
Update on Methods for Oral Biofilm Disruption
Regular personal and professional biofilm removal is key to preventing and treating oral infections.
This course was published in the December 2017 issue and expires December 2020. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define biofilms.
- Identify the two strategies for biofilm control.
- Discuss the effectiveness of the myriad methods for biofilm removal, both at home and in the oral health care setting.
Biofilms are composed of bacteria adhering to each other or to living or nonliving surfaces. They form complex communities surrounded by extracellular polymeric substances.1 Cells within these biofilms have changing physiologic and metabolic properties that contribute to their persistence.1 If not removed regularly, a complex and mature biofilm develops, with up to 100 bacterial species at a single site.2 Oral biofilm exposed to an excess of carbohydrates contains mainly Gram-positive carbohydrate-fermenting bacteria that may cause demineralization, caries, pulpitis, and periodontitis.2–4 Supra- and subgingival oral biofilms dominated by Gram-negative anaerobic bacteria colonize and cause gingival inflammation. Subsequently, gingivitis, chronic and aggressive periodontitis, and peri-implantitis can ensue.2,3 There are two strategies for biofilm control: interfere with attachment, and remove or disrupt biofilm. Total removal is not possible;1 therefore, disruption is the most practical option.4
TOOTHBRUSHING
Toothbrushing is the most powerful way to disrupt supragingival biofilm at home, preventing colonization of microbes subgingivally. Research shows that both manual toothbrushing and power toothbrushing result in a reduction of plaque scores.5,6 Many types of manual toothbrushes are available. Results of randomized controlled trials found no difference in plaque removal between different types of manual toothbrushes,7,8 and all manual toothbrushes were efficacious.7 A systematic review is needed to investigate the effects of filament texture and arrangement on plaque, gingivitis, and adverse events.9
Power toothbrushes have different modes of action to improve efficacy, such as sonic, ultrasonic, rotating, counter-oscillating, oscillating rotation, back and forth, and side to side.6,10 Systematic reviews found that power and manual brushing are at least equally effective in removing plaque, reducing gingival inflammation,11–13 and preventing calculus formation.12 The key to an effective power toothbrush is the presence of a moving brush head.6 Both vertical and horizontal methods are effective in biofilm removal; however, one study found that the vertical method removed more plaque from the interproximal surfaces and produced lower plaque scores than the horizontal method.14 This finding is noteworthy because this clinical trial looked at brushing in regard to interproximal effectiveness.
Duration of brushing remains a key factor in efficacy of biofilm removal. After 2 minutes of brushing, a 41% reduction in plaque scores was found compared with only a 21% reduction after 1 minute of brushing.5 For gingivitis prevention, brushing at least 2 minutes twice per day with fluoride toothpaste was supported for all patient populations, while 2 minutes was found to be insufficient for patients with periodontitis.9
ANTIBACTERIAL DENTIFRICES
Toothbrushing provides the main mechanical effect of plaque removal, not toothpaste.15 However, adding antibacterial ingredients within dentifrice is helpful for biofilm management. When combined with fluoride (for caries prevention), antibacterial pastes provide an efficacious option for combating oral diseases.
Stannous fluoride has antibacterial effects against species associated with plaque, gingivitis, caries, and malodor, and it reduces plaque, gingival inflammation, and bleeding.16 Stannous fluoride and sodium hexametaphosphate inhibit calculus and stain formation.16
Triclosan/copolymer fluoride dentifrices reduced gingival inflammation and gingival bleeding when compared with conventional fluoride dentifrices. Also, high-quality evidence demonstrated that the use of triclosan/copolymer fluoride dentifrices led to a small reduction in coronal caries, while weaker evidence demonstrated its effectiveness in decreasing root caries and calculus.17
INTERDENTAL AIDS
Brushing alone does not significantly disrupt biofilm from proximal surfaces, therefore, patients should be educated about interdental self-care. In fact, interdental biofilm is more prevalent, acidogenic, and readily forming than other oral biofilm.18 Evaluation of patients’ interdental space accessibility should be part of all routine oral examinations.19
Floss does not meet the intraoral and personal needs of all patients. Also, compliance with daily flossing is low.20,21 Nevertheless, dental floss is ideal for those who can use it effectively and patients with type I gingival embrasure spaces and shallow pockets. Conversely, open embrasures and recession may be best treated with interdental brushes.
