Evaluating Scientific Methodologies
This course was developed in part with an unrestricted educational grant from Colgate Oral Pharmaceuticals.
This course was published in the February 2010 issue and expires February 2013. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the types of clinical studies and define their function.
- Define essential design criteria needed for reliable clinical trials.
- List the four phases of clinical trials and describe the purpose of each phase.
- Describe selected prominent indices used to assess plaque and gingival inflammation in oral care clinical trials.
FROM THE GUEST EDITOR
Reviewing the literature may not be easy or exciting but it is necessary in order for dental professionals to keep abreast of the new trends and products available in dentistry today. The third article in the the Leveraging Scientific Evidence to Improve the Oral Health Practices of Patients series, “Evaluating the Evidence,” covers another critical element—the methodologies used in a clinical trial to critically assess gingivitis and plaque among study subjects. The authors provide an overview of the types and phases of clinical trials and describe the most widely used indices for plaque and gingivitis assessment in oral care research. —Christine A. Hovliaras, RDH, BS, MBA, CDE, Guest Editor
The effective management of caries and gingival diseases relies on the treatment regimens delivered by the dental team and the preventive self-care routine performed by the patient. To determine which treatments are best for the prevention and management of these diseases, dental professionals must be able to evaluate clinically relevant evidence on which therapies reduce dental plaque and gingival inflammation. Therefore, the accurate and reliable measurement of dental plaque and gingival inflammation is imperative to ascertain clinical effectiveness. The necessary clinical evidence to support treatment regimens is only reached through carefully controlled studies conducted in humans that test the safety and efficacy of drugs or treatments.
A clinical trial is an organized experiment using human volunteers (subjects) designed to answer specific questions about the safety and/or effectiveness of drugs, vaccines, therapies, or innovative ways of using existing treatments.1 Only clinical trials that adhere to strong principles of scientific experimentation offer a reliable basis for accurately evaluating the efficacy and safety of new health care approaches.2
Various types of clinical trials are conducted based on the research question. Prevention trials attempt to discover more effective methods of preventing the occurrence of disease in those who have never had the illness or to avert the return of a disease. Prevention trials usually involve medicines, vaccines, vitamins, or lifestyle changes. Screening trials are used to detect a disease before any symptoms are noticeable and usually involve imaging, laboratory, and genetic tests. Diagnostic trials strive to find improved tests for identifying a disease, and subjects recruited for diagnostic trials are usually exhibiting symptoms of the disease. Diagnostic trials investigate new treatments, combination of drugs, or procedures for treatment of a specific disease. Quality of Life trials explore ideas for improving the comfort and quality of life for people who have chronic illness. Lastly, Compassionate Use trials offer a mechanism for providing investigational drugs to seriously ill patients who are not eligible to receive the therapy in a clinical trial but have no other treatments options.3
Important Criteria for Reliable Clinical Trials
Clinical trials conducted to determine the safety and efficacy of drugs or treatments are difficult to execute, expensive to complete, and timeconsuming. To develop an efficient and trustworthy clinical trial, specific characteristics are written into a document called the clinical trial protocol, which describes the scientific rationale, objectives, experimental design, methodology, statistical analyses, and the organization of the clinical trial. To ensure meaningful information for the public from clinical trials, the following criteria must be carefully considered:
1. Randomization. Participants in a clinical trial are assigned to either a treatment group or a comparison (control) group. The investigator has direct control over subject assignment and since these subjects are followed over time to ascertain differences in the outcomes between the treatment and control groups, the assignment of subjects is of paramount importance. Randomization of the study subjects means having no specific pattern, arrangement, or predictable outcome in the assignment of study subjects. Treatment and control groups must be comparable in all aspects. Which group becomes the treatment group as opposed to the control group should be based on chance. Since the process of randomization provides comparable groups without bias, the differences in outcomes between groups can be attributed to the intervention being studied and permits a definitive interpretation of the trial results.
2. Masking. Masking investigators and participants to the therapy provided aids in prevention of bias in the clinical study. Awareness of the treatment received by the subject or investigator can influence the perception of the benefit by the subject as well as the observation or care by the provider. To prevent this biased assessment of outcomes, subjects, observers (investigators), and statistician(s) are not informed about what group subjects are assigned. A single masking occurs when subjects are unaware of who is in the treatment group vs the control group. A double masking occurs when both subjects and investigators are unaware of who is in the treatment or control groups and a triple masking occurs when subjects, investigators, and statisticians are unaware of who is in the treatment or control groups.
