 BANANASTOCK / ISTOCK / GETTY IMAGES PLUS
BANANASTOCK / ISTOCK / GETTY IMAGES PLUS
The Impact of Orofacial Myofunction Disorders on Malocclusion
Orofacial myofunctional disorders and chronic oral dysfunction may increase the risk for dental malocclusion and related craniofacial dysmorphology.
This course was published in the July 2022 issue and expires July 2025. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the relationship between orofacial myofunctional disorder (OMD) and malocclusion.
- Identify the impact of oral habits on the risk for OMD.
- Explain the role of the dental hygienist in detecting and addressing OMDs.
Orofacial myology focuses on the anatomy, organization, and function of the mouth and facial muscles. An orofacial myofunctional disorder (OMD) is a dysfunctional pattern of the orofacial musculature that interferes with normal growth, development, or proper function of the orofacial tissues.1 OMDs can impact individuals of any age, and may negatively affect psychological and functional well-being. The relationship between malocclusion and OMDs and their treatment has received significant attention over the past decade, however, uniform assessment protocols are still needed.2
OMDs may develop in conjunction with speech and swallowing difficulties, or they may result from a connection between learned behaviors, sleep disorders, physical and structural characteristics, or genetic and environmental influences.1 Disruptive oral habits are one of the main contributors to OMDs, including thumb or finger sucking, cheek/nail/cuticle biting, teeth clenching/grinding, and tongue, lip, or cheek sucking.3 Use of pacifiers, bottles, or sippy cups over prolonged periods may also contribute to OMD development (Table 1).3 Additional causes are related to structural or physiological abnormalities, such as enlarged tonsils, adenoids, deviated septum, short lingual frenum, and a restricted nasal airway. Neurological disorders, developmental delays, and genetics may also play a role in OMD development.3
Malocclusion
Malocclusion is a disturbance of the proper relationship between the maxilla and mandible when they come together in occlusion.4 Facial skeletal abnormalities, which are often associated with malocclusion, influence a variety of orofacial functions, including alterations in the locations of bones, teeth, and muscles. Consequently, chewing processes, speech sound articulation, swallowing, and breathing are altered to accommodate the dentofacial environment.2 Dental and skeletal malocclusion may be inherited or acquired, and are often due to developmental abnormalities.
Edward Angle, MD, DDS, who developed the universally accepted system for describing dental occlusion, believed mouth breathing to be one of the most influential and persistent causes of malocclusion.5 Mouth breathing and poor oral habits are risk factors for malocclusion because they may disrupt the normal balance of growth and function throughout development. Mouth breathing is substantially more connected with occlusal issues, with or without a genetic predisposition. Oral habits, on the other hand, are less relevant in the context of malocclusion unless predisposing contributing factors are present.6
The posterior crossbite is associated with both changed tongue position and speech distortion. The posterior crossbite does not self-correct during tooth development, therefore, early intervention is recommended to allow appropriate growth of the craniofacial structures in order to avoid functional speech impairment and maintain healthy tongue posture.7 A systematic review and meta-analysis conducted revealed that the global prevalence of malocclusion is 56%, with the United States at 53%, suggesting that more than half of the US population have some degree of malocclusion.8