Flossing in addition to toothbrushing enhances interproximal biofilm disruption by 70% compared with 25% by brushing alone.8Although the quality of evidence about flossing’s efficacy is low, regular flossing with toothbrushing is effective in preventing gingivitis.22 Floss with 5% CHX resulted in additional reductions in supragingival biofilm when compared with waxed floss on the anterior teeth of a well-motivated and well-instructed population.23 It would be useful for future studies to focus on antimicrobials in floss for the general population to assess if regular use would be valuable.
Interdental brushes come in different widths to match a patient’s interproximal anatomy. Brushes for use around implants have a coated wire to avoid scratching and prevent galvanic shock. In general, interdental brushes as an adjunct to toothbrushing are more effective in removing plaque compared with brushing alone.24–26
Patients should approach the interdental space from both the buccal and lingual aspects to adequately disrupt the biofilm, particularly with spaces that are partially occluded with gingiva. Flexible interdental cleaners with rubber bristles are effective when compared with other interdental brushes and may offer increased patient comfort when compared with metal-core brushes.27
Few studies have looked at the efficacy of wood sticks on oral biofilm removal, periodontal diseases, or caries. A systematic review about triangular wood sticks in addition to toothbrushing showed no effect on plaque or gingival indexes.28 The review did find, however, an advantage in reducing interdental gingival bleeding.28 Wood sticks may be a viable alternative for patients who have not had success with other interdental aids.
ORAL IRRIGATORS
Oral irrigation can be used for supragingival or subgingival biofilm disruption or both, and with water alone or an antimicrobial. Two systematic reviews revealed that while the oral irrigator and toothbrushing did not reduce visible plaque biofilm, their use did improve gingival health.29,30 It may be that irrigation alters the composition of key pathogens, interferes with biofilm maturation, or changes the subgingival microbial environment due to the pulsating action.31 These effects are worth future investigation. Oral irrigators may be well suited for site-specific concerns, such as crowns, malocclusion, or other localized areas where persistent inflammation exists. In regard to implant care, CHX irrigation was found to be more effective in reducing biofilm and marginal bleeding scores when compared with rinsing with CHX alone.32
Water flossing is a relatively new term to describe oral irrigation. Results of two studies found the water flosser to be more effective than interdental brushes in removing plaque biofilm after a single use,33 and in reducing gingival bleeding over 2 weeks.34 Although these results are limited in scope, they do show promise for water flossing’s efficacy.
MOUTHRINSES
Evidence supports the use of antimicrobial mouthrinses in addition to mechanical biofilm disruption for most patients. These antiseptic rinses act on the oral biofilm’s ability to form, grow, and mature.35 In fact, toothbrushing in combination with any CHX mouthrinse was more effective than toothbrushing alone in biofilm reduction.36
Evidence supports the efficacy of CHX and essential oils (EO).36–39 Benefits for plaque and gingivitis were also shown with cetylpyridinium chloride (CPC).39 Patients with orthodontic appliances, mental or physical disabilities, systemic diseases, and smokers may particularly benefit from antimicrobial mouthrinse use.
CHX is an effective antimicrobial that has positive implications for both caries and gingivitis. CHX is active against Gram-positive and Gram-negative bacteria, yeasts, and viruses, and is bacteriostatic vs bactericidal.40 CHX mouthrinse is released slowly, has sustained release, and remains in the oral cavity for extended periods. It, therefore, has the ability to adsorb to oral mucosa, hydroxyapatite, and salivary glycoprotein. CHX mouthrinses are now formulated without alcohol.
EOs have been used as antimicrobials in mouthrinses for many years, and have been shown to have anti-plaque and anti-gingivitis properties. They are easy to use and purchase (no prescription needed) and there is no residual staining, as is the case with
CHX.41–43
While not an antimicrobial, delmopinol hydrochloride inhibits plaque and bacteria formation on the tooth surface.44 Other mouthrinse ingredients, such as chitosan-argininamide, tea tree oil, peppermint oil, lemon peel oil, and aloe vera, may provide benefits but more research is needed.
MECHANICAL DEBRIDEMENT
Mechanical biofilm disruption by the professional occurs both in the supragingival (oral prophylaxis/debridement) and the subgingival environment (scaling and root planing/debridement). Mechanical debridement of the subgingival environment remains the cornerstone of periodontal therapy. Although not a permanent solution to biofilm removal, mechanical therapy temporarily disrupts its aggregation. The American Dental Association’s (ADA) Evidence-Based Clinical Practice Guidelines on Nonsurgical Treatment of Chronic Periodontitis supports scaling and root planing as the initial nonsurgical treatment for chronic periodontitis.45
Scaling, debridement, root planing, and polishing all mechanically disrupt biofilm, which is absolutely necessary to prevent and treat biofilm-induced infections. Although calculus and calculus-retaining entities (overhangs) are not causative factors in inflammatory diseases, they do provide the niche necessary to harbor oral biofilms.46 Furthermore, removing only the superficial biofilm, and leaving calculus deposits underneath likely contributes to biofilm regrowth. The remaining deposit provides a niche for biofilm reformation in a rough and stagnant environment.
