 KTSIMAGE / ISTOCK / THINKSTOCK
KTSIMAGE / ISTOCK / THINKSTOCK
Laser Basics
Although the research is mixed, the use of laser technology in periodontics and implantology continues to grow.
This course was published in the April 2016 issue and expires April 20, 2019. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss how lasers work and how they are used in periodontics and implantology.
- Identify the characteristics of C02, argon, Nd:YAG, erbium, and diode lasers.
- Explain the safety protocols required during laser use.
Laser—an acronym for light amplification by stimulated emission of radiation—is a medical device capable of delivering energy to a target. When the laser energy reaches human tissue, it selectively vaporizes components of human tissue based on its wavelength, power, and exposure time.
Essentially, a laser consists of a box with a medium inside, which can be a gas, solid, or semiconductor. It is the medium that determines the type of laser. The lasers most commonly used in dentistry are:
- Carbon dioxide (CO2) and argon: gas medium
- Neodymium-doped yttrium aluminium garnet (Nd:YAG) and erbium (Er): solid medium
- Diodes: semiconductor medium
The most important determinant of a laser’s potential effects on living tissue is the wavelength of the laser beam (Figure 1). Wavelengths are measured in nanometers (nm) or microns. Nm is the most commonly used wavelength measurement but microns are often implemented to calibrate wavelength measurements in the scientific literature. A thousand nm equal 1 micron. For example, 1,064 nm = 1.064 microns.

COLUZZI D. FUNDAMENTALS OF LASERS IN DENTISTRY: BASIC SCIENCE, TISSUE INTERACTION, AND INSTRUMENTATION. J LASER DENT. 2008
Generally, laser wavelengths cannot be changed—they are fixed. The most common range of wavelengths used in periodontics and implantology spans from 400 nm to 10,600 nm. This range includes both the invisible and visible portions (which produce the perception of light) of the electromagnetic spectrum. Interestingly, animals can see wavelengths that humans cannot, which are typically in the ultraviolet portion (300 nm to 500 nm) of the electromagnetic spectrum.
More than 95% of the lasers used in dentistry, including those used to treat periodontitis and peri-implantitis, produce invisible energy. The range of the electromagnetic spectrum includes the visible wavelengths (390 nm to 700 nm); the invisible range, also known as infrared and far-infrared portions of the electromagnetic spectrum (700 nm+); and wavelengths below 450 nm. Ionizing radiation (X-rays, gamma rays) is also part of the invisible range. It is generally harmful to human tissue depending on exposure durations. Dental lasers do not produce this type of radiation.
Laser light can exhibit the following effects:
- Absorption
- Transmission
- Reflection
- Scatter
When a laser is directed at and absorbed by living tissue, the target tissue is directly impacted (Figure 2). However, the laser’s light energy can also be reflected, scattered, or move through the tissue without any effect. Different laser wavelengths have varying abilities to affect living tissue. Therapeutic lasers are designed to target certain substances or tissues, known as chromophores. These include water, blood, pigmentation, epithelium, collagen, inflamed areas, bone, minerals, enamel, dentin, cementum, and bacteria.

GLOBAL PERIODONTAL LASER SOCIETY
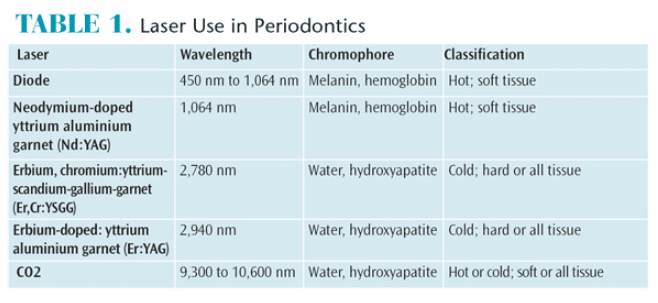
The most common surgical dental lasers and their absorption spectra are:
- CO2: water and hydroxyapatite
- Erbium: water and hydroxyapatite
- Nd:YAG: pigmentation, hemoglobin, and melanin
- Diode: pigmentation, hemoglobin, and melanin (Table 1)
These lasers have the potential to treat periodontitis and ailing implants because the absorption spectra is targeting the tissues that need to be restored to health.
