
Improve Oral Health With Probiotic Therapy
This natural approach can help patients achieve oral homeostasis and maintain a balanced salivary pH.
This course was published in the March 2023 issue and expires March 2026. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
AGD Subject Code: 010
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the origins of probiotics.
- Identify the role probiotics play in oral health.
- Explain how dental hygienist can use this therapy to help patients improve oral health.
As more people have become interested in improving their health, the demand for natural therapies, healthy dietary choices, and modern solutions to prevent overall health problems has grown.1 Probiotics—the “good” bacteria in the form of live cultures found in foods and supplements—are used as alternatives and adjuncts to traditional therapies. In some cases, they have become more popular than antibiotics, as they have the potential to restore homeostasis.1
Probiotics offer many health benefits. They are often associated with balancing bacteria in the gastrointestinal tract, beginning with the oral cavity. The oral cavity is the second most colonized microbial habitat in the human body and is home to more than 700 bacterial species.2,3 From an oral health perspective, probiotic therapy can assist in achieving oral homeostasis to counter harmful bacteria caused by poor nutrition, smoking, limited access to oral healthcare, systemic diseases, and medication usage.4
Research suggests that balancing salivary pH with probiotic therapy may reduce the risk of chronic oral diseases such as dental caries, gingivitis, periodontal diseases, oral malodor, tooth loss, and oral cancer.4 Dental hygienists play a key role in educating patients on how adjunctive probiotic therapy can prevent oral diseases.
Probiotics Defined
The word “probiotic” comes from Latin and Greek roots, as “pro” means “for” in Latin and “bios” means “life” in Greek.5 Dating back to the 1800s, fermented food products containing Lactobacillus were thought to prolong life, yet scientific study on potential health benefits did not begin until 1905. At the time, probiotics were found to be most impactful to gastrointestinal health, as probiotics exist mainly in the human intestines.6,7
The composition of intestinal microorganisms significantly impacts the immune response.7 It was not until the 1980s, that probiotic strains were found to help prevent disease-causing bacteria.6 Today, the term “probiotics” is used to describe microorganisms that help manage a poorly balanced bacterial community.4 Probiotics assist in not only the mitigation of intestinal disorders, but also in the prevention of disease.8
Probiotics and the Oral Cavity
The oral microbiome is a naturally diverse living space of microorganisms that is in constant battle to maintain balance while considering the host’s immune response.9 Oral homeostasis is maintained by the pro- and anti-inflammatory functions of resident organisms; it is complex, as it is responsible for the maintenance of a healthy oral microbiome (symbiosis) and is associated with an imbalanced oral microbiome (dysbiosis).9
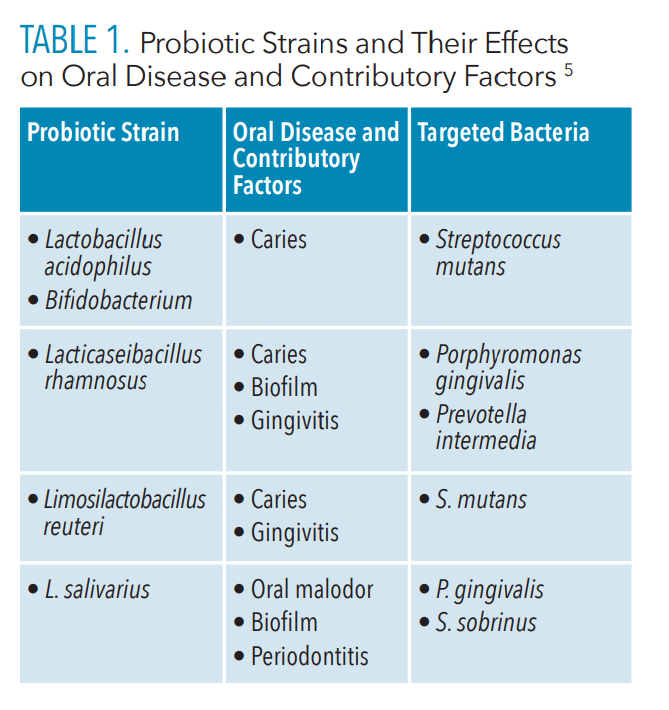
When dysbiosis occurs and the oral microbiome becomes disrupted, it can contribute to the decline of both oral and overall health.9 The counteraction for dysbiosis is to shift toward a healthy balance through the addition of probiotics. Several different strains of probiotics can be used to target oral diseases and their causative pathogens (Table 1).5
 Lactobacillus and Bifidobacterium are health-promoting probiotic strains that target harmful oral bacteria. Both are present in breast milk and are typically the first microorganisms to populate the oral cavity.10
Lactobacillus and Bifidobacterium are health-promoting probiotic strains that target harmful oral bacteria. Both are present in breast milk and are typically the first microorganisms to populate the oral cavity.10
A wide variety of Lactobacilli strains are beneficial to the periodontium. They produce hydrogen peroxide and lactic acid, which work together to intercept the colonization of harmful oral pathogens.11 To further maintain oral homeostasis, counter the constant battle between bacterial dominance, and reduce the risks of contributory factors of oral disease, certain strains of Lactobacillus adhere rapidly to surfaces in the oral cavity.10
The administration of Lacticaseibacillus rhamnosus and Limosilactobacillus reuteri inhibit the proliferation and adhesion of periodontopathogenic bacteria, namely Porphyromonas gingivalis and Prevotella intermedia, both causative agents of gingivitis and periodontitis.4 Furthermore, L. rhamnosus is able to adhere to tooth surfaces and inhibit the growth of caries-forming bacteria, such as Streptococcus mutans and Prevotella intermedia, by 70% to 90%.5