Burnished calculus deposits might attract oral biofilm and perpetuate inflammation.46 Use of the dental endoscope has aided in discovering the relationship between subgingival calculus covered with biofilm and inflammation of adjacent tissue.47 In fact, a strong correlation has been noted between bleeding on probing and subgingival biofilm and calculus post-scaling and root planing.48
Nonsurgical anti-infective periodontal therapy is another name for reducing biofilm via mechanical means of scaling and root planing.49 Unfortunately, nonsurgical periodontal therapy sometimes produces unfavorable results or fails where deep pockets and furcations are involved.50 However, moderate and shallow pockets have been effectively treated with mechanical debridement by disrupting and removing oral biofilms and removing calculus and other retaining entities.50,51
The outcomes of mechanical debridement in multirooted teeth are less favorable than single-rooted teeth.52 An update of periodontal therapy outcomes shows, however, that positive long-term survival rates can be accomplished in multirooted teeth based on the therapy provided.53 Initial furcations (degree I) can be successfully managed by nonsurgical mechanical debridement.53
The use of hand and power instrumentation provides similar clinical outcomes.54 Determining which type of mechanical debridement is best depends on myriad factors such as time spent, expertise, new vs experienced operators, experience with specific instruments, instrument selection, etc. Most likely, the optimal means of mechanical debridement is the combined use of hand and power instruments.55
A key to subgingival biofilm disruption is reevaluation and subsequent assessment of disease conditions at recare visits. These are the means by which a clinician decides, over time, when and if the root has been biologically well prepared for healing. This point of stability is different from patient to patient. The clinician’s responsibility is to determine a clinical endpoint during the mechanical debridement appointment(s) and a therapeutic endpoint at the reevaluation visit and recare appointments.56 The addition of a dental endoscope has been shown to enhance mechanical debridement by improving the removal of subgingival calculus and healing of the periodontium.57–60
An objective in mechanical periodontal therapy is to leave the root smooth without unnecessarily removing healthy root surface. A smooth root is thought to lend itself to less bacterial recolonization over time. When comparing instruments, curets, diamond burs, piezoceramic (used in scaling and root planing only), and piezosurgery ultrasonic instruments (used in bone surgery and root planing) in vitro, it was found that all reduced roughness of the root, however, the piezosurgery ultrasonic produced the smoothest surface.61When comparing a new sonic, piezoceramic, and double Gracey curet instruments, it was concluded that all were effective in root debridement during maintenance, and the ultrasonic resulted in the smoothest root surfaces.62
CONCLUSION
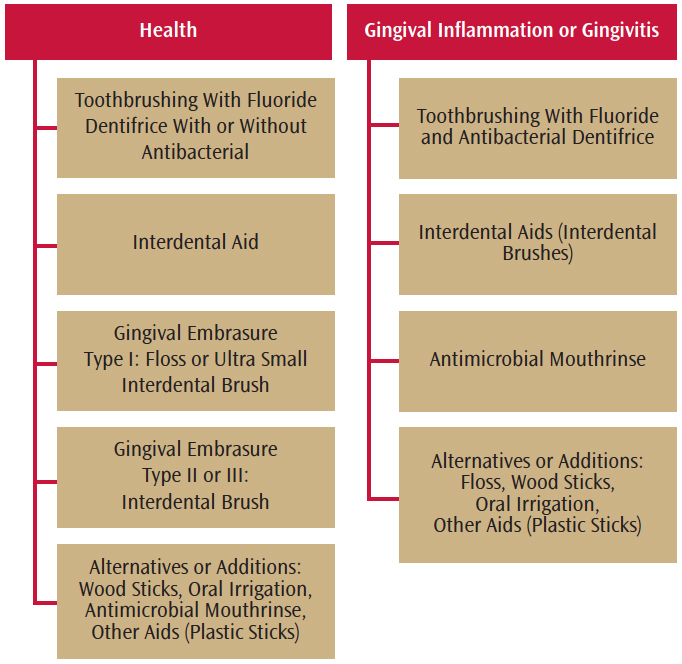
Regular personal and professional biofilm removal is key to preventing and treating oral infections.2 A single assault on biofilm, however, is not likely to achieve control; rather multiple strategies are needed for each individual patient (Figure 1). It is important to combine the scientific evidence, professional judgment, and patient needs to provide the best treatment and recommendations for biofilm disruption.
