 PEOPLEIMAGES/E+/GETTY IMAGES PLUS
PEOPLEIMAGES/E+/GETTY IMAGES PLUS
The Importance of Interpersonal Communication Skills
Patient care and team building are supported by highly effective interpersonal communication skills.
This course was published in the September 2018 issue and expires September 30, 2021. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define interpersonal communication.
- List beneficial patient outcomes of interpersonal care.
- Identify the key components of motivational interviewing.
- Describe how interpersonal communication promotes team building and collaboration.
Dentistry is a people-focused profession, in which good communication skills are essential. Patient care requires effective communication to assess and accurately address a patient’s chief complaint, triage emergencies, establish a common goal during treatment planning, and to ensure informed consent is obtained. In health care, strong interpersonal communication skills can help to improve patients’ health outcomes and satisfaction levels.1–4 By using the tenets of effective interpersonal communication, clinicians can improve verbal and nonverbal communication skills, effectively manage conflict, improve cultural sensitivity, increase the accuracy of their perceptions, and strengthen team collaboration.
Interpersonal communication is defined as a face-to-face exchange of information, feelings, and meaning through verbal and nonverbal messages. It is a distinctive form of human communication involving shared influences, usually for the purpose of managing relationships.5 This communication occurs between two people who hold a sociologically significant relationship in which a clear connection has been established. In a humanistic perspective, interpersonal communication includes openness, empathy, supportive behavior, and commonality. In a pragmatic perspective, interpersonal communication includes self-confidence, togetherness, interaction management, and expressive behavior. Ultimately the goal of interpersonal communication is to foster an effective interaction.6
People spend approximately 80% to 90% of their day communicating with others.5 However, many face-to-face interactions occur without unique knowledge of the other person, creating an impersonal or noninterpersonal interaction. Interpersonal communication follows an “other-oriented” approach and is essential in patient care, as it treats interactions with each individual as a unique, authentic entity.5 When translated into the dental operatory, this reflects a patient-centered approach.
BENEFITS
As interpersonal communication focuses on common goals, empathy, and collaboration, it is useful when educating patients on their oral health status and treatment needs. Studies show that empathy is critical to patient care6–10 and the development of a trusting relationship.4,6,7 In primary care, the Consultation and Relational Empathy (CARE) measure is widely used to assess patients’ perceptions of practitioners’ interpersonal empathy.4,7,9 Bikker et al7 assessed the validity of CARE among nurses during primary care consultations. This study focused on the practitioner’s ability to:
- Understand the patient’s situation, perspective, and feelings along with their attached significances
- Communicate that understanding back to the patient and confirm accuracy, and
- Act on that understanding with the patient in a helpful way by addressing the patient’s needs
Results showed an empathetic approach garnered higher levels of patient satisfaction than a nonempathetic approach.7 The use of an empathetic approach also resulted in patients taking ownership for their role in the health care partnership. Interpersonal communication between patients and oral health professionals can lead to better adherence4 to pre-operative and post-operative care management, decreasing post-operative complications. Effective communication has also shown to improve diagnostic accuracy.4 These findings suggest that an interpersonal approach may result in better health outcomes.2,4,6,11 Effective communication may also decrease the risk of malpractice litigation.12
Communication between providers and patients is a critical element of quality health care. Effective communication enhances patient awareness and provides patients with a comprehensive understanding of their current health/disease status. As inferences are drawn each time new information is presented, miscommunication can happen even when information is presented accurately. Interpersonal communication decreases the fragmented nature of the patient-provider interaction, increasing clarity.