Lasers are sometimes referred to as soft or hard tissue lasers. This is determined by what tissue is affected and by the wavelength of the laser used. When a laser is activated and the energy is absorbed into the target tissue, the effects comprise: thermal or heat (photothermal); acoustic or vibratory (photo-acoustic); or chemical (photochemical) interactions. Chemical interactions occur at the cellular level and can kill or alter bacteria, cause mitochondrial stimulation or biostimulation, enable vasodilation or sealing of vessels, encourage cell proliferation, and stimulate growth factors and progenitor cells.
The effects of laser energy are wide ranging. Lasers show promise in wound healing, tissue ablation, bacterial reduction, epithelial ablation, connective tissue remodeling, enhanced bone metabolism, hemorrhage control, and enhanced root preparation. They may also facilitate regeneration around teeth and titanium implants.
When activated, lasers can work on a continuous basis or on a pulsed setting. Most highly sophisticated laser surgical systems operate with very precise pulsing that enables the target tissues to cool in between intense pulses (microseconds or millionths of a second). This is the type of precision, controlled power, and pin-point accuracy that lasers have the potential to perform. However, not all lasers operate in the same fashion. Some are used continuously at low power, while others are pulsed with high-intensity power.
When choosing the appropriate laser for use in periodontics and implantology, the wavelength, target tissue, type of power, pulsing mode, cooling mechanism, delivery system, quality, and, most important, the training required to safely operate the device are all factors to consider.
CO2 LASERS
The wavelengths for a CO2 laser range from 9,300 nm to 10,600 nm. The medium for the CO2 lasers is a gas that is cooled with either water or air. CO2 laser light is well absorbed by water molecules and hydroxyapatite and the energy is delivered through a hollow tube-like waveguide. CO2 lasers can operate in a continuous or pulsed mode. The older CO2 systems were mostly continuous or gated (a modified way of pulsing with little energy and half the power).
Much of the initial research on CO2 lasers evaluated use in a continuous mode. Contemporary research is evaluating the abilities of a super-pulsed CO2 laser to treat periodontitis and peri-implantitis.3–18 Due to their high absorption in water, super-pulsed CO2 lasers penetrate the soft tissues only shallowly. This makes them excellent cutting lasers that create little collateral damage. Periodontal and implant procedures conducted with a super-pulsed CO2 laser have demonstrated bacterial kill of pathogens in the diseased periodontal pocket with no damage to the bone or tooth surfaces, including enamel, dentin, and cementum.3,4 Case reports indicate that CO2 laser therapy provides significant periodontal benefits.3 Due to the high reflectivity of the 10,600 nm wavelength, the super-pulsed laser is also safe and effective for detoxifying titanium on the surfaces of ailing implants with bone loss. Scanning electron microscopy has shown no deleterious effects on titanium in vitro and in vivo at the newly established settings of the 10,600 nm super-pulsed CO2 laser.3 In addition, little temperature change occurred during in vitro experimentation on the implant surfaces.4
Human clinical trials are currently studying the effects of a new treatment protocol that uses a 10,600 nm super-pulsed CO2 laser for the treatment of periodontitis and peri-implantitis.3 Other potential uses for the CO2 laser include precise cutting of tissue, biopsy sampling, removal of pathology, and elimination of excess hyperplastic and inflamed soft tissue. The CO2 laser can also perform soft tissue procedures such as gingivectomy, frenectomy, epulis removal, and correction of tongue ties.
