Implementing Dental Hygiene Diagnosis into Practice
This essential part of oral health care ensures that patients receive an effective evaluation and personalized treatment plan.
This course was published in the September 2015 issue and expires September 30, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define dental hygiene diagnosis.
- Discuss the importance of this component of patient care.
- Identify the main categories in the dental hygiene diagnosis operatory chart model.
- Explain how to implement dental hygiene diagnosis into practice.
Dental hygienists work with patients in a variety of clinical environments. The American Dental Hygienists’ Association (ADHA) established the dental hygiene process of care to ensure that every patient is evaluated and treated as an individual with unique oral health needs.1 While dental hygiene diagnosis is an essential part of dental hygiene care, confusion exists on how to implement it into daily practice.
In 2015, the ADHA defined dental hygiene diagnosis as “the identification of an individual’s health behaviors, attitudes, and oral health care needs for which a dental hygienist is educationally qualified and licensed to provide.”2 Critical thinking skills are necessary to evaluate assessment data, identify a dental hygiene diagnosis, and formulate a dental hygiene care plan.1,3 Care plans must include prevention and treatment strategies.
In addition, the Commission on Dental Accreditation defines dental hygiene diagnosis as the “identification of an existing or potential oral health problem that a dental hygienist is qualified and licensed to treat.”4 Collaboration with a dentist ensures the incorporation of the dental hygiene care plan into the patient’s overall oral health care plan.1 Dentistry involves a team approach requiring each member of the team to apply his or her expertise on the patient’s behalf. Dentists rely on dental hygienists to be the experts in preventive care.
IMPORTANCE OF DENTAL HYGIENE DIAGNOSIS
Dental hygienists are educated to identify the signs and symptoms of oral disease, as well as its etiology.1 The purpose of a dental hygiene diagnosis is to evaluate the individual dental hygiene needs of a patient after conducting a thorough examination and risk assessment. A dental hygiene diagnosis is a necessary component of patient care.2 Once a dental hygiene diagnosis has been recognized, the patient’s individualized dental hygiene care plan can be developed and implemented. The American Dental Education Association (ADEA) approved entry-level competencies for dental hygienists based on the ADHA’s process of care published in 2008.1,3 These competencies require that dental hygiene graduates be able to assess, diagnose, plan, implement, and evaluate treatment.3 The most important reason to acknowledge a dental hygiene diagnosis during patient care, however, is to provide the best advice, education, prevention strategies, self-care recommendations, treatment, and evaluation protocols possible. Discussing the dental hygiene diagnosis with patients creates the space for a dialogue between the patient and the dental hygienist regarding oral health conditions, risks, and prevention.5
The United States Department of Health and Human Services—in its nationwide initiative to improve the health of all Americans, Healthy People 2020—recognized two needs that can be addressed specifically by dental hygienists during a discussion of the dental hygiene diagnosis.6 These include raising awareness about the importance of oral health and its relationship to overall health, and encouraging the acceptance and adoption of prevention measures to improve oral health.6 The ultimate goal is to improve oral health outcomes among all patients by inviting them to partner with dental hygienists during the process.
PUTTING THE DENTAL HYGIENE DIAGNOSIS INTO PRACTICE
Table 1 includes a diagnostic operatory chart model designed to assist dental hygienists in effectively and efficiently formulating a dental hygiene diagnosis for patients. While not an exhaustive list of diagnoses, this model provides an opportunity for dental hygiene practitioners to develop skills in writing dental hygiene diagnosis statements that pertain to each patient’s unique clinical presentation. Diagnoses can relate to general and oral health conditions. Related causes and signs and symptoms can be readily identified and noted. As seen in this model, patients may exhibit multiple diagnoses, enabling dental hygienists to expand treatment plans as needed.
An important consideration is the fact that diagnostic terms are not exclusive to one health care discipline. According to Darby and Walsh,7 “a diagnosis becomes discipline specific when it is applied to the practice of that discipline.” The functions discussed in the following examples are within the dental hygiene scope of practice. For instance, a patient may present with hypertension and cardiovascular disease. While the dental hygienist may not prescribe medication to treat these medical conditions, he or she does need to take vital signs, monitor the patient during the course of treatment, evaluate for contraindications if local anesthesia is planned, reinforce healthy lifestyle behaviors, and ensure the patient’s vital signs are within normal limits at the conclusion of the dental hygiene appointment. In some cases such as when a patient has elevated blood pressure, the dental hygienist may refer the patient back to his or her physician for further evaluation.
A dental hygiene diagnosis that involves a patient who presents with the potential for emergency due to his/her history of diabetes and medication usage needs to note the patient’s increased risk of hypoglycemia. The dental hygienist would assess the patient for signs of hypoglycemia and be prepared to manage a medical emergency should one arise. In addition, because of the patient’s diabetes, the dental hygienist may examine him or her for caries and periodontal disease.
It is estimated that approximately 46,000 individuals will be diagnosed with oral and pharyngeal cancer, and 8,650 will die from this disease in 2015.8 Therefore, all patients need to receive a comprehensive oral examination at every dental hygiene appointment. Dental hygienists can assess for the potential development of head and neck cancers and educate their patients about cancer risk. It is within the scope of practice for dental hygienists to refer patients to dentists, oral and maxillofacial surgeons, or ear, nose, and throat physicians for evaluation and biopsy of any noted pathoses.
While dental caries is traditionally viewed as a dental diagnosis, it can also fall within a dental hygiene diagnosis. Dental caries risk and certain types of caries can be managed with preventive education, pit and fissure sealants, and the application of fluoride varnish and other minimally invasive treatments.