L. acidophilus also targets S. mutans.11 Reducing dental biofilm through the probiotic administration of L. salivarius, in combination with xylitol, is helpful, especially in patients who smoke.5
Once adhered to surfaces in the oral cavity, probiotics function in various ways. They work directly on the tooth surface through close contact with biofilm and indirectly by balancing the mucosal immune system and preventing biofilm formation.10 The inhibition of biofilm and reduction in the adherence of harmful bacteria contributes to a more balanced pH environment.12 Probiotic therapies may counter the unbalanced oral microbiome.10 Other factors relating to bacterial colonization in the oral cavity include salivary content and pH.
Function of Saliva and Oral pH
The dietary habits and general health of the host influence salivary composition, oral pH, and the overall oral microbiome.5 The microorganisms that comprise the oral microbiome nourish saliva and help maintain oral homeostasis. Saliva plays a critical role in the maintenance of optimal oral health, as it contains various bactericidal, bacteriostatic, and inhibitory proteins that serve to create an ecological balance.10,13
Saliva is composed of electrolytes, glycoproteins, and enzymes that lubricate and protect the oral mucosa, aid in digestion, and provide sensation to taste.3 Additionally, saliva contains various host defense factors that contribute to calculus formation and influence the process of periodontal diseases.14
Alteration in salivary conditions, including salivary flow rate and pH, results in changes in the oral environment. Reduced salivary flow can cause dry mouth and interfere with salivary composition. Variance in salivary flow rate may be caused by a change in diet, emotional and/or psychological stress, systemic disease, size of the salivary glands, body weight, age, lack of exercise, and use of medications.15
The buffering capacity of salivary pH plays an important role in maintaining the integrity of the oral cavity.16 Oral pH is maintained near neutrality (6.7 to 7.3) by saliva in two ways. First, salivary flow removes acids produced by bacteria and eliminates carbohydrates that could be metabolized by bacteria.14 Second, acidity from certain foods, drinks, and bacterial activity is neutralized by the buffering mechanism of saliva.
Typically, a salivary pH of 7.0 indicates an environment conducive to oral health, as the incidence of caries and calculus accumulation is low. Acidemia (salivary pH below 7.0) is harmful to the oral cavity, as it encourages the proliferation of bacteria.14,15 Additionally, a too-low pH creates an acidic environment that dissolves the hard tissues, such as enamel and dentin, raising caries risk.10,13 Probiotics may help to increase salivary flow rate, as well as neutralize acidic pH in the oral cavity, thereby inhibiting pathogenic growth.15
Balancing Salivary pH with Probiotic Therapy
Probiotic therapy can help establish oral homeostasis and maintain a balanced salivary pH.17 Probiotics restore oral homeostasis by inhibiting pathogens, stabilizing salivary pH, and modifying the immune response.18 Consuming foods with probiotics neutralizes the acidic conditions of the mouth.19 When incorporated into dairy products, probiotics help balance salivary pH and mitigate common oral diseases such as dental caries.19,20
Probiotics compete with acidogenic oral microorganisms and reduce their numbers, thereby decreasing acid production and increasing salivary pH.20 The increase in pH alkalinity in saliva promotes an uptake in remineralization as the tooth surface evolves into its most absorbent state. Additionally, balancing salivary pH with the use of probiotics inhibits caries.13 Dosage may also affect probiotic efficacy; however, further research is needed to identify ideal strains and modes of delivery.21
Vehicles of Probiotic Administration
While several vehicles of probiotic administration are available, the most commonly studied are dairy products. Universally available, dairy is a safe option due to its natural proteins, calcium, and phosphates. Daily consumption of cheese, yogurt, and curd has been shown to reduce biofilm accumulation.22
Natural remedies that include green tea and probiotics may support effective self-care. Green tea is enriched with epigallocatechin gallate, a powerful antioxidant. When this antioxidant is combined with L. salivarius, it can reduce caries, periodontitis, and oral malodor.23 Probiotic supplements also come in mouthrinses, gum, tablets, capsules, chewables, and lozenges.
