CHERRYBEANS/ISTOCK/GETTY IMAGES PLUS
CHERRYBEANS/ISTOCK/GETTY IMAGES PLUS
The Role of Dental Hygienists in Addressing Sleep Breathing Disorders
These clinicians are uniquely positioned to provide screening, compliance support, and education on treating these common health problems.
This course was published in the December 2020 issue and expires December 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define obstructive sleep apnea (OSA), sleep breathing disorders, and current screening methods.
- Discuss standard and adjunctive treatments for individuals with sleep breathing disorders.
- Identify the connection between untreated sleep breathing disorders and systemic health conditions.
- Describe the unique strengths of dental hygienists to educate patients about sleep breathing disorders.
Obstructive sleep apnea (OSA) is a sleep breathing disorder characterized by severe hypoxia, or periods when an individual does not get enough oxygen during sleep.1 Upper airway resistance syndrome (UARS) is classified beneath the umbrella of OSA syndrome.2 The apnea-hypopnea index (AHI) is a scale used to classify OSA severity based on the number of oxygen desaturations per hour during an overnight sleep study.3 Using the AHI scale to indicate OSA severity, a minimum of five respiratory events per hour is needed to determine mild OSA.2,3 At the opposite extreme, more than 30 events per hour indicate severe OSA.3 These drops in oxygen can be complete, indicating an apnea, or partial, indicating hypopnea.3 UARS is marked by more hypopneas than apneas on the AHI.3 These episodes put an individual at risk for systemic conditions and inadequate healing.1
This article will focus on screening for sleep breathing disorders in the dental setting, treatments for these issues, and the role of dental hygienists in detecting sleep disorders.
Screening Tools
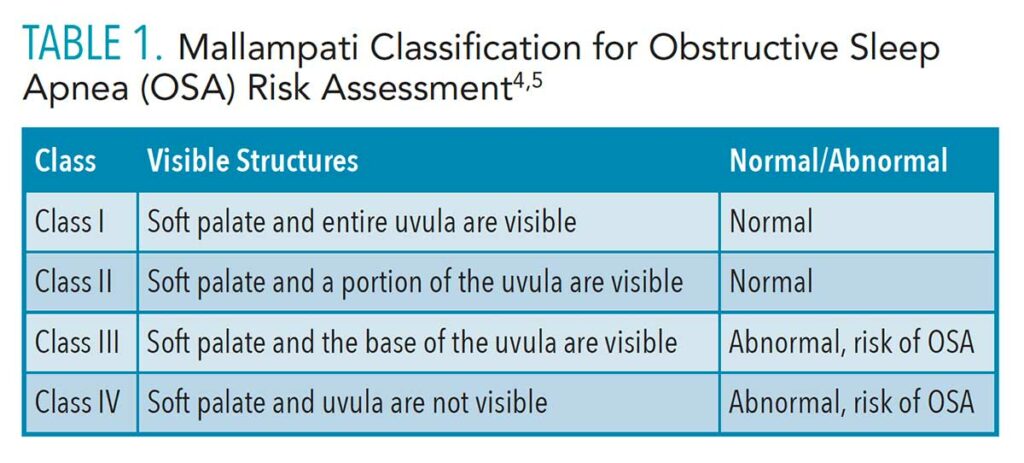
Several screening methods are available for OSA and other sleep breathing disorders. The Mallampati Airway Classification is used by anesthesiologists to score ease of intubation, which is a risk predictor for sleep apnea.1 To use the Mallampati Airway Classification, patients stick out their tongues and the clinician evaluates their airway based on the visibility of the palate and uvula (Table 1).4,5
Research shows that dental hygiene students are capable of accurately classifying a patient’s Mallampati score. In a study of dental hygiene students in which the control used was the supervising dentist’s assessment of Mallampati score, Kandray et al1 found that dental hygiene students showed a 77% agreement between the students’ and dentist’s classifications.
