 KTSTOCK / ISTOCK / GETTY IMAGES PLUS
KTSTOCK / ISTOCK / GETTY IMAGES PLUS
Oral Cancer Prevention
A combination of brief motivational interviewing and vaccination counseling can reduce risk for human papillomavirus-related oropharyngeal cancers.
This course was published in the July 2022 issue and expires July 2025. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the incidence of human papillomavirus-related oropharyngeal cancers (HPV-OPCs), common locations for lesions, and epidemiologic risk factors.
- Explain the dental hygienist’s role in providing HPV-OPC prevention counseling and HPV vaccine advocacy in dental settings.
- Describe effective communication strategies when discussing HPV-OPCs and HPV vaccine uptake with patients and parents/caregivers.
The incidence of human papillomavirus-related oropharyngeal cancers (HPV-OPCs) continues to rise. As this is the most common HPV-related cancer in the United States,1 the American Dental Association and American Academy of Pediatric Dentistry support advocacy for HPV prevention, as well as administration of the HPV vaccine in dental settings.2,3 Dental hygienists may serve an instrumental role in screening and providing patient-centered counseling for the prevention of HPV-OPCs.
The challenges in screening for HPV-OPC and prevention counseling are twofold. First, screening during intraoral examinations is challenging due to the limited visibility of the lesion(s), which are generally located in the posterior oropharyngeal area. Common locations for HPV-OPCs are the base of the tongue, soft palate, and tonsillar crypts. The lack of a precursor lesion and adequate diagnostic technology add to the difficulty of early stage identification.1 Second, oral health professionals report a lack of knowledge, comfort, confidence, and training for HPV-OPC screening and prevention counseling.4–7 Research demonstrates adults and parents/caregivers of adolescents are generally comfortable and expect HPV-OPC prevention counseling and vaccine advocacy from oral health professionals.8,9
The increased momentum to provide HPV-OPC prevention counseling and advocate for HPV vaccine acceptance in dental offices has highlighted the need for additional training. Clinicians have reported a willingness to receive training in HPV communication and vaccine advocacy.5,7,10 In order to counsel patients effectively in the prevention of HPV-related cancers, providers need skills-based HPV-OPC communication training. This should include HPV epidemiology, OPC signs and symptoms, OPC screening techniques, immunization dosing schedules, trends in vaccine acceptance, and evidence-based communication strategies so clinicians feel confident in their role in HPV-OPC prevention.
Human Papillomavirus-Related Oropharyngeal Cancers and Asymptomatic Individuals
Individuals with HPV frequently do not experience symptoms. Of the more than 200 distinct types of HPV, most are considered low risk. While low-risk types can cause skin and anogenital warts, they do not cause cancer. High-risk types are those that can cause cancer. Most infections are cleared by the immune system within 2 years of infection, but remain active until cleared.11 The virus can still be spread through skin-to-skin sexual contact in asymptomatic individuals during the active phase.11 High-risk types, such as HPV-16 and HPV-18, may persist for several decades with no symptoms, eventually developing into cancer.12
Currently, HPV causes 70% to 80% of OPCs in the US, with incidence rates increasing more rapidly than most other cancers.1,13,14 Recent trends show an alarming increase in HPV-OPC incidence among non-Hispanic white men, and men age 65 and older, with a rise in mortality due to later stage diagnosis.1
Cases of HPV-positive OPCs are distinct from HPV-negative OPCs, with different epidemiologic factors, molecular biology, symptoms, and outcomes. Epidemiologic factors associated with HPV-OPCs include male gender, higher socioeconomic status, younger age at sexual debut, and multiple oral sex partners.14 
Human Papillomavirus Vaccination