Although the mechanical removal of biofilm is the most effective form of disease prevention, implementing a topical probiotic via mouthrinse can help reduce plaque and gingival indices.24 Research suggests that probiotic mouthrinses can be as effective as chlorhexidine gluconate and sodium fluoride rinses.25
Probiotic chewing gum may be especially helpful for patients with gingivitis. Short-term exposure to probiotic chewing gum containing L. reuteri may reduce pro-inflammatory cytokines in gingival crevicular fluid, thereby decreasing the cytokine storm associated with gingival inflammation.26
Probiotic lozenges can promote the growth of good bacteria in the oral cavity while simultaneously increasing antibody production. A 4-week clinical study found that the intake of probiotic lozenges reduced the amount of S. mutans by 45% after 2 weeks and 72% by the end of the study.27 Additional studies have shown that, when combined with scaling and root planing, probiotic lozenges are effective in controlling periodontal inflammation.21
Role of the Dental Hygienist
Research indicates that an unbalanced oral microbiome can contribute to biofilm accumulation, caries, gingivitis, periodontitis, and oral malodor.1 The clinical treatment, oral hygiene instruction, and nutritional counseling provided by dental hygienists are integral to the efficacy of probiotic therapy on oral homeostasis.
The administration of probiotic bacteria has been found to suppress the odor-producing sulfur compounds that cause oral malodor.10,16 Circumvallate papillae harbor an abundance of anaerobic bacteria associated with malodor.
Probiotic therapy has the potential to improve oral health among patients of all ages when used in conjunction with professional oral health maintenance, as well as proper self-care and nutrition.10
To incorporate probiotics into nutritional counseling, dental hygienists may recommend a change in diet and/or the inclusion of supplements. Fermented food, also known as functional food, are nutrient-rich foods that may be suggested for their additional health benefits. They are enriched with probiotics and play a role in disease prevention by reducing the growth of pathogenic bacteria, increasing the defense of mucosal tissues, and aiding in the repair and prevention of infection.28
Compared to fresh or raw foods, the fermentation process increases shelf life by stripping foods of toxic and perishable compounds, which preserves beneficial nutrients over time.28 Examples include yogurt, cheese, tempeh, miso soups, sauerkraut, kefir, and preserved vegetables.10
Conclusion
More patients are seeking natural solutions to health problems. While probiotics are most frequently associated with gastrointestinal health, they have gained attention for their oral health benefits.
Growing evidence suggests that probiotic therapy may play a beneficial role in the treatment of chronic inflammatory diseases, such as periodontitis, as well as the maintenance of overall health. Probiotics improve salivary flow and pH, which play an important role in the prevention of oral infection and help maintain oral homeostasis. Further research is needed to establish the optimal delivery methods and treatment schedules for effective probiotic therapy.
References
- Allaker RP, Stephen AS. Use of probiotics and oral health. Curr Oral Health Rep. 2017;4:309–318.
- Pathak JL, Yan Y, Zhang Q, Wang L, Ge L. The role of oral microbiome in respiratory health and diseases. Respir Med. 2021;185:106475.
- Chhabra T, Sanghvi U, Sethuraman R. Effect of probiotics on the amount and pH of saliva in edentulous patients: a prospective studyJ J Indian Prosthodont Soc. 2018;18:277.
- Saïz P, Taveira N, Alves R. Probiotics in oral health and disease: a systematic review. Appl Sci (Basel). 2021;11:8070.
- Chugh P, Dutt R, Sharma A, Bhagat N, Dhar MS. A critical appraisal of the effects of probiotics on oral health. J Funct Foods. 2020;70:103985.
- McFarland LV. From yaks to yogurt: the history, development, and current use of probiotics. Clin Infect Dis. 2015;60(Suppl 2):S85–90.
