
Innovations in Implant Therapy
Novel minimally invasive dental implant restorative techniques offer increased patient treatment acceptance and shortened recovery time.
This course was published in the March 2023 issue and expires March 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 690
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the history of implant therapy.
- Explain flapless surgical implant placement.
- Identify technological advancements for precise implant placement.
Tooth loss affects more than half of the adult population in the United States.1 Implant-supported restorations have become the top choice for restorative tooth replacement due to the benefits of conserving the surrounding alveolar bone and tooth structures.1,2
Data from the National Health and Nutrition Examination Survey show the prevalence of dental implants rose from 5.7% to 17% between 1999 and 2016 with projected growth as high as 23% by 2026.1
As implants have become the gold standard for replacing missing teeth, innovative and less invasive approaches have emerged, warranting a greater understanding of the current techniques available.
History of Dental Implants
Human attempts to fashion dental implants date back many centuries. Evidence of custom-designed, soldered gold bands intended to restore oral function was discovered among 500 BC-period Etruscans and attempts at stabilizing periodontally involved teeth with gold ligature wires have been noted as far back as ancient Egyptian times.3
The titanium-coated implants used today are the product of Per-Ingvar Brånemark, MD, PhD, who developed the pure titanium screw method in 1965.3 Brånemark’s work led to the idea of osseointegration and the inclusion of dental implants into dental curricula.
The conventional placement of implants requires surgically flapping the tissue to expose the bone and inserting the implant using a free-handed method.4 However, emerging technologies provide enhanced location accuracy through medical imaging technology such as cone-beam computed tomography (CBCT) and surgically guided placement procedures.4
Flapless Surgical Implant Placement
The term “flapless implant surgery” involves preparing the implant osteotomy and placing the implant without the elevation of a mucoperiosteal flap.2,4 Ledermann pioneered the flapless surgical technique in the late 1970s in an attempt to minimize the bone resorption process associated with implant osseointegration.5
Osseointegration is when living bone is in direct contact with the implant surface, establishing a nonmovable integration between the implant and bone.6,7 The degree of osseointegration is a key determinant of implant success. Additionally, the adaptation of the epithelium to the abutment or implant plays a significant role in its longevity.8
Should the biologic seal be broken, a cascade of tissue and cell injury will result within the internal milieu that supports the implant device, triggering an inflammatory response in the surrounding soft tissues. The underlying hard tissue will then undergo osteoclastic activity, followed by chronic resorption of the supporting bone. As the supporting bone continues to deteriorate, granulation tissue will develop, causing implant failure.8
Primary variables related to different types of surgical procedures, as well as secondary factors associated with the development of marginal bone loss, may impact the long-term clinical performance of dental implant therapy.6 The traditional technique for implant surgery entails flap elevation, which gives direct access to implant sites, improves placement angulation control, and minimizes the risk of bone fenestrations and dehiscence.4
Some studies, however, found that this method resulted in higher or receded soft tissue and bone resorption, post-operative edema, discomfort, and delayed recovery due to increased surgical stress and longer surgical time.9 Maintaining the papillae and gingival contour intact around the implant is critical, particularly with patients whose soft tissue is visible while performing functions such as speaking and smiling.5 By eliminating the need for an incision, there is less chance of interrupting blood flow from the bone membranes or soft tissues, which could otherwise lead to inadequate blood circulation and the necessary nutrients to the recipient site, resulting in poor bone regeneration or osseointegration surrounding the implants.10
The bone receives its blood supply through three distinct pathways: the periodontal ligaments, connective tissue above the periosteum, and the alveolar bone. When a tooth is lost or extracted, the periodontal ligament loses its blood supply, leaving only the soft tissues and bone to supply the necessary blood in the area.5
Compared to bone marrow, cortical bone has few blood vessels flowing through it. When soft tissue is flapped, the available blood from the soft tissue to the bone (supraperiosteal blood supply) is taken, leaving behind an inadequately vascularized cortical bone, which contributes to bone resorption during the initial phase of healing.5
Although few studies have evaluated the crestal bone height between flapless and flap surgical procedures, one study compared the clinical manifestations of marginal bone loss and swelling, patients’ reported pain assessment, and number of analgesics taken between flapless and conventional flap implant insertion. Researchers found that the flapless implant placement resulted in more positive outcomes concerning marginal bone loss, patient pain perception, and number of post-operative analgesics taken. No significant difference was noted in post-operative swelling between the two implant techniques.5
Technological Advancements
Innovative digital technological advancements, such as guided computer-assisted surgery, have improved implant placement by substantially increasing the precision with which implants are positioned for optimal biological and prosthetic locations.2,11 Effective access to the alveolar bone is a crucial step in the implant-placement process.
Conventional approaches to dental implant insertion require crestal incision and mucoperiosteal flap reflection to ensure visual recognition of underlying anatomical landmarks, such as foramina, lingual undercuts, and maxillary sinuses; prevent injury to the patient; and support proper placement of the implant for long-term success.4
Despite its potential benefits, flapless surgery is often regarded as unperceptive due to difficulties in assessing the shape and health of underlying alveolar bone and anatomical regions.9 However, with the use of CBCT and dental implant planning software, the residual bone and essential anatomical features in surgery sites may be precisely analyzed via three-dimensional radiography.