Oral habits are learned behaviors that often begin with a physiological need, such as nasal breathing, stress, or adaptation to anatomical limitations, and then become a default mechanism through repetition.3 Mouth breathing and swallowing are the most common oral habits associated with malocclusion.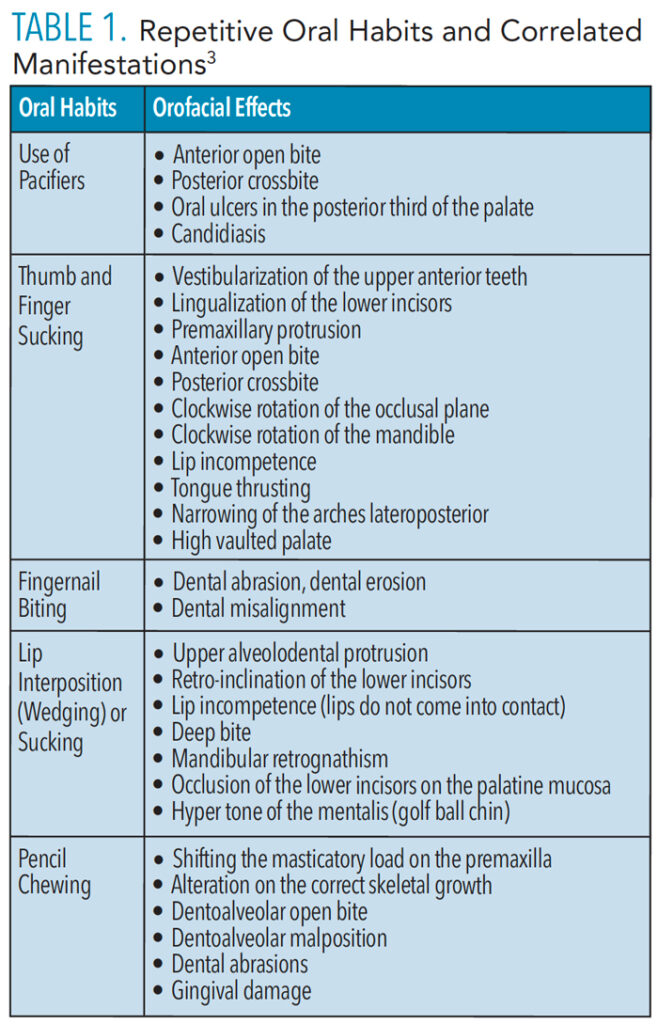
Mouth Breathing
Mouth breathing is a risk factor for malocclusion.6,9 Most commonly occurring during sleep, mouth breathing may be caused by a variety of factors, such as tonsil hypertrophy, septal deviation, nasal polyps, and allergic rhinitis.9 Mouth breathing can cause a broken lip seal, vertical pattern of growth, proclined upper incisors, increased lower facial height, steep mandibular plane angle, and lowering of the chin.10
Optimal craniofacial growth and development are influenced by the ability to breathe comfortably through the nose with the lips gently closed and the tongue positioned upward.11 Lack of muscular pressure on facial bones can negatively impact directional growth over time. Patients with nasal breathing difficulties who subsequently develop a mouth breathing habit typically present with hyperdivergent retrognathic growth patterns that appear as long, narrow, “adenoid” faces, due to its relation to adenoid inflammation.12 This phenotype is characterized by an incompetent upper lip, retro positioned hyoid bone, lingualized mandibular incisors, increased anterior face height, narrow maxillary arch, increased mandibular plane angle, and posteriorly rotated mandible.12
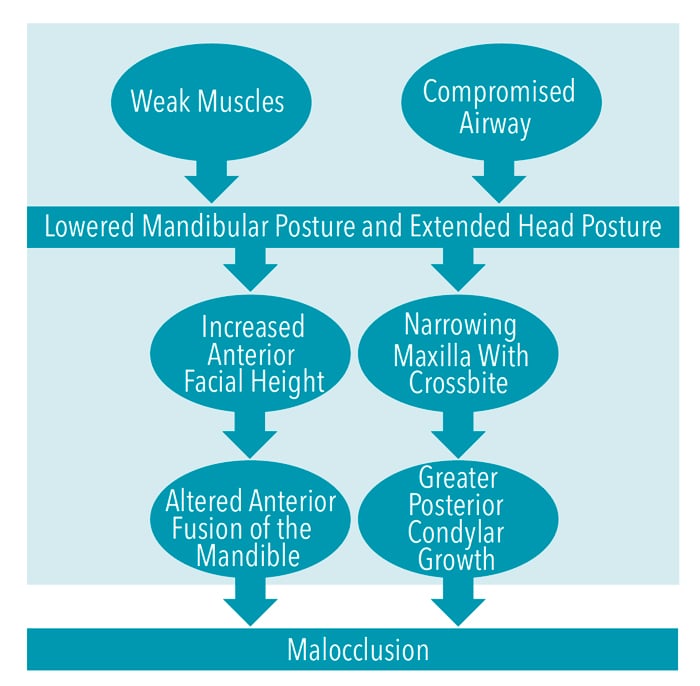
In most cases, patients with high vertical growth patterns do not self-correct over time.14 These patients present with the most challenging cases for orthodontists to treat because of the skeletal complexity, including the overeruption of teeth due to insufficient occlusal contact.13 Although complete correction may not be attainable, patients should be treated for esthetics and functional improvement. The causes of hyperdivergent growth patterns appear to be environmental due to postural adjustments, particularly forward head posture, related to obstructed airways and weak masticatory musculature (Figure 1).14 Hyperdivergent growth may also increase the risk of developing a Class II malocclusion.14,15
Swallowing Patterns
Normal swallowing patterns start with the anterior portion of the tongue placed at the incisive papilla and the dorsum of the tongue completely in contact with the palate.15 The action pressure of the tongue against the palate follows the direction of the median palatine suture toward the oropharynx.16 When normal movement is inhibited, abnormal swallowing develops as a compensatory movement pattern.17 Abnormal swallowing is the interposition of the tongue between or against the teeth. This type of swallowing is typical in infants before tooth eruption; however, during maturation, swallowing changes.3 Normal adult swallowing is characterized by the tip of the tongue being placed in the palate, the dental arches touching, and the absence of labial contraction.3
An abnormal swallowing habit usually produces an open bite and may separate not only the anterior teeth but also most of the posterior teeth. If not corrected, the habit will cause the anterior segments to relapse to their former position after the completion of orthodontic treatment. An open bite alone is not always indicative of the abnormal swallowing habit. Interference habits, such as thumb or finger-sucking, lip or nail-biting, and tongue thrusting, can also adversely affect the dentition.18 A tongue thrust swallow involves excessive perioral effort, as the tongue exerts forward and/or puts lateral pressure into the teeth, rather than vertical pressure into the hard palate with a front to back motion, reinforcing a low resting tongue posture.17,19
Breastfeeding