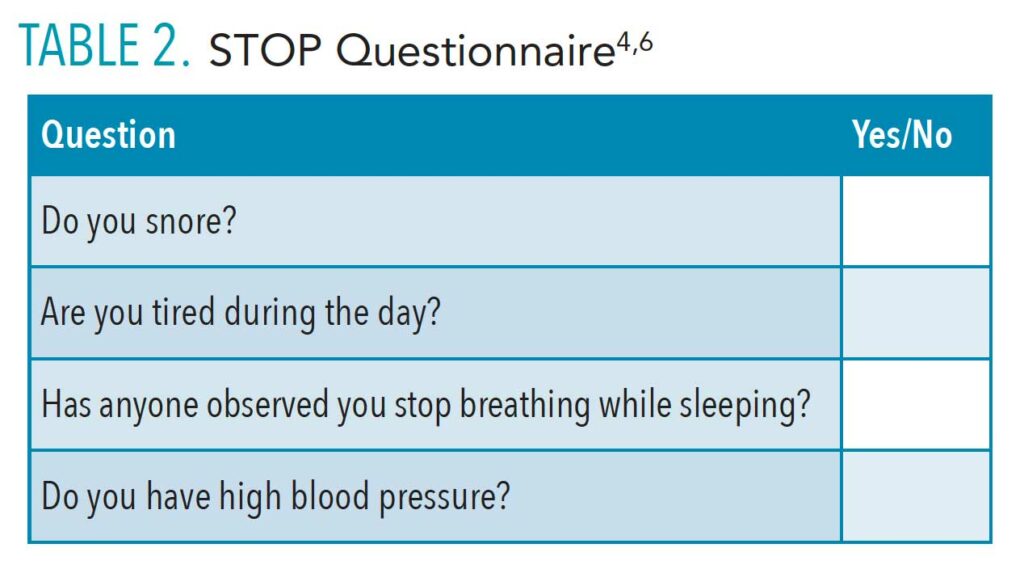
The STOP Questionnaire (Table 2) and the STOP-Bang Questionnaire are simple tools that can quickly indicate elevated risk for sleep breathing disorders. Both ask questions regarding snoring, fatigue, and whether the patient stops breathing during sleep, in addition to questions regarding systemic health. The STOP-Bang Questionnaire goes more in-depth with questions regarding gender, body mass index, and neck circumference. “Yes” answers to three or more questions indicate high risk of sleep breathing disorders.4,6
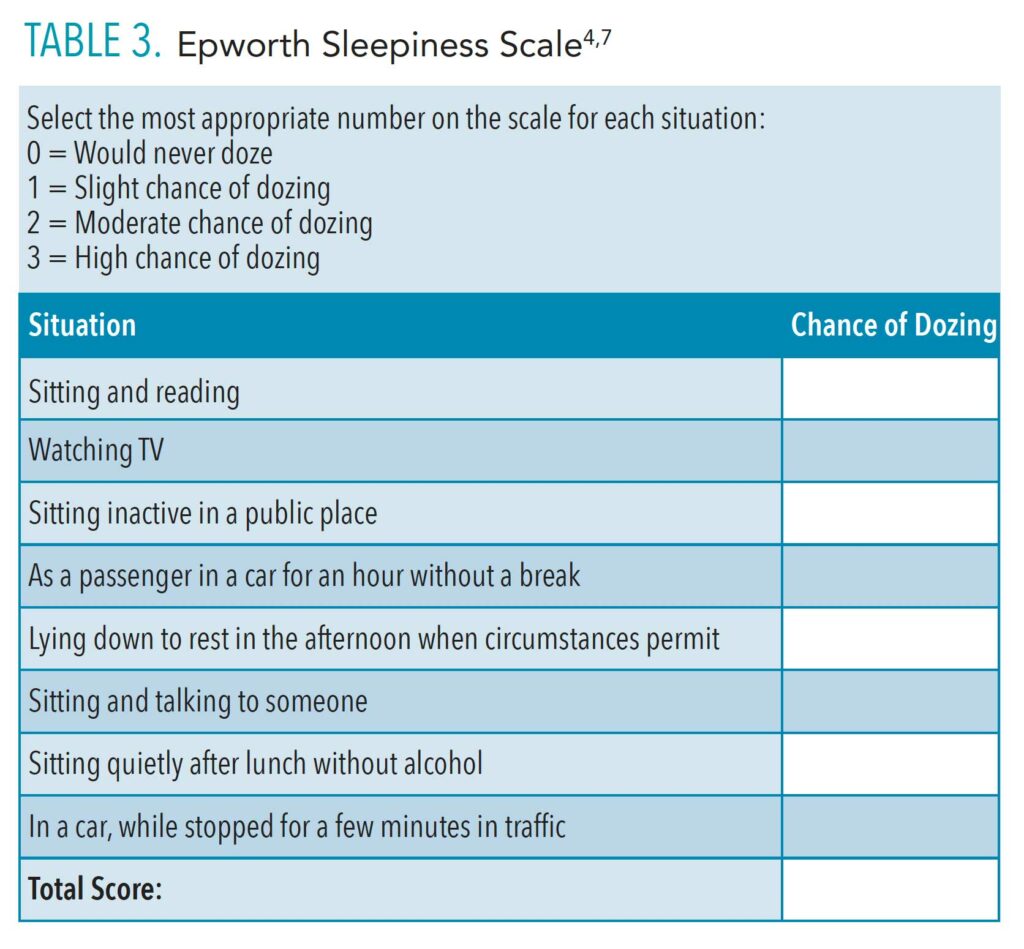
The Epworth Sleepiness Scale (Table 3) is a questionnaire that patients complete themselves that asks questions regarding how fatigued they are during the day. Patients who score 16 or higher are at risk for sleep breathing disorders.4,7
These screening tools could easily be added to a traditional extraoral/intraoral cancer screening and provide a basis for patient discussion of sleep breathing disorder risk as well as discussion of possible treatments.