A 9-valent HPV vaccine is currently available (Gardasil 9). The vaccine is effective against nine types of HPV, including those that cause anogenital warts and seven high-risk types responsible for most cases of HPV-OPC.15 The US Food and Drug Administration (FDA) and Advisory Committee on Immunization Practices (ACIP) are responsible for ensuring HPV vaccine safety and efficacy. The vaccine was approved by the FDA for females between the ages of 9 and 26 in 2006 to prevent cervical cancer and genital warts, and for males between the ages of 9 and 26 in 2009 to prevent genital warts.16 The ACIP recommends adolescents receive the vaccine between the ages of 11 and 12, with a “catch up” schedule between 13 years and 26 years of age.17
As new research becomes available, the FDA continues to expand its approved indications for the HPV vaccine. In 2018, it expanded indications to include adults up to age 45 who may not be adequately vaccinated. A further expansion in 2020 added OPC prevention as an indication.18 The ACIP recommends that individuals older than 26 receive the vaccine only after a shared decision-making process with their healthcare provider.19 The vaccine is administered as a two-dose series (0, and 6-month to 12-month schedule) before the age of 15, and a three-dose series (0, 1-month to 2-month, and 6-month schedule) for individuals 15 and older, as well as those who are immunocompromised.15
Despite the availability of this cancer-preventing vaccine, patient uptake is well below the national target of 80% completion rates for adolescents ages 13 years to 15 years, and has remained stagnant at 48% since 2015.20 Additionally, the COVID-19 pandemic has negatively impacted HPV vaccine rates of adolescents, with a substantial reduction in acceptance observed during 2020.21 Simulation-based models predict an increase between 600 and 6,200 cases of HPV-OPC due to the decline in vaccine acceptance during the COVID-19 pandemic.1 The low HPV vaccine compliance statistics can be attributed to several factors, mainly parental safety concerns.22 Other factors include a lack of knowledge and absence of provider recommendation.22,23 Oral health professionals are key players in HPV-OPC prevention by using an evidence-based approach to educate patients in plain terms that desexualize HPV transmission and advocate for immunization against HPV-related OPCs.
Motivational Interviewing
Motivational interviewing (MI) is a collaborative, patient-centered counseling approach to evoke a patient’s intrinsic motivation for positive behavior change.24,25 A derivative of MI—brief motivational interviewing— has been used by oral health professionals with limited time (5 minutes to 10 minutes) for patient counseling.26,27
Communication training using MI for the prevention of HPV-OPCs and advocacy for the HPV vaccine began in medical settings. Medical providers were able to increase their MI knowledge and reported this technique as a useful approach to counseling.4,28 In a medical setting, MI helped promote HPV vaccine uptake.4,23,28 In dental educational settings, brief MI has been documented as an effective communication tool in skills-based training for the prevention of HPV-OPCs and promotion of the HPV vaccine. In short, brief MI training helps prepare students to counsel patients effectively.29–31
It is important for clinicians to apply the “spirit of MI” during brief MI sessions. This is a philosophy that helps establish patient-provider rapport and trust.24 There are four integrated components: collaboration, compassion, acceptance, and evocation. Using the spirit of MI supports patient autonomy,24 which is necessary due to the sensitive nature of HPV-OPC conversations. Effective use of brief MI is grounded in MI principles, strategies and rules that assist clinicians when implementing the elicit-provide-elicit (E-P-E) technique.
Fundamental Principles
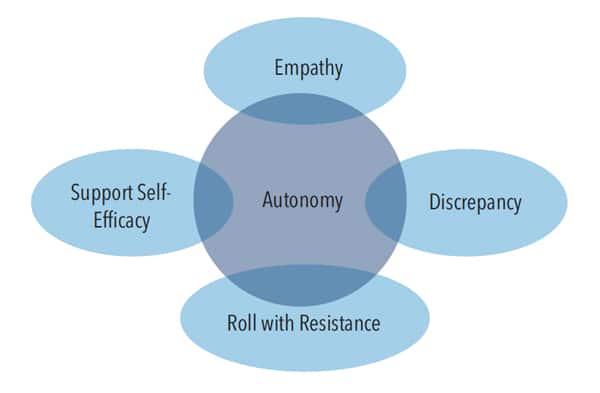
To assist patients in maintaining their autonomy during brief MI sessions, clinicians should follow four key MI principles (Figure 1). Empathy focuses on the provider’s ability to show understanding of patients’ perceptions of HPV-OPCs and the HPV vaccine.25,30 Developing discrepancy helps patients distinguish between their values and behaviors that are inconsistent with these values—and may actually increase risk of HPV-OPCs.25,30 Rolling with resistance is avoiding conflict during HPV-OPC and HPV vaccine conversations.25,30 This is crucial given the high rate of vaccine hesitancy.22 Self-efficacy provides encouraging affirmations to build self-confidence in patients’ actions toward the prevention of HPV-related cancers.25,30 Oral health professionals who follow these MI principles and present evidence-based facts effectively support patient autonomy.