The action of breastfeeding trains the newborn in many healthy chewing and breathing habits.20 Stimulation of the orofacial muscles is initiated by breastfeeding and continued through mastication.21 The rhythm of sucking to draw milk is a precursor for the rhythm of chewing, as the movement of the masseters, temporalis, and buccinators mimic the act of chewing.20 Breastfeeding also introduces critical connections between the child’s brain and oral habits, as the hypoglossal nerve (cranial nerve XII) powers the tongue to work with deep throat nerves to teach the newborn to swallow, training the airway to be strong and open.21 Furthermore, breastfeeding affects the development of the maxilla and mandible and thus influences dental occlusion.21
Soft Tissue Restriction
Ankyloglossia, or “tongue tie,” is a congenital condition in which a thickened, tightened, or shortened lingual frenulum limits movement of the tongue.22 This condition interferes with feeding, such as mastication, and negatively impacts dental health, sucking, speech, and breathing.23–26 A short lingual frenulum can lead to oral-facial malformations that may decrease the size of the upper airway.23 Lingual frenum restriction can also be a phenotype of obstructive sleep apnea in children,27 as it may increase the possibility of upper airway collapse during sleep.28 Consequently, due to the restrictions that a short lingual frenum places on the muscles and tongue, as well as the impediment placed on bone growth, malocclusion may develop.
Proper surgical release associated with myofunctional therapy can result in increased function and improvement in quality of life. When the tongue rests in its proper position on the palate rather than resting on the floor of the mouth, proper sleep, balance, and posture are supported. Furthermore, when the tongue rests on the palate, the muscles responsible for holding the head up and reducing forward head posture and cervical extension are activated.29
Mastication
Mastication begins in the first year of life and provides the earliest form of input to the oral sensory system. The deep pressure, or proprioception, provided by chewing contributes to the foundation for normal oral movement needed for speech. Chewing aids in the digestion of food, regulates bone growth, reduces psychological stress, increases cognition,30 and stabilizes the temporomandibular joint.31 Non-nutritive chewing of objects can influence the development of malocclusion and craniofacial changes, leading to imbalanced and inefficient chewing.32 Masseter orientation angle and bite force are correlated to different malocclusions, and softer foods require less chewing and less bite force,33 therefore the drastic evolution of the human diet from harder to softer food may also be a contributory factor.
Additionally, one OMD may contribute to the development of another. Chewing, for example, can be affected by mouth breathing, as mouth breathing has been shown to reduce chewing cycles and chewing stroke count.34 Because mastication and respiration are typically accomplished through different routes and mechanisms, masticatory function must be stopped or interrupted during mouth breathing. This is because when nasal breathing is replaced by mouth breathing, the position of the tongue, lips, and mandible are altered to provide an airway through the mouth, which directly affects the chewing process.10,34
Role of the Dental Hygienist
Orofacial dysfunction may be first recognized by the dental hygienist in a clinical setting. While not traditionally within the scope of dental hygiene practice, numerous state dental hygiene boards, such as Nebraska and Iowa, have declared myofunctional therapy part of the practice of dental hygiene.15 More dental hygienists are receiving training and using their knowledge for patient assessment, contributing greatly to early intervention and recognition of myofunctional disorders.