A patient’s inability to recall information causes significant consequences for treatment compliance.13 An estimated 40% to 80% of information provided to patients is immediately forgotten or remembered incorrectly.13 Interpersonal communication increases the probability patients accurately understand the information presented.14
MOTIVATIONAL INTERVIEWING
Motivational Interviewing is a form of patient-centered communication designed to facilitate resolution and promote positive behavior changes.15,16 This collaborative communication style strengthens patient motivation and is effective in chronic disease management, disease prevention, and reducing risk of comorbidity.17,18 Motivational interviewing is an evidence-based method that stimulates positive change through personal motivation and aims to establish healthy behaviors by reducing ambivalence.16,19
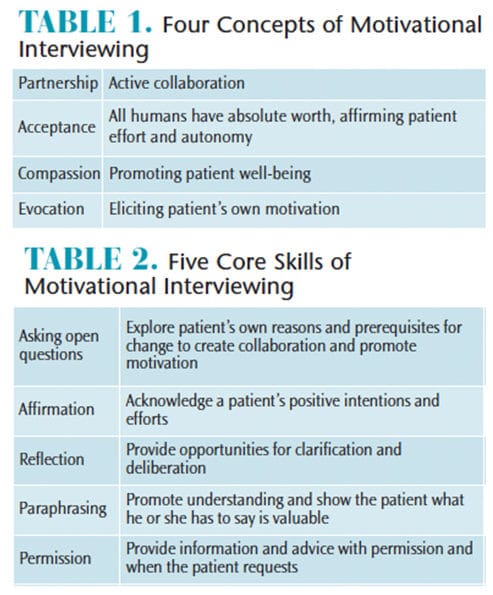
The four elements of motivational interviewing are partnership, acceptance, compassion, and evocation. Core skills required to practice motivational interviewing are asking open-ended questions, affirmation, reflection, paraphrasing, and asking permission to give advice (Table 1 and Table 2).17 Motivational interviewing facilitates resolution of patient issues that inhibit healthy behaviors. Dental hygienists should become comfortable practicing this technique, as it enhances patient compliance and produces better health outcomes.15,17 To reduce ambivalence, dental hygienists should explore both sides of the situation. For example, ask the patient about the benefits of treatment, along with the involved risk of nontreatment.
CONFLICT MANAGEMENT
Conflict can negatively impact team efficacy and productivity and weaken stability.20 Interpersonal communication is critical for effective conflict management. Conflict can arise simply from the awareness of differences in opinion, values, and beliefs between co-workers and patients. Conflict within a dental team could involve distribution of work load, quality of relationships, and processes or protocols. These types of conflict directly impact employee performance.20,21 Reduced performance has been shown to negatively impact patient care.20 Additionally, poorly managed conflict is correlated with stress, sickness, reduced job satisfaction, and distrust. With proper management, conflict can be constructive vs destructive and promote growth and collaboration.20,21 Interpersonal communication provides steps to decrease the risk of conflict escalating to a point in which the environment inhibits understanding and views conflict as a normal and productive part of group deliberations.5 Five interpersonal skills that improve conflict management are: effective communication, assertiveness, anger management, conflict resolution, and team work.22
Assertiveness provides a decisive delivery and ensures that the message given is clear and concise. Assertiveness benefits patients when discussing disease status and treatment needs by minimizing confusion. To promote clarity, clinicians should summarize in their own words what the other person has said and provide opportunity for the patient to do the same. This helps to ensure a collaborative comprehensive understanding is achieved. This “interactive communication loop” is known as the teach-back method.13,23
The teach-back method is a best practice communication technique that invites the patient to take part in the interaction.13,23 When used effectively, the teach-back method improves communication accuracy and health outcomes and is regarded as an important patient safety practice.13
Anger management is part of conflict resolution as it removes the negative and hostile emotion from disagreements. Conflict management is key to good patient-provider relationships and positive relationships among co-workers. It is essential in a team setting to replace negative emotions with positive ones to foster a supportive environment. When discussing treatment plans with patients, the patient should be supported, rewarded, and acknowledged for any positive behavior or improvements in his or her oral health or self-care routine.
When managing conflict, interpersonal communication stresses collaboration as the best, most effective, conflict management style. Dental teams should view conflict as a set of problems to be solved rather than a game to win.5 Interpersonal communication suggests awareness, involvement, and understanding to promote equality and improve conflict management. Practicing collaboration encourages provider accountability to help manage emotions appropriately, thus separating the person from the problem to emphasize common interests, common values, and to establish common goals (Figure 1).
SELF-ORIENTED VS PATIENT-CENTERED GOALS

provider accountability to help manage emotions
appropriately.
All goals should be patient-centered and must address the patient’s unmet needs.15 In practice, a clinician’s goals may be self-oriented to include production, as it relates to systems and processes. Often the clinician’s idea of treatment outcomes may seem different from the patient’s goals. Dental hygienists might have a production goal and the patient might have a goal for a more esthetic smile. With an open exchange of information and collaboration, both goals can be met. The dental hygienist could discuss the benefits of a prophylaxis using ultrasonics and air polishing, with adjuncts of whitening trays and fluoride, all of which increase production, while still addressing the patient’s desire for a more esthetic smile. Oral health professionals should prioritize the patient’s goals over self-oriented goals and develop a trusted relationship. Darby et al15 suggest clinicians consider the following four patient-centered goal categories:
- Cognitive: to increase knowledge or understanding
- Psychomotor: to enhance skill
- Affective: to change values, beliefs, and attitudes
- Oral health: to address disease and establish health
CULTURAL SENSITIVITY
Diversity in the United States has changed dramatically over the past decade. With this increase in diversity, comes a need for cultural sensitivity when providing dental care. Implementing cultural sensitivity during the process of care allows clinicians to provide quality care, minimizing insensitivities to difference. Cultural sensitivity plays a considerable role in interpersonal communication and is defined as having the awareness that cultural differences exist and affect a person’s values, learning, and behavior.15
When there is a high degree of cultural diversity, both the patient and clinician experience culture shock. This sense of confusion, anxiety, or stress is correlated with the interaction of an unfamiliar culture.5 Oral health professionals need to understand how culture impacts treatment planning. Providing quality dental care to patients requires culturally competent oral health professionals. This involves becoming aware of personal biases and the ability to treat each dissimilarity with respect, validation, and openness.15 Clinicians should be open to learning about different cultures and how they may impact treatment and the delivery of care.