3. Control group. To determine if the group being treated in the clinical trial has been affected, the treated group must be compared to the control group. The control group should be identical to the treatment group with the exception of the single variable of interest whose effect is being tested. In many control groups a placebo is given to the participants in order to ensure blindness for both the subjects and investigators to which group is receiving the treatment being tested.
4. Statistical power. To determine if a treatment is effective, statistical tests must be used to confirm that inferences about this population are accurate. The ability of a statistical test to correctly determine differences between groups is dependent on the size of the sample as well as the size of effect being measured. Hence, the number of enrolled participants has a significant bearing on the study’s ability to detect differences between the treatment and control groups. The larger the sample size, the greater the statistical power. Without appropriate statistical power, the clinical trial cannot accurately determine if differences exist between groups, and efficacy may be missed.
5. Ethics. A crucial component for any clinical trial is the ethical recruitment of subjects. All participants in a study must be clearly informed of the risks and possible benefits of the trial prior to giving their consent to participate. Informed consent is a document that lists benefits and risks of the clinical trial in lay terms and is signed by participants prior to entry into the study. The clinical trial protocol and all components of the informed consent must be reviewed and approved by scientific institutions and funding agencies prior to patient recruitment.
Phases of Clinical Trials
When new drugs or devices are being investigated, approval of drug efficacy and safety occurs in four phases. Each phase of the approval process is executed separately. The first stage of drug approval using clinical trials—Phase I—assesses safety, tolerability, pharmacodynamics, and pharmacokinetics of a drug in a small cohort of healthy subjects.4 Once the initial safety of the drug has been confirmed, Phase II studies use larger groups of healthy volunteers to further assess drug efficacy while continuing to evaluate safety.4 Phase III studies are large clinical studies, usually in randomized, controlled, multicenter trials, in affected study participants that are designed to provide the definitive review of efficacy and safety.4 If the drug is shown to be safe and effective after Phase III trials, approval by the appropriate regulatory agency can be obtained. Once the drugs are placed on the market for patient use, Phase IV trials involve safety surveillance to detect any rare or long-term adverse effects in larger patient populations.4
Significance of Plaque and Gingival Inflammation
Daily oral hygiene practices mechanically disrupt bacteria on tooth surfaces, thereby helping to maintain a state of equilibrium between the host and bacteria flora.5 Effective plaque control practices equate to the absence of visible inflammation and healthy sulcus depths of 1 mm to 3 mm.6 However, when self-care measures decline, increasing numbers of gram-negative anaerobes, spirochetes, and motile bacterial species colonize the tooth surfaces, causing a host immune response. Clinical signs of inflammation are observed along with a deepening of probing depths.7 Bleeding on probing is also a sign of gingival inflammation.8
Ideal periodontal clinical trials report not only a statistically significant effect of the study product, but also a clinically significant result. The statistical p-value allows discussion of the probability of whether a new therapy has any positive (or negative) value, however, inferences about the study’s therapy providing a meaningful clinical effect should be avoided.9
Diagnosis of Plaque-Induced Gingivitis
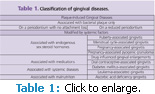
The classification of gingival diseases that rely on dental plaque to initiate the disease process(es) are organized into two large categories: those affected by local factors and those affected by local factors and modified by specific systemic factors found in the host.10 The modification of plaque-induced gingival diseases by systemic factors principally occurs via the endocrine system, hematologic diseases, drugs, or malnutrition (Table 1).11
The gingival diseases associated with plaque, endogenous hormonal fluctuations, drugs, systemic diseases, and malnutrition have several essential characteristics in common (Table 2). The universal features of these gingival diseases include clinical signs of inflammation, signs and symptoms that are confined to the gingiva, reversibility of the diseases by removing the etiology(ies), the presence of bacterial laden plaque to initiate and/or exacerbate the severity of the lesion, and a possible role as a precursor to attachment loss around teeth.11
Table 2.
- Symptoms that are confined to the gingiva.
- The presence of dental plaque to initiate and/or exacerbate the severity of the lesion.
- Clinical symptoms associated with stable attachment levels on a periodontium with no loss of attachment or on a stable but reduced periodontium.
- Clinical signs of inflammation (enlarged gingival contours due to edema or fibrosis, color transition to a red and/or bluish-red hue, elevated sulcular temperature, bleeding on stimulation, increased gingival exudate).
- Reversibility of the disease by removing the etiology(ies).
- Possible role as a precursor to attachment loss around teeth.