As part of the Centers for Disease Control and Prevention’s 2009-2010 National Health and Nutrition Examination Survey, a full-mouth periodontal examination was conducted on adults age 30 and older to assess for mild, moderate, or severe periodontitis. Results of this study estimated that more than 47%, or 64.7 million American adults, have some form of periodontal disease.9 Likewise, Li et al10 found evidence of significant levels of gingivitis in American adults during the same period.
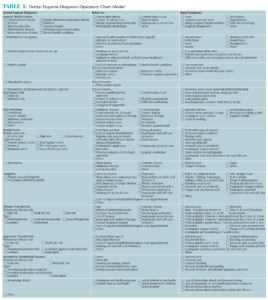
Detecting the early signs and risk factors of periodontal diseases and establishing a comprehensive dental hygiene diagnosis in order to form a cogent treatment plan can curtail the advancement of disease and eventual tooth loss.11 Periodontal assessment begins with evaluating the patient’s health status and periodontal risk factors including gender, smoking status, systemic disease, oral hygiene, socioeconomic status, and education level.11,12 A periodontal examination must be performed assessing existing biofilm, calculus, mobility, furcation involvement, tooth position, six-point probing depth, bleeding on probing, recession, and clinical attachment levels.11,13,14 Consistently performing all steps of this assessment will ensure an accurate periodontal dental hygiene diagnosis (Table 1 provides examples). Multiple factors contributing to the periodontal condition and signs and symptoms are offered as the basis for developing the diagnosis in addition to supporting patient education regarding the periodontal diagnosis and treatment indicated. Note that for each type of periodontitis identified within Table 1, the hygiene diagnostician can specify level of risk and extent of disease present.
Providing comprehensive nonsurgical periodontal therapy is within the scope of practice of the dental hygienist. Further, patients are more inclined to accept treatment when they comprehend that they have been diagnosed with disease.11 By using the model provided in Table 1, the dental hygienist can provide a thorough dental hygiene diagnosis and help patients appreciate their oral health status, underlying cause of disease, and recommended treatment protocols.
Knowledge deficit among patients is a term commonly used in nursing, but also has application in dental hygiene. As noted in Table 1, a knowledge deficit may be related to inadequate oral health education, lack of interest in oral health, and minimal exposure to evidence-based literature. Providing factual health information and preventive education are expected components of dental hygiene practice.
CONCLUSION
The dental hygiene diagnosis is an adjunct to the dental diagnosis and emphasizes the skills and professionalism required of all dental team members.5 Translational health care involves researchers, clinicians, and educators working collaboratively in order to improve overall patient health outcomes.15 In oral health, this interdisciplinary effort includes dentists, dental hygienists, dental assistants, nutritionists, physicians, and other allied health professionals incorporating specific expertise in order to promote optimum health. One key responsibility in dental hygiene practice is to develop a dental hygiene diagnosis and care plan that is integrated into the larger health care system.
The interweaving of oral health and general health is undeniable, as is the importance of patients partnering with health professionals to improve systemic health. Helping patients envision the whole picture of individual oral health is an essential aspect of the dental hygiene diagnosis.1 Dental hygienists are in a unique position as they get to spend quality time with patients fostering relationships and building trust. As this trust develops, acceptance of education and treatment recommendations will also grow.
REFERENCES
- American Dental Hygienists’ Association. Standards for Clinical Dental Hygiene Practice. Available at: adha.org/resources-docs/7261_Standards_Clinical_Practice.pdf. Accessed August 21, 2015.
- American Dental Hygienists’ Association. Dental Hygiene Diagnosis. Available at: adha.org/resourcesdocs/ Diagnosis-Position-Paper.pdf. Accessed August 21, 2015.
- Competencies for entry into the profession of dental hygiene. J Dent Edu. 2004;68:745–749.
- Commission on Dental Accreditation. Accreditation Standards for Dental Hygiene Education Programs. Available at: ada.org/~/media/CODA/Files/2016_dh.ashx. Accessed August 21, 2015.
- Jahn C. Standard II: Dental hygiene diagnosis. Access. 2015;4:25–26.
- Healthy People. Oral Health. Available at: healthypeople.gov/2020/topics-objectives/topic/oral-health. Accessed August 21, 2015.
- Darby ML, Walsh MM. Dental hygiene diagnosis. In: Dental Hygiene Theory and Practice. 4th ed. St. Louis: Saunders; 2015:361–376.
- Cancer Facts & Figures 2015. Atlanta: American Cancer Society; 2015.
- Eke PI, Dye BA, Wei, L, et al. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91:914–920.
- Li Y, Lee S, Hujoel P, et al. Prevalence and severity of gingivitis in American adults. Am J Dent. 2010;23:9–13.
- Sweeting LA, Davis K, Cobb CM. Periodontal treatment protocol (PTP) for the general dental practice. J Dent Hyg. 2008;82:16–26.
- Hodges KO. Evaluate disease potential. Dimensions of Dental Hygiene. 2015;13(6):24–26.
- American Academy of Periodontology. Parameter on comprehensive periodontology examination. J Periodontol. 2000;71:847–848.
- American Academy of Periodontology. Position Paper: Guidelines for periodontal therapy. J Periodontol. 2001;72:1624–1628.
- Mata HJ, Davis S. Translational health research: perspectives from health education specialists. Clin Transl Med. 2012;1:27.
From Dimensions of Dental Hygiene. September 2015;13(9):56–59.




[…] https://dimensionsofdentalhygiene.com/article/implementing-dental-hygiene-diagnosis-into-practice/ […]