The CO2 laser provides a clear operating field, which enables it to seal blood vessels and coagulate soft tissue. Patients who undergo CO2 laser treatment appear to experience less post-operative pain than more invasive methods. Research using a visual analog scale to evaluate pain in a controlled trial is needed to evaluate this clinical observation.5
ARGON LASERS
Argon lasers use a gas medium and produce wavelengths between 488 nm and 514 nm. This beam is in the visible light spectrum (blue and blue green). This wavelength is poorly absorbed in enamel and dentin. Argon lasers were traditionally used for caries detection. When they illuminate the tooth, the caries lesion appears dark orange/reddish in color and is easy discernable from the surrounding enamel and dentin. However, these lasers are no longer in common use because of technological advances in the field of caries detection. Additionally, some early studies showed argon lasers may have adversely affected wound healing.
Nd:YAG LASERS
Nd:YAG lasers have a solid crystal medium with a wavelength of 1,064 nm. It is well absorbed by hemoglobin, blood, pigmentation, and melanin. The 1,064 nm wavelength is poorly absorbed in water; therefore, this wavelength can penetrate deeply into some tissues. Nd:YAG lasers have a pulsing mode with high powers delivering a blast of energy in extremely short bursts (millionths of a second). The energy is delivered through a very thin quartz fiber, which needs to be cut to deliver the proper energy to the target tissue.
In 2004, the laser-assisted new attachment procedure (LANAP) received clearance by the United States Food and Drug Administration (FDA) for the treatment of periodontitis as a stand-alone surgical procedure using the Nd:YAG 1,064 nm wavelength. The use of this patented protocol is said to require a specific FDA-cleared laser for which the operator must complete additional training. The LANAP protocol also includes a laser assisted peri-implantitis protocol for the treatment of ailing implants. Both of these protocols are flapless and conducted under local anesthesia.
Some human histological studies have produced evidence that suggests the LANAP protocol may spur at least some periodontal regeneration around teeth.17,18 However, no histological studies to date show that the LANAP results in regeneration around dental implants.
The use of an Nd:YAG 1,064 nm laser may support biostimulation due to the depth of penetration into living tissues. Proper training, however, is essential to the safe performance of this procedure. Due to the deep penetration of this wavelength, caution is indicated because of the potential for lateral thermal necrosis (thermal damage to tissues). Implant surfaces can heat up quickly and melt if the proper laser technique is not followed.7
ERBIUM LASERS
Erbium lasers are available in two wavelengths: 2,780 nm (erbium, chromium:yttrium-scandium-gallium-garnet or Er,Cr:YSGG) and 2,940 nm (Erbium-doped: yttrium aluminiumgarnet or Er:YAG). Both have solid crystal mediums. These lasers are primarily absorbed in water and hydroxyapatite, and they can work both as both soft tissue and hard tissue lasers. The penetration is shallow due to the high absorption in water. Energy is delivered in a pulsed mode via a flexible fiber, usually with a handpiece.
Because the erbium 2,940 nm laser has been in existence much longer than the 2,780 nm version, most of the research has used the 2,940 nm wavelength.19–30 The research has shown that these wavelengths are effective in both flap and flapless surgical protocols for the treatment of periodontitis and peri-implantitis. Erbium lasers can be safely used on root surfaces and implants if strict protocols are followed.7 They can remove calculus and granulation tissue and detoxify titanium. The penetration is shallow and the absorption in water reduces any thermal damage or heating. There is a slight difference in absorption in water between the two erbium wavelengths. The 2,940 nm erbium laser is absorbed three times better in water than the 2,780 nm version.19,20
DIODE LASERS
Diode lasers are in the 450 nm to 1,064 nm wavelength range. The mediums are semiconductor crystals. These lasers target pigmentation, melanin, and use low power, which can be pulsed or gated. Diode laserss can be used to cut tissue, kill bacteria at shallow depths, bistipulate tissues, and provide low-level laser therapy. Diode lasers can also generate high temperatures and should be used with caution around living tissues such as the gingiva, bone, enamel, dentin, cementum, and mucosa, as well as titanium. With diode lasers, the longer the wavelength, the greater absorption in hemoglobin and water, which accompanies a decrease in melanin absorption. As absorption by water increases, the depth of penetration in the surrounding tissues decreases. The high-diode wavelength lasers tend to generate less thermal heat on titanium surfaces. However, extreme caution should be exercised when using diodes around tissue and titanium. The potential risk of necrosis and increased bone temperature exists if the practitioner does not understand the variation of tissue effects caused by diode lasers of different wavelengths and energies.