Facial Dimensions and Upper Airway Resistance
Certain oral characteristics and facial dimensions are associated with increased risk for OSA, offering yet another tool to help dental hygienists in screening for sleep breathing disorders. Lee et al8 determined that a patient’s mid-face and lower-face width are highly associated with predicting tongue volume, often a main factor in lower airway obstruction. The thickness and volume of the mid-face and upper airway soft tissue correlate with the potential for airway narrowing or possible airway obstruction. Similar facial dimensions and airway architecture are evident in patients with OSA.8 As such, subtypes of patient facial dimension may be used to develop better treatment tools and screening protocols for OSA and other sleep breathing disorders.8 With the tools to screen both intraoral and extraoral characteristics, dental hygienists may be able to improve screening efficiency, increase follow-up, and decrease incidence of related systemic diseases.
Standard and Adjunctive Treatments
Treatment for OSA varies depending on the severity of the disorder. Severity is assessed using data gathered during a sleep study. The sleep study, or polysomnography, is considered the gold standard for diagnosing sleep breathing disorders.9,10 Various treatments are implemented depending on individual levels of severity and patient compliance. Treatments include continuous positive airway pressure (CPAP), mandibular advancement splint (MAS) therapy, tongue stabilizing devices, and myofunctional therapy.11 However, compliance with CPAP therapy is low. Surgical procedures are also available, however, they are not as effective as CPAP treatment.9 More data are needed to determine efficacy of available treatments.
Myofunctional therapy has been shown to reduce snoring intensity and the amount of time spent snoring for patients with OSA.12 Even in children where compliance with myofunctional therapy can be low, passive therapy with an oral appliance used at night showed decreases in the AHI and a lower percentage of respiratory-related arousals among children who were born full-term.13 Evidence shows children born prematurely may have a decreased AHI during rapid eye movement (REM) sleep and a low mean heart rate when using a nightly oral appliance.13 Myofunctional therapy has also been investigated as an adjunct therapy with a CPAP machine, and it has been shown to improve CPAP compliance and strengthen tongue and soft palate muscle tone.11
Systemic Disease Connection
The relationship between sleep apnea and systemic disease has been well documented. Patients with mild to moderate OSA treated with a MAS for 1 year showed improvement in arterial stiffness, glucose control, and insulin resistance.14 A significant correlation has been shown between periodontitis and OSA, although more research is needed.15 Hypertension is also associated with patients who have OSA.16 Specifically the higher the AHI score during REM sleep, the higher the prevalence of hypertension.16 In sleep cycles other than REM, the AHI does not show an association with hypertension.16 Perhaps future studies will shed light on the importance of CPAP devices and other interventions specifically during REM sleep. Additionally, a recent meta-analysis on the incidence of cancer in patients with OSA showed that even after controlling for other cancer risk factors, a significantly higher incidence of cancer was seen in patients with OSA when compared to patients without the condition.17
Screenings for sleep breathing disorders in the dental operatory could result in patients being identified, diagnosed, and treated at earlier stages, possibly preventing comorbidities. Dental hygienists already screen for hypertension during a routine dental visit. Discussion of hypertension, its connection to OSA and other sleep breathing disorders, and individual patient oral architecture, combined with OSA screening, fit well into a dental hygienist’s role in patient education. While the need for consensus on a single screening protocol is still being sought, any screening provided by dental hygienists has the potential to ensure patients receive early diagnosis and treatment for sleep breathing disorders. The connection between systemic diseases and untreated sleep breathing disorders and the need for a uniform multidisciplinary approach to diagnosis and treatment leads to tremendous opportunity for the dental hygiene profession.
Dental Hygiene’s Strengths
Bridging the gap between what has been demonstrated in research and what is practical in the clinic setting is crucial to patient treatment success. Patient differences in preference, compliance, and interest level are all factors with which dental hygienists are familiar. Daily, dental hygienists tailor treatment and education to each patient’s unique needs. The dental hygiene profession is prevention-minded and has more time available per patient than other health professionals to educate patients concerning chronic diseases. OSA and other sleep breathing disorders are chronic conditions that benefit from early intervention. The strengths of the dental hygiene profession, including significant time spent with patients, focus on prevention, development of long-term relationships with patients, expertise in patient education and screening, emphasize its natural role in increasing the efficiency of OSA diagnosis and treatment.