- Wang X, Zhang P, Zhang X. Probiotics regulate gut Microbiota: An effective method to improve immunity. Molecules. 2021;26:6076.
- Shi LH, Balakrishnan K, Thiagarajah K, Mohd Ismail NI, Yin OS. Beneficial properties of probiotics. Trop Life Sci Res. 2016;27:73–90.
- Kilian M, Chapple ILC, Hannig M, et al. The oral microbiome—an update for oral healthcare professionals. Br Dent J. 2016;221:657–666.
- Jain P, Sharma P. Probiotics and their efficacy in improving oral health: a review. Journal of Applied Pharmaceutical Science. 2012;2(11):151–163.
- Fang F, Xu J, Li Q, Xia X, Du G. Characterization of a Lactobacillus brevis strain with potential oral probiotic properties. BMC Microbiol. 2018;18:221.
- Srivastava S, Saha S, Kumari M, Mohd S. Effect of probiotic curd on salivary pH and Streptococcus mutans: a double blind parallel randomized controlled trial. J Clin Diagn Res. 2016;10:13–16.
- Kamalaksharappa SK, Rai R, Babaji P, Pradeep MC. Efficacy of probiotic and green tea mouthrinse on salivary pH. J Indian Soc Pedod Prev Dent. 2018;36:279–282.
- Baliga S, Muglikar S, Kale R. Salivary pH: a diagnostic biomarker. J Indian Soc Periodontol. 2013;17:461–465.
- Damayanti T, Suharsini M, Budiardjo S. Effect of probiotics on salivary flow rate and ph in children with acute lymphocytic leukemia (all) during chemotherapy. Iranian Journal of Blood and Cancer. 2021;13(4):119–124.
- Gueimonde L, Vesterlund S, García-Pola MJ, et al. Supplementation of xylitol-containing chewing gum with probiotics: a double blind, randomised pilot study focusing on saliva flow and saliva properties. Food Funct. 2016;7:1601–1609.
- Lamont RJ, Koo H, Hajishengallis G. The oral microbiota: dynamic communities and host interactions. Nat Rev Microbiol. 2018;16:745–759.
- Angarita-Díaz MP, Forero-Escobar D, Cerón-Bastidas XA, et al. Effects of a functional food supplemented with probiotics on biological factors related to dental caries in children: a pilot study. Eur Arch Paediatr Dent. 2020;21:161–169.
- Devine DA, Marsh PD. Prospects for the development of probiotics and prebiotics for oral applications. J Oral Microbiol. 2009;1:1949.
- Nadelman P, Magno MB, Masterson D, da Cruz AG, Maia LC. Are dairy products containing probiotics beneficial for oral health? A systematic review and meta-analysis. Clin Oral Investig. 2018;22:2763–2785.
- Raff A, Hunt LC. Probiotics for periodontal health: a review of the literature. J Dent Hyg. 2012;86:71–81.
- Holban G. Milk-Based Beverages: Volume 9: The Science of Beverages. Sawston, United Kingdom: Woodhead Publishing; 2019.
- Higuchi T, Suzuki N, Nakaya S, et al. Effects of Lactobacillus salivarius WB21 combined with green tea catechins on dental caries, periodontitis, and oral malodor. Arch Oral Biol. 2019;98:243–247.
- Nadkerny P, Ravishankar P, Pramod V, Agarwal L, Bhandari S. A comparative evaluation of the efficacy of probiotic and chlorhexidine mouthrinses on clinical inflammatory parameters of gingivitis: a randomized controlled clinical study. J Indian Soc Periodontol. 2015;19:633.
- Jothika M, Vanajassun PP, Someshwar B. Effectiveness of probiotic, chlorhexidine and fluoride mouthwash against Streptococcus mutans – Randomized, single-blind, in vivo study. J Int Soc Prev Community Dent. 2015;5(Suppl 1):S44–48.
- Twetman S, Derawi B, Keller M, Ekstrand K, Yucel-Lindberg T, Stecksén-Blicks C. Short-term effect of chewing gums containing probiotic Lactobacillus reuterion the levels of inflammatory mediators in gingival crevicular fluid. Acta Odontol Scand. 2009;67:19–24.
- Lin CW, Chen YT, Ho HH, et al. Lozenges with probiotic strains enhance oral immune response and health. Oral Dis. 2022;28:1723–1732.
- Milanda T, Soemarie Y, Barliana M. Fermented foods as probiotics: a review. J Adv Pharm Technol Res. 2021;12:335.
From Dimensions of Dental Hygiene. March 2023; 21(3)28,31-33.