SAFETY
Safety is always the number one priority when working with surgical lasers. All dental surgical lasers have the potential to cause severe harm to the eyes and skin. Patients and clinicians must wear protective eyeglasses (dependent on the type of laser in use).
Surgical lasers produce plumes of vaporized tissue when activated. Thus, high-speed vacuum evacuation and universal precautions—such as the wearing of masks and gloves—must be observed when using surgical lasers. The Occupational Safety and Health Administration requires the display of appropriate signage in each room in which a laser is utilized.
SUMMARY
The CO2, erbium, Nd:YAG, and some of the diode lasers have demonstrated promising clinical outcomes for the treatment of periodontitis and peri-implantitis. There are a number of different wavelengths that can be utilized alone or in combination to achieve clinical goals (Table 2). In 2010, the American Academy of Periodontology (AAP) created a position paper (published in 2011) noting there was insufficient evidence to show that laser therapy was better than traditional treatment techniques for the treatment of chronic periodontitis.31 However, the AAP is working on a new position paper that will incorporate the research conducted over the past 6 years. More study is warranted to further demonstrate the effectiveness and safety of laser therapy.
References
- Natto ZS, Aladmawy M, Levi PA Jr, Wang HL. Comparison of the efficacy of different types of lasers for the treatment of peri-implantitis: a systematic review. Int J Oral Maxillofac Implants. 2015;30:338–345.
- Kotsakis GA, Konstantinidis I, Karoussis IK, Ma X, Chu H. Systematic review and meta-analysis of the effect of various laser wavelengths in the treatment of peri-implantitis. J Periodontol. 2014;85:1203–1213.
- Linden E, Vitruk P. SuperPulse 10.6um CO2 laser-assisted, closed flap treatment of peri-implantitis. Implant Practice. 2015:8:30–34.
- Cobb C, Vitruk P. Effectiveness of a super pulsed CO2 laser for removal of biofilm from three different types of implant surfaces: an in vitro study. Implant Practice US. 2015;8:14–20.
- Linden E, Abrams H, Matheny J, Kaplan A, Kopczyk R, Jasper S. A comparison of postoperative pain experience following periodontal surgery using two local anesthetic agents. J Periodontol. 1986;57:637–642.
- Javed F, Hussain HA, Romanos GE. Re-stability of dental implants following treatment of peri-implantitis. Interv Med Appl Sci. 2013;5:116–121.
- Aoki A, Sasaki KM, Watanabe H, Ishikawa I. Lasers in nonsurgical periodontal therapy. J Periodontol. 2004:36:59–97.
- Aoki A, Mizutani K, Schwarz F, et al. Periodontal and peri-implant would healing following laser therapy. Periodontol 2000. 2000;68:217–269.
- Barone A, Covani U, Crespi R, Romanos GE. Root surface morphological changes after focused versus defocused CO2 laser irradiation: a scanning electron microscopy analysis. J Periodontol. 2002;7:370–373.
- Convissar RA, Goldstein EE. An overview of lasers in dentistry. Gen Dent. 2003;51:436–440.
- Crespi R, Covani U, Margarone JE, et al. Periodontal tissue regeneration in beagle dogs after laser therapy. Laser Surgy Med. 1997;21:395–402.