To identify OSA risk and reduce the impact of UARS, dental hygienists can use their observation skills during the extraoral and intraoral examination to identify a patient’s risk. Dental hygienists are trained to visualize and evaluate the oropharynx and identify premolar extraction, palatal formation, and other architectural features of the mouth. They can play a key role in educating patients about the nasal sinus, its location, and how the size of this space can predispose patients to UARS. Dental hygienists can then refer the patient to an otolaryngologist for further evaluation of the upper airway and identification of airway interferences, including deviated septum, enlarged turbinates, and other interferences that could impede airflow.
The ability of other health professionals to identify patients at risk for sleep breathing disorders has been studied. Pharmacists were able to correctly match between 21.4% and 67% of patients to their OSA risk level.18 The theory behind such a study is that pharmacists are easily accessed and underutilized in referring patients to physicians. The same argument can be applied to dental hygienists, who are underutilized in many states where they are unable to practice to the full extent of their training.19 However, pharmacists often work 12-hour shifts and are unlikely to have a full hour to work on patient education or develop a therapeutic patient-provider relationship as dental hygienists routinely do.
While in many states dental hygienists must work under the direct or indirect supervision of a dentist, in other states they are able to initiate referrals, conduct examinations, and own their own practices.19 Collaboration with dentists is always important; however, this does not prevent a dental hygienist from discussing the possibility of referral with patients. Dental hygienists may make referrals for hypertension or lesions found during an oral cancer screening. In the same way, dental hygienists have a duty, once trained, to discuss and screen for sleep breathing disorders in their patients. This screening can be aided by questions concerning snoring and sleep disturbances on the medical history.
Increasing Treatment Compliance
Patient compliance is a daily challenge for oral health professionals. Struggling with compliance is also a common concern for patients using CPAP to treat their sleep breathing disorder.10 When upper and nasal airway obstruction has been ruled out, patients have mild to moderate OSA, or have difficulty tolerating CPAP treatment, a mandibular advancement splint (MAS) is a good alternative.10
Dental hygienists who are educated in screening for OSA and MAS can help educate patients who do not tolerate the CPAP. If risk for OSA and other sleep breathing disorders is identified earlier and more broadly by dental hygienists, there is potential to positively impact treatment of this disease and quality of life for those affected.20
Multidisciplinary Screening Approach
Perhaps the absence of a standard protocol among interdisciplinary health professions is one of the main reasons why current treatment options for sleep breathing disorders are not broadly adopted. Additionally, there is a disconnect between polysomnography data, which are used to inform practitioners of the diagnosis and severity of OSA, and the efficacy of MAS therapy in patient treatment.21 Based on current literature, demographic, anthropometric, and polysomnographic data do not predict the efficacy of MAS devices.21 Polysomnography does not reliably predict or correlate with MAS efficacy in aiding breathing. An alternative or additional test for predicting efficacy of MAS therapy is needed.21 Other metrics commonly measured with polysomnography include respiratory related arousals and respiratory disturbance index.3
The need for standardization of diagnosis and treatment is clear. Creating protocols and standards across disciplines adds organization and clarity to multidisciplinary communication.22 Ten Berge et al22 found that a structured clinical follow-up between medical and dental teams reduced the time lost between sleep apnea diagnosis and treatment by an average of 102 days.
Future Applications
Patient compliance is important in any therapy. Although CPAP is the gold standard for treatment of OSA, it is difficult to tolerate. Polysomnography may de-emphasize other sleep breathing disorders such as UARS. Perhaps this is why severity ratings from polysomnography are unable to predict MAS therapy success. The larger anatomical picture needs to be considered to advance beyond simply treating obstructive airway disease to preventing it and optimizing healing.
Increasing patient access to treatment for sleep breathing disorders and improving REM sleep can reduce hypertension risk, and aid in the prevention and management of other chronic inflammatory diseases.14–16 Teaching risk evaluation for sleep breathing disorders in dental hygiene education is one component of the multidisciplinary solution needed to improve the early identification of OSA and other sleep breathing disorders. Curriculum on the disease process of OSA, treatment options, and oral appliance therapy has already been developed.3 This curriculum could be adapted and edited depending on a student’s clinical practice level.
