;16:89.
- Schoo AM, Lawn S, Rudnik E, Litt JC. Teaching health science students foundation motivational interviewing skills: use of motivational interviewing treatment integrity and self-reflection to approach transformative learning. BMC Med Educ. 2015;15:228.
- Chi AC, Neville BW, Krayer JW, Gonsalves WC. Oral manifestations of systemic disease. AmFam Phys. 2010;82:1381-1388.
From Dimensions of Dental Hygiene. March 2024; 22(2):36,39-41