Perceptions between clinicians and patients may be different when a high degree of racial diversity exists. A study focusing on teachers’ and students’ perceptions based on ethnicity showed that the ethnic background of a teacher was correlated with his or her perceived helpfulness, friendliness, and strictness.24 The same study demonstrated that how teachers perceive themselves may be skewed and that typically teachers rated themselves higher in areas such as personal interaction with students, encouraging student interaction, support, helpfulness, friendliness, task orientation, providing order, and clarification of rules.24 Accurate perceptions prevent miscommunication and correlate with interpersonal communication and cultural competence, whereby both parties feel supported and, more important, accurately understood. Improving interpersonal communication allows clinicians to more accurately be perceived by their patients and team members. This, again, encourages an other-oriented approach by seeking and facilitating continual feedback and establishing clarity.
IMPROVING INTERPERSONAL COMMUNICATION
When discussing disease, therapy, and self-care techniques, clinicians need to explain to patients their current disease status, future prevention strategies, therapy recommendations, and the prognosis after therapy to allow patients to make informed decisions when consenting to treatment. As with all patient-centered care, the process of establishing informed consent is accomplished by various exchanges of information that open the opportunity for miscommunication. As professionalism demands effective communication, oral health professionals must invest time in developing and maintaining interpersonal communication skills.
It is a common misconception that communication skills are innate and cannot be learned or developed through practice and training.7,9,11,15 Multiple studies have shown that the efficacy of communication improves when communication training is integrated in health care education.18,25 These studies also correlated additional communication training with increased confidence levels when communicating with patients. This perception positively influenced the patient’s trust in the clinician, leading to higher patient satisfaction levels.3 Good clinician-patient communication is important in maintaining relationships. Patients place higher value on health providers who take time to listen and present clear treatment plans. As with many skill sets, communication loses its effectiveness when not practiced.2 Oral health professionals should invest time in reinforcing interpersonal skills, as they have been linked to increased patient satisfaction, provider-patient trust, improved health outcomes, and patient compliance.2–4,6,11,12
CONCLUSION
Interpersonal communication is essential for team building and patient care. When oral health professionals are attune to others’ unique situations, a more cohesive relationship that values shared goals is created. Interpersonal communication draws a parallel to quality assurance, as interpersonal-based encounters positively influence patient satisfaction and health outcomes. This empathetic and patient-centered approach not only improves the health outcomes of patients but fosters patient accountability. Additionally, the collaborative nature of interpersonal communication promotes progressive development and growth of a practice, as conflict is met with solutions that work for each person. Dental teams that practice interpersonal communication will ultimately be more efficient, productive, produce healthier more satisfied patients, and have better patient retention rates.
REFERENCES
- Berger CR. Interpersonal communication. In: Handbooks of Communication Science. 6th ed. Berlin: De Gruyter Mouton; 2014:3.
- Choudhary A, Gupta V. Teaching communications skills to medical students: Introducing the fine are of medical practice. Int J App Basic Med Res. 2015;5:S41–S44.
- Chang CS, Chen SY, Lan YT. Service quality, trust, and patient satisfaction in interpersonal-based medical encounters. BMC Health Serv Res. 2013;13:22.
- Wirtz M, Boecker M, Forkmann T, Neumann M. Evaluation of the “Consultation and Relational Empathy”(CARE) measure by means of Rasch-analysis at the example of cancer patients. Patient Educ Couns. 2011;82:298–306.
- Beebe SA, Beebe SJ, Redmond MV. Interpersonal Communication: Relating to Others. 4th ed. Boston: Pearson Education Inc; 2005:5–6, 94–99, 203–226.