REFERENCES
- Cooper RA. Biofilms in wounds: a review ofpresent knowledge. J Wound Care. 2014;23:570–582.
- Larsen T, Fiehn N. Dental biofilm infections—anupdate. Biofilm Infections. 2017;125:376–384.
- Sanz M, Beighton D, Curtis MA, et al. Role ofmicrobial biofilms in the maintenance of oral health and in the development ofdental caries and periodontal diseases. J Clin Periodontol. 2017;44(Suppl 18):S5–S11.
- Kaidonis J, Townsend G. The”sialo-microbial-dental complex” in oral health and disease. Ann Annal.2016;203:85–89.
- Slot DE, Wiggelinkhulzen L, Rosema NAM, Van derWeijden GA. The efficacy of manual toothbrushes following a brushing exercise:a systematic review. Int J Dent Hyg. 2012;10:187–197.
- Rosema NAM, Slo DE, Van Palenstein Helderman WH,Wiggelinkhuizen L, Van der Weijden GA. The efficacy of powered toothbrushesfollowing a brushing exercise: a systematic review. Int J Dent Hyg. 2016;14:29–41.
- Nieri M, Giani M, Pagliaro U, Picciullo A,Franceschi D, Rotundo R. Efficacy and preference of manual toothbrushes: arandomized, single blind, controlled trial. Eur J Orl Implantol. 2013;6:181–188.
- Ashwath B, Vijayalakshmi R, Arun D, Kumar V.Site-based plaque removal efficacy of four branded toothbrushes and the effectof dental floss on interproximal plaque removal: a randomized examiner-blindcontrolled study. Quitessence Int. 2014;45(7):577–584.
- Chapple ILC, van der Weijdenn F, Doerfer C, etal. Primary prevention of periodontitis: managing gingivitis. J Clin Perio. 2015;42:S71–S76.
- Deacon SA, Glenny AM, Deery C, et al. Differentpowered toothbrushes for plaque control and gingival health. CochraneDatabase Syst Rev. 2010;12:CD004971.
- Goh EX, Lum PL. Fact or Fiction? PoweredToothbrushing is more effective than manual toothbrushing. Oral Health andPreventive Dentistry. 2017;15(1):23–32.
- Nagy P. Kover K, Gera I, Horvath A. Evaluationof the efficacy of powered versus manual toothbrushes in preventing oraldiseases. (Systematic review with meta-analysis). Fogory Sz. 2016;109:3–22.
- Yaacob M, Worthington HV, Deacon SA, et al.Powered versus manual toothbrushing for oral health. CochraneDatabase Syst Rev. 2014;17:CD002281.
- Mastroberardino S, Cagetti MG, Cocco F, Campus G.Pizzocri J, Strohmenger L. Vertical brushing versus horizontal brushing: arandomized split-mouth clinical trial. Quintessence Int. 2014;45:653–661.
- Valkenburg C, Slot DE, Bakker EWP, Van derWeijden FA. Does dentifrice use help to remove plaque? A systematic review. J ClinPeriodontol. 2016.43:1050–1058.
- Sensabaugh C, Sagel E. Stannous fluoridedentifrice with sodium hexametaphosphate: Review of laboratory, clinical andpractice-based data. J Dent Hyg. 2009;83:70–78.
- Riley P, Lamont.T. Triclosan/copolymer containingtoothpastes for oral health. Cochrane Database Syst Rev. 2013;12:CD010514.
- Johnson TM, Worthington HV, Clarkson JE, et al.Mechanical interdental cleaning for preventing and controlling periodontaldiseases and dental caries (Protocol). Cochrane Database Syst Rev. 2013;18;12:CD009857.
- Carrouel F, Llodra JC, Viennot S, Santamaria J,Bravo M, Bourgeois D. Access to interdental brushing in periodontal healthyyoung adults: a cross-sectional study. PLoS One. 2016;11:e0155467.
- Wiener RC, Crout RJ, Wiener MA. Toothpaste use bychildren, oral hygiene, and nutritional education: an assessment of parentalperformance. J Dent Hyg. 2009;83:141–145.
- Santos A, Pascual A, Llopis J, et al.Self-reported oral hygiene habits in smokers and nonsmokers diagnosed withperiodontal disease. Oral Health Prev Dent. 2015;13:245–1251.