- Deppy H, Grime H, Brill T, Waynesfield S. Titanium deposition after peri-implant care with the carbon dioxide laser. Into J Oral Maxillofacial Implants. 2002;17:707–714.
- Essen E, Hayton MC, Oz IAN, Eroding O, Kaslik ED. Gingival melanin pigmentation and its treatment with the CO2 laser. Oral Surgy Oral Med Oral Patrol Oral Radios Endor. 2004;98:522–527.
- Javed F, Hussain HA, Romanos GE. Re-stability of dental implants following treatment of peri-implantitis. Interv Med Appl Sci. 2013;5:116–121.
- Luthanen M, Merriam JI, Letha VP. Extracellular matrix in healing C02 laser incision wound. J Oral Pathol. 1978;16:322–331.
- McCormack SM, Fried D, Featherstone JD, Glena RE, Seka W. Scanning electron microscope observations of CO2 laser effects on dental enamel. J Dent Res. 1995;74:1702–1708.
- Yukna RA1, Carr RL, Evans GH. Histological evaluation of an Nd:YAG laser-assisted new attachment procedure in humans. Int J Periodontics Restorative Dent. 2007;27:577–587.
- Kim DM, De Angelis N, Camelo M, Nevins ML, Schupbach P, Nevins M. Human clinical and histological evaluation of laser-assisted new attachment procedure. Int J Periodontics Restorative Dent. 2012;32:497–507.
- Al-Falaki R, Cronshaw M, Hughes FJ. Treatment outcome following use of the erbium, chromium:yttrium, scandium, gallium, garnet laser in the non-surgical management of peri-implantitis: a case series. Br Dent J. 2014;217:453–457.
- Al-Falaki R, Wadia R, Hughes FJ. Use of erbium, chromium:yttrium scandium gallium garnet laser as an adjunct to root surface instrumentation: analysis of an extended case series. J Clin Periodontol. January 2015. Epub before print.
- Aoki A, Sasaki K, Watanabe H. Lasers in non-surgical periodontal therapy. Periodontol 2000. 2004;36:59–97.
- Aoki A, Mizutani K, Schwarz F, et al. Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000. 201568:217–269.
- Cobb CM, Low S, Coluzzi DJ. Lasers and the treatment of chronic periodontitis. Dent Clin N Am. 2010;54:35–53.
- Dyer B, Sung EC. Minimally invasive periodontal treatment using the er, cr:ysgg laser. A 2-year retrospective preliminary clinical study. Open Dent J. 2012;6:74–78.
- Schwarz F, Aoki A, Becker J, Sculean A. Laser application in non-surgical periodontal therapy: a systematic review. J Clin Periodontol. 2008;35(Suppl 8):29–44.
- Schwarz F, Becker J. Treatment of periodontitis and peri-implantitis with an Er:YAG laser:experimental and clinical studies. Medical Laser Application. 2005;47–59.
- Schwarz F, Sculean A, Berakdar M, Georg T, Reich E, Becker J. Periodontal treatment with an Er:YAG laser or scaling and root planing. A 2-year follow-up split-mouth study. J Periodontol. 2003;74:590–596.
- Schwarz F, Sculean A, Georg T. Periodontal treatment with an Er:YAG laser compared to scaling and root planing. A controlled clinical study. J Periodontol. 2001;72:361–367.
- Sculean A, Schwarz F, Berakdar M, Romanos GE, Arweiler NB, Becker J. Periodontal treatment with an Er:YAG laser compared to ultrasonic instrumentation: A pilot study. J Periodontol. 2004;75:966–973.
- Ishikawa I, Aoki A, Takasaki A. Potential applications of erbium:YAG laser in periodontics. J Periodontal Res. 2004:39:275–285.
- American Academy of Periodontology statement on the efficacy of lasers in the non-surgical treatment of inflammatory periodontal disease. J Periodontol. 2011;82:513–514.
From Dimensions of Dental Hygiene. April 2016;14(04):56–59.