Guiding Strategies
There are eight strategies for brief MI counseling that will enhance providers’ ability to follow MI principles and encourage patient autonomy (Table 1).24,25,30 Of these, clinicians who are beginning to apply brief MI may wish to focus on open questions, affirmations, reflections, and summaries (OARS). Open-ended questions give patients an opportunity to respond and provide insight on their perceptions about HPV-OPCs and the HPV vaccine.24,25,30 Affirmations are used to encourage patients and acknowledge their knowledge, awareness, or perceptions without judgement.24,25,30 Reflections allow clinicians to demonstrate their understanding of patients’ perceptions and potential ambivalence toward HPV vaccination.24,25,30 Since oral health professionals have limited time during appointments, summaries are required to close the brief MI session. Summaries provide a final opportunity to demonstrate an understanding of patients’ perceptions of HPV-OPCs and the HPV vaccine following clinical counseling.24,25,30
Rules to Follow
Clinicians applying brief MI for HPV-OPC prevention and HPV vaccine counseling are advised to follow the four MI rules that align with the technique’s principles. The first is to “resist the righting reflex;” this means providers should not lecture patients.24,25 The clinician’s role is to evoke and initiate conversations designed to change behaviors that raise risk levels. The second rule is to “understand” the patient’s perceptions of HPV-OPCs and the HPV vaccine.24,25,30 The third is to “listen” with empathy, as this demonstrates compassion for the patient’s perceptions of his or her risks for HPV-OPCs and/or acceptance of the HPV vaccine.24,25,30 The fourth rule is to “empower” the patient to support autonomy.
Elicit-Provide-Elicit
The E-P-E approach helps providers keep within the 5-minute to 10-minute limits for a brief MI session. The E-P-E technique enhances understanding of the patient’s awareness. It also lets clinicians seek permission before providing or sharing information, and elicit the patient’s motivation and readiness for change.24,30,32,33 The first step is to elicit what the patient already knows about HPV-OPCs and the HPV vaccine by asking evocative, open-ended questions.24,30,32 This is essential before providing information on related cancers or the vaccine to avoid giving unwanted information or details the patient already knows.
The next step is to provide information, with permission to correct misinformation or fill in any gaps.32 Asking permission before sharing particulars supports patient autonomy to lead the discussion on this sensitive topic. Patients may feel uncomfortable with the sexual context of HPV. Lastly, elicit again with open-ended questions to gain insight and perceptions on the information provided.30,32 The E-P-E approach saves time, validates the patient’s knowledge, and presents an opportunity to explore ambivalence toward the HPV vaccine.
Getting Started
Oral health professionals need accurate knowledge of HPV transmission, prevention strategies, and the risks/benefits of the HPV vaccine to enhance their comfort and confidence in counseling patients about HPV-OPCs. Training in brief MI techniques should include coaching, role-playing, and feedback for skill retention.29–31 Clinicians interested in improving their HPV counseling skills should seek out continuing education courses (including this article) and online learning modules covering HPV-OPC and the HPV vaccine. Fact sheets (available from several sources) serve as helpful, age-appropriate educational aids.34,35 Having HPV fact sheets available in multiple languages is an excellent way to initiate BMI sessions. These tools provide a tangible resource for patients and help clinicians evoke patient perceptions of HPV-OPCs and the HPV vaccine.
The Motivational Interviewing Network of Trainers is an excellent resource for those seeking training, continuing education, and practice opportunities.36 Stephen Rollnick, PhD,37 a cofounder and pioneer of MI, has a website that offers online courses, webinars, consulting, mentoring and books. Another good source is Psychwire, which offers online MI and vaccine hesitancy courses.38
Conclusion
Data show that HPV-related OPC rates are rising, despite the availability of a cancer-preventing vaccine. Vaccination rates are dismal, however, and fall well below national goals. Factors contributing to low vaccination uptake include parental hesitancy and lack of knowledge. Clinical recommendation of the HPV vaccine is positively associated with vaccine acceptance, yet many parents and caregivers report a lack of provider recommendation.
Oral health professionals can play an important role in HPV-OPC prevention through patient education and vaccine advocacy. Patient-centered counseling using MI and brief MI has shown to be an effective approach in HPV communication. Clinicians are encouraged to seek training to improve their knowledge of HPV, and develop skills in MI and brief MI principles, strategies, and rules— for these are the tools that facilitate meaningful and impactful patient discussions about HPV-OPCs and HPV vaccine uptake.