- Sambunjak D, Nickerson JW, Poklepovic T, et al.Flossing for the management of periodontal diseases and dental caries inadults. Cochrane Database Syst Rev. 2011;12:CD008829.
- Muniz FW, Sena KS, de Oliveira CC, Verissimo DM,Carvalho RS, Martins RS. Efficacy of dental floss impregnated withchlorhexidine on reduction of supragingival biofilm: a randomized controltrial. Int J Dent Hyg. 2015;13:117–124.
- Gluch JI. As an adjunct to tooth brushing,interdental brushes (idbs) are more effective in removing plaque as comparedwith brushing alone or the combination use of tooth brushing and dental floss. J Evid BasedDent Practice. 2012;12:81–88.
- Slot De, Dorfer Ce, Van der Weijden GA. Theefficacy of interdental brushes on plaque and parameters of periodontalinflammation: a systematic review. Int J Dent Hygine, 2008;6:253–264.
- Rasines G. The use of interdental brushes alongwith toothbrushing removes most plaque. Evid Based Dent. 200;10:74.
- Abouassi T, Woelber JP, Holst K, et al. Clinicalefficacy and patients’ acceptance of a rubber interdental bristle. A randomizedcontrolled trial. Clin Oral Investig. 2014;18:1873–1880.
- Hoenderdos NL, Slot DE, Paraskevas S, Van derWeijden GA. The efficacy of woodsticks on plaque and gingival inflammation: asystematic review. Int J Dent Hyg. 2008;6:280–289.
- Hussein A, Slot DE, Van der Weijden GA. Theefficacy of oral irrigation in addition to toothbrush on plaque and clinicalpaprameters of periodontal inflammation: a systematic review. Int J Dent Hyg. 2008;6:304–314
- Jin L. Is oral irrigation beneficial to gingivalhealth as an adjunct to toothbrushing? Evid Based Dent. 2009;10:40–41.
- Wilder RS, Bray KS. Improving periodontaloutcomes: merging clinical and behavioral science. Periodontol2000. 2016;71:65–81.
- Grusovin MG, Coulthard P, Worthington HV, GeorgeP, Esposito M. Interventions for replacing missing teeth: maintaining andrecovering soft tissue health around dental implants. Cochrane DatabaseSyst Rev. 2010;8:CD003069.
- Lyle DM, Goyal CR, Qaqish JG, Schuller R.Comparison of water flosser and interdental brush on plaque removal: asingle-use pilot study. J Clin Dent. 2016;27:23–26.
- Goyle CR, Lyle DM, Qaqish JG, Schuller R. Evaluationof the plaque removal efficiacy of a water flosser compared to string floss inadults after a single use. J Clin Dent. 2013;24:37–42.
- Boyle P, Koechlin A, Autier P. Mouthwash use andthe prevention of plaque, gingivitis and caries. Oral Dis. 2014;20:1–68.
- Zimmer S, Korte P, Verde P, Ohmann C, Naumova E,Jordan RA. Randomized controlled trial on the efficacy of new alcohol-freechlorhexidine mouthrinses after 8 weeks. Int J Dent Hyg. 2015;13:110–116.
- Gunsolley JC. Clinical efficacy of antimicrobialmouthrinses. J Dent. 2010;38(Suppl 1):S6–S10.
- Van der Weijden FA, Van der Sluijs E, Ciancio SG,Slot DE. Can chemical mouthwash agents achieve plaque/gingivitis control? Dent Clin NorthAm. 2015;59:799–829.
- Serrano J, Escribano M, Roldan S, Martin C,Herrara D. Efficacy of adjunctive anti-plaque chemical agents in managinggingivitis: a systematic review and meta analysis. J Clin Perio. 2015;42:S106–S138.
- Karpinski TM, Szkaradkiewicz AK. Chlorhexidene—pharmaco-biologicalactivity and application. Eur Rev Med Pharmacol Sci. 2015;19:1321–1326.
- Drisko CL. Periodontal self-care: evidence-basedsupport. Periodontology 2000. 2013;62:243–255.
- Araujo MW, Charles CA, Weinstein RB, et al.Meta-analysis of the effect of an essential oil-containing mouthrinse ongingivitis and plaque. J Am Dent Assoc. 2015;146:610–644.
- Vlachojannis C, Al-Ahmad A, Hellwig E, ChrubasikS. Listerine® Products: An Update on the Efficacy and Safety. Phytother Res. 2016;30:367–373.