Teaching screening protocols for sleep breathing disorders in dental hygiene schools is a powerful way to impact patient health and wellness. The need and importance of treatment referral for undiagnosed disease is an opportunity that should not be missed. The challenge will be further refining screening protocols based on diligent research.
References
- Kandray DP, Juruaz D, Yacovone M, Chang GA. Inter-rater reliability of the mallampati classification for patients in a dental hygiene clinic. J Dent Hyg. 2013;87:134–139.
- Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Darien, Illinois: American Academy of Sleep Medicine; 2014.
- Güneri P, İlhan B, Çal E, Epstein JB, Klasser GD. Obstructive sleep apnoea and the need for its introduction into dental curricula. Eur J Dent Educ. 2016;21:121–129.
- Kornegay E. Addressing obstructive sleep apnea. Dimensions of Dental Hygiene. January 2017;15(1):38-41.
- Nuckton TJ, Glidden DV, Browner WS, Claman DM. Physical examination: mallampati score as an independent predictor of obstructive sleep apnea. Sleep. 2006;29:903–908.
- Chung F, Yegneswaran B, Liao P, et al. STOP Questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812–821.
- Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–545.
- Lee RWW, Sutherland K., Chan ASL, Zeng B, et al. Relationship between surface facial dimensions and upper airway structures in Obstructive Sleep Apnea. Sleep. 2010;33:1249–1254.
- de Godoy LBM, Palombini LO, Guilleminault C, Poyares D, Tufik S, Togeiro SM. Treatment of upper airway resistance syndrome in adults: Where do we stand? Sleep Sci. 2015;8:42–48.
- Sutherland K, Phillips CL, Davies A, et al. A. CPAP pressure for prediction of oral appliance treatment response in obstructive sleep apnea. J Clin Sleep Med. 2014;10:943–949.
- Diaferia G, Santos-Silva R, Truksinas E, et al. Myofunctional therapy improves adherence to continuous positive airway pressure treatment. Sleep Breath. 2015;21:387–395.
- Camacho M, Guilleminault C, Wei JM, et al. Oropharyngeal and tongue exercises (myofunctional therapy) for snoring: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2018;275:849–855.
- Chuang L, Lian Y, Hervy-Auboiron M, Guilleminault C, Huang Y. Passive myofunctional therapy applied on children with obstructive sleep apnea: a 6-month follow-up. J Formos Med Assoc. 2017;116:536–541.
- Galic T, Bozic J, Ivkovic N, Gunjaca G, Ticinovic, TK, Dogas Z. Effects of mandibular advancement device treatment on arterial stiffness and glucose metabolism in patients with mild to moderate obstructive sleep apnea: A prospective 1-year study. Sleep Breath. 2015;20:69–77.
- Al-Jewair TS, Al-Jasser R, Almas K. Periodontitis and obstructive sleep apnea’s bidirectional relationship: a systematic review and meta-analysis. Sleep Breath. 2015;19:1111–1120.
- Mokhlesi B, Finn L, Hagen E, et al. Obstructive sleep apnea during REM sleep and hypertension results of the Wisconsin sleep cohort. Am J Respir Crit Care Med. 2014;190:1158–1167.
- Palamaner Subash Shantha G, Kumar AA, Cheskin LJ, Pancholy SB. Association between sleep-disordered breathing, obstructive sleep apnea, and cancer incidence: a systematic review and meta-analysis. Sleep Med. 2015;16:1289–1294.
- Cawley MJ, Warning II WJ. A systematic review of pharmacists performing obstructive sleep apnea screening services. Int J Clin Pharm. 2016;38:752–760.
- Dental Hygiene Practice Act Overview Permitted functions and supervision levels by state. Available at: adha.org/resources-docs/7511_Permitted_Services_Supervision_Levels_by_State.pdf Accessed September 20, 2018.
- Lee W, Lee S, Ryu HU, Chung Y, Kim WS. Quality of life in patients with obstructive sleep apnea: Relationship with daytime sleepiness, sleep quality, depression, and apnea severity. Chron Resp Dis. 2016; 13:33-39.
- Sutherland K, Takaya H, Qian J, Petocz P, Ng AT, Cistulli PA. Oral Appliance Treatment Response and Polysomnographic Phenotypes of Obstructive Sleep Apnea. J Clin Sleep Med. 2015;11:861–868.
- Ten Berge DM, Braem MJ, Altenburg A, Dieltjens M, Van de Heyning PH, Vanhaecht, K., & Vanderveken, O. M. Evaluation of the impact of a clinical pathway on the organization of a multidisciplinary dental sleep clinic. Sleep and Breath. 2014;18:325–334.
From Dimensions of Dental Hygiene. December 2020;18(11):32-35.