References
- Damgacioglu H, Sonawane K, Zhu Y, et al. Oropharyngeal cancer incidence and mortality trends in all 50 states in the US, 2001–2017. JAMA Otolaryngol Head Neck Surg. 2022;148:155–165.
- American Dental Association. FDA adds oropharyngeal cancer prevention as indication for HPV vaccine. Available at: https://www.ada.org/publications/ada-news/떔/june/fda-adds-oropharyngeal-cancer-prevention-as-indication-for-hpv-vaccine#:~:text=The%20ADA%20adopted%20a%20policy,HPV%20associated%20with%20oropharyngeal%20cancer. Accessed May 11, 2022.
- American Academy of Pediatric Dentistry. Policy on human papilloma virus vaccinations. The Reference Manual of Pediatric Dentistry. Chicago, Ill: American Academy of Pediatric Dentistry; 2021:106–107.
- Reno JE, Thomas J, Pyrzanowski J, et al. Examining strategies for improving healthcare providers’ communication about adolescent HPV vaccination: evaluation of secondary outcomes in a randomized controlled trial. Hum Vaccin Immunother. 2019;15:1592–1598.
- Stull CL, Lunos S. Knowledge, attitudes and practices regarding human papilloma virus communication and vaccine advocacy among Minnesota dentists and dental hygienists. J Dent Hyg. 2019;93:33–42.
- Patel S, Koskan A, Spolarich A, Perry M, Flood T. Dental professionals’ knowledge, attitudes, and practice behaviors related to human papillomavirus vaccination. J Public Health Dent. 2020;80:61–69.
- Guadiana D, Kavanagh NM, Squarize CH. Oral health care professionals recommending and administering the HPV vaccine: Understanding the strengths and assessing the barriers. PLoS One. 2021;16:e0248047.
- Daley EM, Thompson EL, Beckstead J, et al. Discussing HPV and oropharyngeal cancer in dental settings: gender and provider-type matter. Hum Vaccin Immunother. 2021;17:5454–5459.
- Stull C, Freese R, Sarvas E. Parent perceptions of dental care providers’ role in human papillomavirus prevention and vaccine advocacy. J Am Dent Assoc. 2020;151:560–567.
- Askelson N, Ryan G, McKernan S, Scherer A, Daly E, Avdic L. A mixed-methods examination of factors related to HPV vaccination promotion in private dental settings, Iowa, 2019. Prev Chronic Dis. 2021;18:E26.
- U.S. Centers for Disease Control and Prevention. HPV Infection. Available at: https://www.cdc.gov/hpv/parents/about-hpv.html. Accessed May 11, 2022.
- Wood ZC, Bain CJ, Smith DD, Whiterman DC, Antonsson A. Oral human papillomavirus infection incidence and clearance: A systematic review of the literature. J Gen Virol. 2017;98:519–526.
- U.S. Centers for Disease Control and Prevention. How Many Cancers Are Linked With HPV Each Year? Available at: https://www.cdc.gov/cancer/hpv/statistics/cases.htm. Accessed May 11, 2022.
- Lechner M, Liu J, Masterson L, Fenton TR. HPV-associated oropharyngeal cancer: epidemiology, molecular biology and clinical management. Nat Rev Clin Oncol. 2022;19:306–327.
- U.S. Centers for Disease Control and Prevention. Human papillomavirus vaccines. Available at: https://www.cdc.gov/vaccines/pubs/pinkbook/hpv.html#vaccines. Accessed May 11, 2022.
- U.S. Food and Drug Administration. FDA approves expanded use of Gardasil 9 to include individuals 27 through 45 years old. Available at: https://www.fda.gov/news-events/press-announcements/fda-approves-expanded-use-gardasil-9-include-individuals-27-through-45-years-old. Accessed May 11, 2022.
- U.S. Food and Drug Administration. Gardasil. Available at: https://www.fda.gov/vaccines-blood-biologics/vaccines/gardasil. Accessed May 11, 2022.
- U.S. Centers for Disease Control and Prevention. Human papillomavirus (HPV) ACIP vaccine recommendations. Available at: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/hpv.html. Accessed May 11, 2022.