Types of Plaque Indices Used in Clinical Trials
Clinicians, researchers, and community practitioners use oral hygiene indices to educate and motivate patients and evaluate treatment and self-care outcomes; assess the effects of innovative agents or procedure on prevention, progression, or control of a disease; and identify trends or patterns of oral health and disease in large populations.12
The Oral Hygiene Index (OHI)13 was designed to quantify the oral cleanliness status in an individual or large population. OHI has two components: the Debris Index and the Calculus Index. Each component has its own scoring criteria and is calculated and reported independently but combined to report the final OHI outcome. Oral debris for OHI is defined as soft foreign matter on the surface of the teeth consisting of bacteria, material alba, and food. To score, each arch is divided into segments, two posterior and one anterior. Using a number five explorer, the examiner passes the instrument over the buccal and lingual surfaces of the teeth while observing the extent of debris removed from each surface. Two numerical scores are assigned to each segment based on the buccal and lingual surface displaying the most debris.
The Periodontal Disease Index (PDI)14 is an assessment tool that includes a select number of sample teeth that provide a valid representation of the disease status in the entire mouth; probing depth measured in relation to the cemento-enamel junction; and measurement of gingival, plaque, and calculus findings as adjunct parts of the index. Selected teeth are stained and then scored according to specific criteria. The final PDI score is calculated by summing all numeric values divided by the number of examined teeth.
The Quigley-Hein Plaque Index15 is an assessment method still used today in clinical trials that evaluates oral hygiene products. All teeth are stained and then rated based on the quantity of plaque on the buccal, labial, and lingual surfaces.
The Plaque Index (PI)16 evaluates the thickness of plaque at the gingival margin. Four surfaces on six selected teeth are given a score of 0 to 3 based on quantity of plaque. The PI is attained by passing an explorer along the supragingival and subgingival surfaces of the teeth. Final PI results can be reported on various levels— per area, tooth, group of teeth, or individual.
The Plaque Control Record17 was created as a rapid assessment tool. The index records only the presence of plaque on individual tooth surfaces. The Plaque Control Record affords patients an instrument for monitoring individual self-care progress. Disclosing solution or a chewable tablet is used to stain all the teeth. The examiner inspects all teeth and records the presence of plaque on the mesial, distal, facial, and lingual surfaces. Final results are tabulated by multiplying the number of surfaces with plaque by 100 then dividing by the number of available tooth surfaces. The result is a percentage of plaque present in the mouth.
The Patient Hygiene Performance (PHP) Index18 was first used as an oral hygiene assessment method when working with patients. Oral debris for the PHP Index is defined as soft foreign matter consisting of bacteria, mucin, and food loosely attached to tooth surfaces. Teeth are disclosed and a mouth mirror examination is made of specific teeth. The examiner mentally divides each tooth into five subsections and determines the presence or absence of oral debris on each of the subdivisions. Summing the values for each of the five subdivisions provides the oral debris score for the tooth. An overall patient hygiene performance score is tabulated by dividing the sum of the tooth scores by the number of surfaces charted.
The Plaque Severity Index (P-S Index)19 is used in clinical research studies comparing the effects of chemotherapeutic agents on new or established supragingival plaque formation and gingivitis. This index measures the proportion of tooth sites rated with high Quigley-Hein Plaque Index scores. The final result yields an assessment of how effective the test agent is on tooth surfaces with higher plaque accumulations.
Gingival Indices Used in Clinical Trials
The first attempt to quantify the severity of gingival inflammation objectively was the development of the papillary portion (P), marginal portion (M), and attached portion (A) index—P-M-A Index.20 The goal is to assess the presence of symptoms of established gingivitis. Each gingival unit is subdivided into three defined portions: papillary, marginal, and attached. A numerical score is assigned to each tooth based on the degree and extent of the inflammation. Qualitative assessment is classified based on the type of gingivitis present: acute or chronic.
The PM-Index classifies up to three distinct entities of gingivitis: morbidity, prevalence, and severity.21 Labial gingiva of the upper and lower anterior regions are examined for gingivitis. The result is expressed as a percentage of the number of subjects who have one or more of the gingival units inflamed to the total number of children examined. If gingival inflammation is present, its extent and severity are then measured by counting the number of affected gingival units found in the inspected regions. Severity is scored according to the degree of inflammation in PM-units.
The Sulcus Bleeding Index (SBI)22 locates initial areas of gingival bleeding and color variations and is based on the principles that early signs of marginal gingivitis include increased gingival crevicular fluid flow rates and bleeding on probing. A blunt periodontal probe is positioned parallel to the long axis of the tooth recording the labial and lingual bleeding points, and angling toward the interdental col to record proximal sites for bleeding.
The Papillary Bleeding Index23 uses the presence or absence of papillary bleeding when using a toothpick between the teeth as criteria.