The use of CBCT-guided surgery permits advanced detection of vestibular concavities and lingual-palatal bone plates around the desired recipient site, thereby optimizing bur angulation and decreasing the likelihood of bone perforations and fenestrations.12,13
CBCT scans assist with planning and visualizing the placement by creating a surgical drilling guide.12 The use of traditional dental Xrays for implant insertion is no longer an accepted practice due to the considerable risk involved and limited diagnostic ability of anatomical accuracy.14
Although some oral specialists still rely on two-dimensional panoramic imaging for routine cases, the American Academy of Oral and Maxillofacial Radiology recommends the use of cross-sectional imaging for all dental implant surgeries as the evidence demonstrates that CBCT offers significant advantages that can alter treatment planning and improve surgical outcomes (Table 1).15
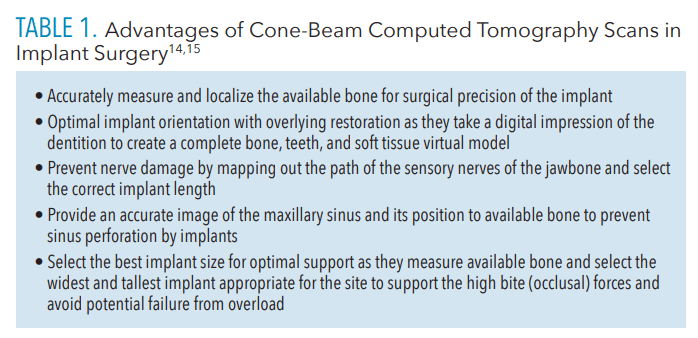 Additional patient considerations regarding CBCT scans are the inexpensive cost, relatively low radiation, and convenience of use. The 3D image produced by a CBCT scan can also be used by oral health care professionals as an effective visual tool while educating patients chairside about recommended restorative treatment.14
Additional patient considerations regarding CBCT scans are the inexpensive cost, relatively low radiation, and convenience of use. The 3D image produced by a CBCT scan can also be used by oral health care professionals as an effective visual tool while educating patients chairside about recommended restorative treatment.14
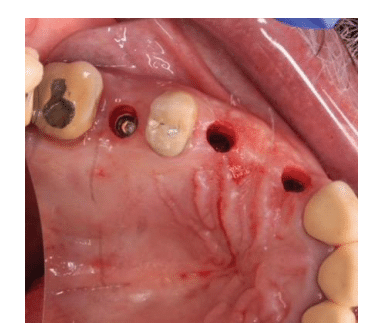
Data from CT scans is used in virtual implant planning systems to evaluate bone volume, while 3D computer models are used to create the implant-retained prosthesis and surgical guidance. Guides may be fabricated using a model base or through a rapid prototyping technique. Surgical templates using model-based guides are fabricated manually or using computerized technology by milling or laser printing, and can be used with a traditional flap or flapless implant procedures (Figure 1).15,16
The guide is built to provide stability as the implant is drilled into the bone and eliminates the margin of error by restricting the permitted range of route trajectory and depth for exact placement.2,12 Several variables must be considered with any implant insertion technique, including the clinician’s expertise, condition of the patient’s hard and soft tissues, patient’s overall health, and nature of the surgical treatment itself, as they can affect the long-term clinical performance.10
implant placement.
As implant insertion accuracy-enhancing technologies gain significance in restorative dentistry, oral health professionals must become knowledgeable about implant placement procedures. Free-handed implant placement involves osteotomy preparation and implant insertion, which are both done by hand, with no surgical guides to affect the path of implantation into the recipient site.18
Cast-based partially guided implant placement uses a prosthetically driven nonrestrictive surgical guide while bone bed preparation and implant insertion are done freehand.18 These guidelines are made from dental casts and don’t consider the underlying bone shape.
When the drill partially guided implant placement method is used, although the implant insertion is done by free hand, the bone bed preparation is directed by a restricted prosthetically driven surgical guide designed with the underlying bone shape in mind.18
The static computer-aided implant placement uses a completely guided method that includes both restricted osteotomy preparation and implant placement using a prosthetically driven surgical guide that was created with preoperative computed tomographic and stereolithographic data.18,19
Finally, the dynamic computer-aided implant placement is a completely guided method for both osteotomy preparation and implant insertion using a surgical navigation system that immediately reproduces the virtual implant location using computerized tomographic data and allows for intra-operative alterations.18,19
Patient Considerations for Flapless Implant Placement
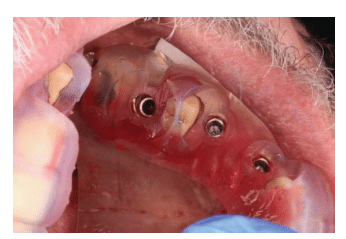
Patients who present with sufficient keratinized attached gingiva, an approximate bone width of 7 mm in the implant recipient site, and do not require bone augmentation are considered viable candidates for flapless, computer-assisted guided implant placement.11 The procedure allows insertion of implants into the bone through the mucosal tissue without invasive incision of the tissue or flap reflection that can sometimes lead to gingival scarring, vascular disruption, and impairment of the gingival papilla.2,10
By using a rotating instrument or a soft tissue punch device, dental specialists can pierce the gingival tissue to gain access to the underlying bone while preserving the vascular supply and existing soft tissue shape (Figure 2).5
using a soft tissue punch device.