- U.S. Centers for Disease Control and Prevention. Human Papillomavirus Vaccination for Adults: Updated Recommendations of the Advisory Committee on Immunization Practices. Available at: https://www.cdc.gov/mmwr/volumes/蒐/wr/mm6832a3.htm. Accessed May 11, 2022.
- Healthy People 2030. Increase the proportion of adolescents who get recommended doses of the HPV vaccine — IID-08 — Data. Available at: https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-adolescents-who-get-recommended-doses-hpv-vaccine-iid-08/data?group=None&state=United+States&from=2018&to=2018&populations=&op=Show+Data#views-exposed-form-hp-data-tables-page-1. Accessed May 11, 2022.
- Daniels V, Saxena K, Roberts C, et al. Impact of reduced human papillomavirus vaccination coverage rates due to COVID-19 in the United States: A model based analysis. Vaccine. 2021;39:2731–2735.
- Sonawane K, Zhu Y, Lin YY, et al. HPV vaccine recommendations and parental intent. Pediatrics. 2021;147:e2020026286.
- Dempsey AF, Pyrznawoski J, Lockhart S, et al. Effect of a health care professional communication training intervention on adolescent human papillomavirus vaccination: a cluster randomized clinical trial. JAMA Pediatr. 2018;172:e180016.
- Miller WR, Rollnick S. The spirit of motivational interviewing. In: Motivational Interviewing Helping People Change. 3rd ed. New York, NY: The Guilford Press; 2013:14–24.
- Catley D, Goggin K, Lynam I. Motivational interviewing (MI) and its basic tools. In: Ramseier CA, Suvan JE. Health Behavior Change in the Dental Practice. Ames, Iowa: Wiley-Blackwell; 2010:59–92.
- Koeber A. Brief interventions in promoting health behavior change. In: Ramseier CA, Suvan JE. Health Behavior Change in the Dental Practice. Ames, Iowa: Wiley-Blackwell; 2010:93–112.
- Gillam DG, Yusuf H. Brief motivational interviewing in dental practice. Dent J (Basel). 2019;7:51.
- Wermers R, Ostroski T, Hagler D. Health care provider use of motivational interviewing to address vaccine hesitancy in college students. J Am Assoc Nurse Pract. 2021;33:86–93.
- Stull CL, Matthews E, Evans M, Arnett MC. Examining the role of HPV communication training in the knowledge, attitudes, comfort, and confidence of dental hygiene students. J Dent Hyg. 2021;95:47–55.
- Arnett MC, Evans MD, Stull CL. Students’ perceptions of the “importance” of and “confidence” with applying brief motivational interviewing during HPV patient counseling. J Dent Hyg. In press.
- Arnett MC, Evans MD, Stull C. Skills-based training: brief motivational interviewing for human papillomavirus communication. J Dent Hyg. In press.
- Wyatt J, Singer A. Clinical Conversations about Cannabis: Using Elicit – Provide – Elicit. Available at: https://motivationalinterviewing.org/sites/default/files/attc_messenger_article-clinical_conv_cann-using_epe-jun_떏-formatted.pdf. Accessed May 11, 2022.
- Suvan J, Fundak A, Gobat N. Implementaion of health behavior change priniciples in dental practice. In: Ramseier CA, Suvan JE. Health Behavior Change in the Dental Practice. Ames, Iowa: Wiley-Blackwell; 2010:113–144.
- Head and Neck Cancer Alliance, American Head and Neck Society. Throat cancer from a virus? Facts you should know. Available at: https://www.headandneck.org/wp-content/uploads/떓/葍/Patient-HPV-Fact-Sheet_Final-1.pdf. Accessed May 11, 2022.
- Team Maureen. Dental Toolkit. Available at: https://www.teammaureen.org/about/materials/. Accessed May 11, 2022.
- About MINT: Motivational Interviewing Network of Trainers. Available at: https://motivationalinterviewing.org/about_mint. Accessed May 11, 2022.
- Stephen Rollnick Trainer Consultant Author and Co-Founder of Motivational Interviewing. Available at: https://www.stephenrollnick.com/. Accessed May 11, 2022.
- Psychwire. William Miller, Stephen Rollnick and Theresa Moyers Teach Motivational Interviewing. Available at: https://psychwire.com/motivational-interviewing. Accessed May 11, 2022.
From Dimensions of Dental Hygiene. July 2022; 20(7)32-35.