Though effective and reliable guidelines are few, OMD evaluations must include myriad orofacial functions and rely on a variety of disciplines in order to initiate adequate referrals and care for individuals with OMD.2 Dental hygienists must identify the need for referral, as oral myofunctional therapy is an important part of the multidisciplinary approach to treating patients with orthodontic needs, temporomandibular joint disorder, and sleep-disordered breathing.
A chairside clinical assessment will help dental hygienists recognize the presence of OMDs. When performing a chairside clinical evaluation, patients should remain unaware of the assessment so they are present in their most natural state.35 For example, patients with an inclination toward open mouth posture may intentionally keep their mouth closed during assessment if they are aware they are being evaluated. Effective chairside assessment for potential OMDs consists of extraoral observations and intraoral findings. To attain the most accurate observation during extraoral assessment, the patient’s lips should be in a relaxed position and not pursed or straining to gain closure. Clinicians should take note if the tongue is placed between the teeth and listen for unclear “slushy” sounds when patients are speaking.35 During intraoral assessment, malocclusion, ankyloglossia, current or former oral habits, and palate shape should be noted. Clinicians must be aware that although malocclusion may appear to have been corrected through orthodontics, signs from the extraoral assessment may indicate a possible orthodontic relapse.
Conclusion
OMDs and chronic oral dysfunction can lead to dental malocclusion and related craniofacial dysmorphology. Understanding the underlying pathologies that contribute to malocclusion is vital in achieving long-term facial stability. The goal of orofacial myofunctional therapy is to establish optimal functional relationships between the orofacial muscle complex, temporomandibular joint, myofascial connective tissues, and associated neurological systems, resulting in a balanced, stable, and pain-free homeostatic environment.4 Early detection of OMDs and malocclusion by oral health professionals is imperative in supporting this goal, as thorough assessment and proper diagnosis precede effective treatment.
References
- Mason R. A retrospective and prospective view of orofacial myology. International Journal of Orofacial Myology and Myofunctional Therapy. 2005;31(1):5–14.
- Washington S, Ray J. Orofacial myofunctional assessments in adults with malocclusion: a scoping review. International Journal of Orofacial Myology and Myofunctional Therapy. 2021;47(1):22-31.
- Saccomanno S, Paskay L. New ˇrends in Myofunctional Therapy. 2nd ed. Milano, Italy: Edi.Ermes; 2020.
- Benkert K. The effectiveness of orofacial myofunctional therapy in improving dental occlusion. International Journal of Orofacial Myology and Myofunctional Therapy. 1997;23(1):35–46.
- Farrell C, Darcy M. The history of myofunctional orthodontics. Available at: myoresearch.com/storage/app/media/history-of-myofunctional-orthodontics-part-I-0518.pdf. Accessed June 6, 2022.
- Grippaudo C, Paolantonio EG, Antonini G, Saulle R, La Torre G, Deli R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol Ital. 2016;36:386–394.
- Assaf DDC, Knorst JK, Busanello-Stella AR, et al. Association between malocclusion, tongue position and speech distortion in mixed-dentition schoolchildren: an epidemiological study. J Appl Oral Sci. 2021;29:20201005.
- Lombardo G, Vena F, Negri P, et al. Worldwide prevalence of malocclusion in the different stages of dentition: a systematic review and meta-analysis. Eur J Paediatr Dent. 2020;21:115–122.
- da Fontoura C. The interconnection between malocclusion and mouth breathing. Global Journal of Otolaryngology. 2021;24:5.
- Valcheva Z, Arnautska H, Dimova M, Ivanova G, Atanasova I. The role of mouth breathing on dentition development and formation. Journal of IMAB—annual proceeding (scientific papers). Available at: journal-imab-bg.org/issues-2018/issue1/vol24issue1p1878-1882.html. Accessed June 6, 2022.
- Archambault N. Healthy breathing, ’round the clock. Available at: https://leader.pubs.asha.org/doi/葖.1044/leader.FTR1.23022018.48. Accessed June 6, 2022.
- Wysocki J, Krasny M, Skarżyński P. Patency of nasopharynx and a cephalometric image in the children with orthodontic problems. Int J Pediatr Otorhinolaryngol. 2009;73:1803–1809.