The Gingival Index (GI)24 evaluates the severity of gingivitis based on color, consistency, and bleeding on probing using selected teeth. Four sites on each study tooth are examined for the presence of bleeding.
The Gingivitis Severity Index19 is an assessment tool currently used in clinical trials assessing the efficacy of antibacterial agents in controlling gingivitis.
The Gingival Bleeding Index (GBI)25 uses site prevalence results to document gingival inflammation and oral hygiene. Inflammation is determined by gently probing in the sulcus around the gingival margin, waiting 10 seconds, and then recording the presence or absence of bleeding. Final results are reached by dividing the number of positive sites by the number of sites examined.
The Gingival Exudate Index26 is founded on the principle that the flow rate of gingival crevicular fluid (GCF) directly corresponds to the level of inflammation.27 This index uses filter paper strips to collect both extracrevicular and intra cre vi cular GCF.
The Future
Investigators are developing new research methodologies. But, before these innovative applications can be implemented, dental professionals need to ensure they have been validated using independent clinical trails. Novel methodologies must account for the clinical assessment of all teeth for plaque measurements and all gingival tissues for gingival inflammation assessments.
REFERENCES
- Pocock SJ. Clinical Trials A Practical Approach. West Sussex, England: Wiley; 1983:1.
- Hulley SB, Cummings SR, Browner WS, Grady D, Hearst N, Newman TB. Designing Clinical Research. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2001:7.
- Glossary of Clinical Trials Terms. A service of the US National Institutes of Health. Available at: http://clinicaltrials.gov/ct2/info/glossary. Accessed March 15, 2010
- FAQ: ClinicalTrials.gov—Clinical Trial Phases. Available at: www.nlm.nih.gov/services/ctphases.html. Accessed on March 15, 2010.
- Haffajee AD, Teles RP, Socransky SS. The effect of periodontal therapy on the composition of the subgingival microbiota. Periodontol 2000. 2006;42:219-258.
- Newman MG, Takei HH, Carranza FA, eds. Carranza’s Clinical Periodontology. 10th ed. Philadelphia: WB Saunders Co; 2006:242-262, 432-453.
- Socransky SS, Haffajee AD. Dental biofilms: difficult therapieutic targets. Periodontol 2000. 2002;28:12-55.
- Armitage GC. Diagnosis of periodontal diseases. J Periodontol. 2003;74:1237-1247.
- Greenstein G. Clinical versus statistical significance as they relate to the efficacy of periodontal therapy. J Am Dent Assoc. 2003;134,583-591.
- Albandar JM. Epidemiology and risk factors of periodontal diseases. Dent Clin North Am. 2005;49:517-532.
- Mariotti A. Dental plaque-induced gingival diseases. Ann Periodontol. 1999;4:7-17.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2009;326-327.
- Greene JC, Vermillion JR. The oral hygiene index: a method for classifying oral hygiene status. J Am Dent Assoc. 1960;61:172-179.
- Ramfjord, SP. The periodontal disease index. J Periodontol. 1967;38Suppl:602-610.
- Quigley GA, Hein JW. Comparative cleansing efficiency of manual and power brushing. J Am Dent Assoc. 1962;65:26-29.
- Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121-135.
- O’Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972:43:38.
- Podshadley AG, Haley JV. A method for evaluating oral hygiene performance. Public Health Rep. 1968;83:259-264.
- Palomo F, Wantland L, Sanchez A, DeVizio W, Carter W, Baines E. The effect of a dentifrice containing triclosan and a copolymer on plaque formation and gingivitis: A 14-week clinical study. J Am Dent Assoc. 1989;2:231-237.
- Massler M. The P-M-A index for the assessment of gingivitis. J Periodontol. 1967;38Suppl:592-601.
- Muhlemann HR, Mazor ZS. Gingivitis in Zurich school children. Helv Odont Acta. 1958;2:3-12.
- Muhlemann HR, Son S. Gingival sulcus bleeding-a leading symptom in initial gingivitis. Helv Odont Acta. 1971;15:107-113.
- Saxer UP, Muhlemann HR. [Motivation and education]. SSO Schweiz Monatsschr Zahnheilkd. 1975;85:905-919. German.
- Loe H, Silness J. Periodotnal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533-551.
- Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25:229-235.
- Loe H, Holm-Pedersen P. Absence and presence of fluid from normal and inflamed gingivae. Periodontics. 1965;149:171-177.
- Lamster IB, Ahlo JK. Analysis of gingival crevicular fluid as applied to the diagnosis of oral and systemic diseases. Ann N Y Acad Sci, 2007;1098:216-229.
From Dimensions of Dental Hygiene. April 2010; 8(4) Insert.