- Hase JC, Attström R, Edwardsson S, Kelty E, KischJ. 6-month use of 0.2% delmopinol hydrochloride in comparison with 0.2%chlorhexidine digluconate and placebo. Clin Periodontol, 1998;25:746–753.
- Smiley CJ, Tracy SL, Abt E, et al. Evidencebased clinical practice guideline on the nonsurgical treatment of chronicperiodontitis by means of scaling and root planing with or without adjuncts.J Am Dent Assoc. 2015;146:525–35.
- Jepsen S, Deschner J, Braun A, Schwarz F,Eberhard J. Calculus removal and the prevention of its formation. Periodontol2000. 2011;55:167–188.
- Wilson TG, Harrel SK, Nunn ME, Francis B, WebbK. The relationship between the presence of tooth-borne subgingival depositsand inflammation found with a dental endoscope. J Periodontol. 2008;79:2029–2035.
- Checchi L, Montevecchi M, Checchi V, Zappulla F.The relationship between bleeding on probing and subgingival deposits. Anendoscopical evaluation. Open Dent J. 2009;3:154–160.
- Heitz-Mayfield LJ, Trombelli L, Heitz F, Needleman I, Moles D. A systematic review of the effect of surgicaldebridement vs non-surgical debridement for the treatment of chronicperiodontitis. J Clin Periodontol. 2002;29:92–102.
- Hung HC, Douglass CW. Meta analysis of theeffect of scaling and root planing, surgical treatment and antibiotic therapieson periodontal probing depth and attachment loss. J Clin Periodontol.2002;29:975–986.
- Scarf S, Wohlfeil M, Siegelin Y, Schacher ZB,Dannewitz B, Eickholz P. Clinical results after nonsurgical therapy inaggressive and chronic periodontitis. Clin Oral Invest. 2014;18:453–460.
- Serino G, Rosling B, Ramberg P, Socransky SS,Lindhe J. Initial outcome and long-term effect of surgical and non-surgicaltreatment of advanced periodontal disease. J Clin Periodontol.2001;28:910–916.
- Huynh-Ba G, Kuonen P, Hofer D, Schmid J, Lang NP,Salvi GE. The effect of periodontal therapy on the survival rate and incidenceof complications of multirooted teeth with furcation involvement after anobservation period of at least 5 years: a systematic review. J ClinPeriodontol. 2009;36:164–176.
- Walmsley AD, Lea SC, Landini G, Moses AJ.Advances in power driven pocket/root instrumentation. J Clin Periodontol.2008;35:22–28.
- Krishna R, De Stefano JA. Ultrasonic vs. handinstrumentation in periodontal therapy: clinical outcomes. Periodontol 2000.2016;71:113–127.
- Hodges KO. Hand-activated instrumentation. Conceptsin Nonsurgical Periodontal Therapy. Independence, Kentucky: DelmarPublishers;1998.
- Osborn JB, Lenton PA, Lunos SA, Blue CM.Endoscopic vs tactile evaluation of subgingival calculus. J Dent Hyg.2014;88:229–236.
- Poppe K, Blue C. Subjective pain perceptionduring calculus detection with use of a periodontal endoscope. J Dent Hyg.2014;88:114–123.
- Michaud RM, Schoolfield J, Mellonig JT, MealeyBL. The efficacy of subgingival calculus removal with endoscopy-aided scalingand root planing: a study on multirooted teeth. J Periodontol.2007;78:2238–2245.
- Geisinger ML, Mealey BL, Schoolfield J, MellonigJT. The effectiveness of subgingival scaling and root planning: An evaluationof therapy with and without the use of the periodontal endoscope. JPeriodontol. 2007;78:22–28.
- Moreno CS, Santos A, Nart J, Levi P, VelasquezA, Sanz MJ. Evaluation of root surface microtopography following the use offour instrumentation systems by confocal microscopy and scanning electronmicroscopy: an in vitro study. J Periodontal Res. 2012;47:608–615.
- Graetz C, Plaumann A,Wittich R, et al. Removal of simulated biofilm: an evaluation of the effect onroot surfaces roughness after scaling. Clin Oral Investig.2017;21:1021-1028.
Featured photo by PEOPLEIMAGES/E+/GETTY IMAGES PLUS
From Dimensions of Dental Hygiene. December 2017;15(12):35-37.




[…] A team of engineers, dentists, and biologists from the University of Pennsylvania has developed an army of tiny robots that can access hard-to-reach areas of the mouth for plaque and biofilm removal. […]