A study examining the success rate of dental implants among patients with well-controlled diabetes using either the conventional method or the flapless technique revealed a comparatively similar outcome: 94.2% and 92.3%, respectively.20 Diabetes was once thought to be a contraindication for implant restoration therapy due to concerns over poor wound healing.18,20 However, guidelines from the European Federation of Periodontology and International Diabetes Federation suggest that well-controlled glucose levels do not increase the risk of developing peri-implantitis. Conversely, poorly controlled diabetes increases the risk of peri-implantitis.18
Conclusions
Oral health professionals are essential in guiding patients in making educated, evidence-based decisions regarding their oral healthcare needs. With the advent and widespread adoption of cutting-edge dental technologies, patients benefit due to the increased precision and accuracy in diagnostic and restorative therapy.
References
- Elani HW, Starr JR, Da Silva JD, Gallucci GO. Trends in dental implant use in the US, 1999-2016, and projections to 2026J J Dent Res. 2018;97:1424–1430.
- Naeini EN, Atashkadeh M, De Bruyn H, D’Haese J. Narrative review regarding the applicability, accuracy, and clinical outcome of flapless implant surgery with or without computer guidance. Clin Implant Dent Relat Res. 2020;22:454–467.
- Abraham CM. A brief historical perspective on dental implants, their surface coatings and treatments. Open Dent J. 2014;8:50–55.
- Yadav MK, Verma UP, Parikh H, Dixit M. Minimally invasive transgingival implant therapy: a literature review. Natl J Maxillofac Surg. 2018;9:117–122.
- Divakar TK, Gidean Arularasan S, Baskaran M, et al. Clinical evaluation of placement of implant by flapless technique over conventional flap technique. J Maxillofac Oral Surg. 2020;19:74–84.
- Buser D, Sennerby L, De Bruyn H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol 2000. 2017;73:7–21.
- Gehrig JS, Shin DE, Willmann DE. Foundations of Periodontics for the Dental Hygienist. 5th ed. Burlington, Massachusetts: Jones & Bartlett Learning; 2019:165.
- Jayesh RS, Dhinakarsamy V. Osseointegration. J Pharm Bioallied Sci. 2015;7(Suppl 1):S226–S229.
- Cai H, Liang X, Sun DY, Chen JY. Long-term clinical performance of flapless implant surgery compared to the conventional approach with flap elevation: a systematic review and meta-analysis. World J Clin Cases. 2020;8:1087–1103.
- Gao X, Qin S, Cai H, et al. Comparison of general and aesthetic effects between flapless and flap techniques in dental implantation: a meta-analysis of randomized controlled trials. Int J Implant Dent. 2021;7:100.
- Romandini M, Ruales-Carrera E, Sadilina S, Hämmerle CHF, Sanz M. Minimal invasiveness at dental implant placement: A systematic review with meta-analyses on flapless fully guided surgery. Periodontol 2000. 2022;10:1111.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Flapless versus conventional flapped dental implant surgery: a meta-analysis. PLoS One. 2014;9:e100624.
- Nkenke E, Vairaktaris E, Bauersachs A, et al. Acceptance of virtual dental implant planning software in an undergraduate curriculum: a pilot study. BMC Med Educ. 2012;12:90.
- Gupta J, Ali SP. Cone-beam computed tomography in oral implants. Natl J Maxillofac Surg. 2013;4:2-6.
- Weiss R 2nd, Read-Fuller A. Cone-beam computed tomography in oral and maxillofacial surgery: an evidence-based review. Dent J (Basel). 2019;7:52.
- Kernen F, Kramer J, Wanner L, et al. A review of virtual planning software for guided implant surgery – data import and visualization, drill guide design and manufacturing. BMC Oral Health. 2020;20:251.
- Mandelaris GA, Rosenfeld AL, King SD, Nevins ML. Computer-guided implant dentistry for precise implant placement: combining specialized stereolithographically generated drilling guides and surgical implant instrumentation. Int J Periodontics Restorative Dent. 2010;30:275–281.
- Nibali L, Gkranias N, Mainas G, Di Pino A. Periodontitis and implant complications in diabetes. Periodontol 2000. 2022;90:88–105.
- Kalaivani G, Balaji VR, Manikandan D, Rohini G. Expectation and reality of guided implant surgery protocol using computer-assisted static and dynamic navigation system at present scenario: evidence-based literature review. J Indian Soc Periodontol. 2020;24:398–408.
- Singh K, Rao J, Afsheen T, Tiwari B. Survival rate of dental implant placement by conventional or flapless surgery in controlled type 2 diabetes mellitus patients: a systematic review. Indian J Dent Res. 2019;30:600–611.
From Dimensions of Dental Hygiene. March 2023; 21(3)34-37.