- Hutagalung I. The function of interpersonal communication in conflict management organization. Available at: shs-conferences.org/ articles/shsconf/abs/2017/01/shsconf_icome2017_00009/shsconf_icome2017_00009.html. Accessed August 27, 2018.
- Bikker AP, Fitzpatrick B, Murphy D, Mercer SW. Measuring empathic, person-centred communication in Primary Care Nurses: validity and reliability of the Consultation and Relational Empathy (CARE) Measure. BMC Fam Pract. 2015;16:149.
- Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the “nature” and “specific effectiveness” of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns. 2009;74:339–346.
- Mercer SW, Neumann M, Wirtz M, Fitzpatrick B, Vojt G. General practitioner empathy, patient enablement, and patient-reported outcomes in primary care in an area of high socio-economic deprivation in Scotland—a pilot prospective study using structural equation modeling. Patient Educ Couns. 2008;73:240–245.
- Rakel DP, Hoeft TJ, Barrett BP, Chewning BA, Craig BM, Niu M. Practitioner empathy and the duration of the common cold. Fam Med. 2009;41:494.
- Perron NJ, Sommer J, Louis-Simonet M, Nenddaz M. Teaching communication skills: beyond wishful thinking. Available at: researchgate.net/publication/ 272096880_Teaching_communication_skills_Beyond_wishful_thinking. Accessed August 27, 2018.
- Raper SE, Gupta M, Okusanya O, Morris JB. Improving communication skills: a course for academic medical center surgery residents and faculty. J Surg Educ. 2015;72:e202–e211.
- Morony S, Weir K, Duncan G, Biggs J, Nutbeam D, Mccaffery KJ. Enhancing communication skills for telehealth: development and implementation of a Teach-Back intervention for a national maternal and child health helpline in Australia. BMC Health Serv Res. 2018;18:162.
- Zwarenstein M, Rice K, Gotlib-Conn L, Kenaszchuk C, Reeves S. Disengaged: a qualitative study of communication and collaboration between physicians and other professions on general internal medicine wards. BMC Health Serv Res. 2013;13:494.
- Darby ML, Walsh MM, Bowen,DM. Dental Hygiene: Theory and Practice. St. Louis: Elsevier/Saunders; 2015:67–71, 381.
- Douglass JM, Clark MB. Integrating oral health into overall health care to prevent early childhood caries: need, evidence, and solutions. Pediatric Dent. 2015;37:266–274.
- Östlund AS, Kristofferzon ML, Häggström E, Wadensten B. Primary care nurses’ performance in motivational interviewing: a quantitative descriptive study. BMC Family Prac. 2015;16:89.
- Schoo AM, Lawn S, Rudnik E, Litt JC. Teaching health science students foundation motivational interviewing skills: use of motivational interviewing treatment integrity and self-reflection to approach transformative learning. BMC Med Educ. 2015;15:228.
- Johansson AC, Johannsen G, Uhlin L, Johannsen A. Dental hygienist students’ learning about motivational interviewing. Dentistry Journal. 2014;2(2):65–77.
- McKibben L. Conflict management: importance and implications. Br J Nurs. 2017;26:100–113.
- Mulki JP, Jaramillo F, Goad EA, Pesquera MR. Regulation of emotions, interpersonal conflict, and job performance for salespeople. Journal of Business Research. 2015;68(3):623-–630.
- Boyd C, Dare J. Communication Skills for Nurses. Chichester, West Sussex, United Kingdom: Wiley Blackwell; 2014:49–54.
- Hager DR, Hartkopf K, Margolis A, Martin BA. Pharmacist behavior changes following a medication counseling training program targeting teach-back and plain language. Innovations in Pharmacy. Available at: pubs.lib.umn.edu/index.php/ innovations/article/download/418/412/. Accessed August 27, 2019.
- Brok P, Levy J, Rodrigues R, Wubbles T. Perceptions of Asian-American and Hispanic American teachers and their students on teacher interpersonal communication style. Teaching and Teacher Education. Available at: researchgate.net/publication/ 223560224_Perceptions_of_Asian-American_and_HispanicAmerican_teachers_and_their_students_on_teacher_interpersonal_communication_style. Accessed August 27, 2018.
- MacLean S, Kelly M, Geddes F, Della P. Use of simulated patients to develop communication skills in nursing education: an integrative review. Nurse Educ Today. 2017;48:90–98.
From Dimensions of Dental Hygiene. September 2018;16(9):38–41.
The most unique information with movies is on xnxx hd videos




[…] explain how guardians and patients understand. Proper communication enhances patient awareness and provides patients with a comprehensive understanding situation, allowing them to improve their oral health […]