- Mew JR. The postural basis of malocclusion: a philosophical overview. Am J Orthod Dentofacial Orthop. 2004;126:729–738.
- Buschang P, Jacob H, Carrillo R. The morphological characteristics, growth, and etiology of the hyperdivergent phenotype. Semin Orthod. 2013;19:212–226.
- Brinkman-Falter P. Myofunctional therapy: enhancing your dental hygiene career. Available at: pubs.royle.com/publication/frame.php?i=654602&p=&pn=&ver=html5&view=articleBrowser&article_id=3631353. Accessed June 4, 2021.
- Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19:691–707.
- Neiva F, Wertzner, H. A protocol for oral myofunctional assessment: for application with children. International Journal of Orofacial Myology and Myofunctional Therapy. 1996;22(1):8–19.
- Garde J, Suryavanshi R, Jawale B, Deshmukh V, Dadhe D, Suryavanshi M. An epidemiological study to know the prevalence of deleterious oral habits among 6 to 12 year old children. J Int Oral Health. 2014;6:39.
- MacAvoy SK, Jack HC, Kieser J, Farella M. Effect of occlusal vertical dimension on swallowing patterns and perioral electromyographic activity. J Oral Rehabil. 2016;43:481–487.
- Elad D, Kozlovsky P, Blum O, et al. Biomechanics of milk extraction during breast-feeding. Proc Natl Acad Sci U S A. 2014;111:5230–5235.
- Pires SC, Giugliani ER, Caramez da Silva F. Influence of the duration of breastfeeding on quality of muscle function during mastication in preschoolers: a cohort study. BMC Public Health. 2012;12:934.
- Hong P, Lago D, Seargeant J, Pellman L, Magit AE, Pransky SM. Defining ankyloglossia: a case series of anterior and posterior tongue ties. Int J Pediatr Otorhinolaryngol. 2010;74:1003–1006.
- Guilleminault C, Huseni S, Lo L. A frequent phenotype for paediatric sleep apnoea: short lingual frenulum. ERJ Open Research. 2016;2:00043–2016.
- Huang Y, Quo S, Berkowski J, Guilleminault C. Short lingual frenulum and obstructive sleep apnea in children. Int J Pediatr Res. 2015;1:003.
- Baxter R, Merkel-Walsh R, Baxter B, Lashley A, Rendell N. Functional improvements of speech, feeding, and sleep after lingual frenectomy tongue-tie release: a prospective cohort study. Clin Pediatr (Phila). 2020;59:885–892.
- Zaghi S, Valcu-Pinkerton S, Jabara M, et al. Lingual frenuloplasty with myofunctional therapy: Exploring safety and efficacy in 348 cases. Laryngoscope Investig Otolaryngol. 2019;4:489–496.
- Bussi MT, Corrêa C de C, Cassettari AJ, et al. Is ankyloglossia associated with obstructive sleep apnea? Braz J Otorhinolaryngol. 2021;S1808-8694:181–186.
- García Pola MJ, González García M, García Martín JM, Gallas M, Seoane Lestón J. A study of pathology associated with short lingual frenum. ASDC J Dent Child. 2002;69:59–62.
- Wildenberg JC, Tyler ME, Danilov YP, Kaczmarek KA, Meyerand ME. Altered connectivity of the balance processing network after tongue stimulation in balance-impaired individuals. Brain Connect. 2013;3:87–97.
- Hirano Y, Onozuka M. [Chewing and cognitive function]. Brain Nerve. 2014;66:25–32.
- Miles TS, Flavel SC, Nordstrom MA. Stretch reflexes in the human masticatory muscles: a brief review and a new functional role. Hum Mov Sci. 2004;23:337–349.
- D’Onofrio L. Oral dysfunction as a cause of malocclusion. Orthod Craniofac Res. 2019;22(Suppl 1):43–48.
- Becht MP, Mah J, Martin C, et al. Evaluation of masseter muscle morphology in different types of malocclusions using cone beam computed tomography. Int Orthod. 2014;12:32–48.
- Hsu HY, Yamachuchi K. Decreased chewing activity during mouth breathing. J Oral Rehabil. 2012;39:559–567.
- Grandi D. The “interdisciplinary orofacial examination protocol for children and adolescents”: a resource for the interdisciplinary assessment of the stomatognatic system. International Journal of Orofacial Myology and Myofunctional Therapy. 2012;38:15䎮.
From Dimensions of Dental Hygiene. July 2022; 20(7)36-39.



