
Create a Safety Culture
The use of an implant safety checklist can help reduce the risk of error and improve outcomes.
This course was published in the June 2015 issue and expires June 30, 2018. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify barriers to creating a safety culture in the dental practice.
- Discuss how to develop a patient-centered climate in the dental setting.
- Explain the role of the implant safety checklist.
In 1999, the United States Institute of Medicine published a report, “To Err Is Human,” which revealed that more Americans die annually due to medical errors than traffic accidents.1 This publication, among others, galvanized the relatively new discipline of patient safety and has resulted in various efforts to promote a climate of safety in health care professions. Many of the patient safety-related efforts have been focused on medicine, while dentistry has been a relative latecomer to the concept of a safety-based practice.2
Yamalik and Perea Pérez2 discussed several “peculiarities of patient safety in dentistry” that serve as barriers for development of a safety culture. For one, iatrogenic damage to patients is milder in dentistry when compared to medicine because dental procedures typically are less invasive. Deaths related to dental procedures also are relatively rare. In addition, dental care is largely unstructured and often is provided by dentists who practice in isolation. This structure limits the dissemination of knowledge regarding adverse events, as well as their analysis. Lastly, dentists have no incentive to report adverse events, considering that most dentistry is practiced in a private practice setting. This is particularly true when the event may reflect a professional error and/or may have negative financial consequences.
There are few statistics available on patient safety incidents (PSI), such as near misses or adverse events, that occur in dental practice. A large portion of the available information on PSI stems from case studies, which range from less severe events, such as local allergy to dental materials, to life threatening events like airway obstruction or even death.3,4
IMPLANT SAFETY
Recent advances in site development and implant placement techniques have made the practice of dentistry more effective, but also more dangerous.5,6 The American Academy of Implant Dentistry estimates that approximately 3 million individuals in the US have implants, and this number is growing by 500,000 annually.7 Despite the rapid expansion, several safety and quality-of-care issues need to be addressed to reduce the associated risks.8
Experience in placing implants varies widely among clinicians.9–14 In terms of quality of care, implant survival rates are relatively well-documented.15,16 For example, a meta-analysis by Pjetturson et al15 revealed that although dental implants placed by experienced surgeons had a 95% survival rate within 5 years of placement, 39% of these surviving implants were associated with at least one complication. Common problems, such as prosthetic complications, may become more serious when clinician experience is limited.16 For example, implants placed by inexperienced surgeons were shown to be twice as likely to fail as those placed by experienced surgeons.17 When clinicians make iatrogenic errors—especially those leading to patient morbidity and mortality—they face loss of licensure and other legal ramifications.18 In 2012, 11% of medical malpractice payments were against dentists.19,20
Understanding how errors occur is paramount to developing the concept of patient safety. Several models have been proposed to conceptualize patient safety. Reasons’ “Swiss cheese” model focuses on built-in preventive mechanisms that may act as barriers to errors.21 In actual practice, each barrier is more like a slice of Swiss cheese, ie, with several holes, but collectively, they prevent errors. Nevertheless, when several minor errors occur in concert, they can result in an adverse event.
Another way to think about error occurrence is the buildup of risks that lead to a near miss that eventually results in a serious PSI. Sometimes failures in organizational systems can result in human errors, such as structure that is too complex, inappropriate automation, reliance on memory for optimizing information systems, lack of physical/engineering constraints, and the effects of change on systems.22
PUT A PLAN IN PLACE
Developing a patient-centered safety climate is critical to preventing PSI.23 The goal is not to identify individuals to blame but to find system mistakes and prevent errors from occurring.2 Yamalik and Perea Pérez2 proposed the adoption of certain steps to encourage an effective safety climate. Table 1 provides a list of these steps.2
The World Health Organization (WHO) published a surgical safety checklist (available at: http://who.int/patientsafety/safesurgery/tools_resources/SSSL_Checklist_finalJun08.pdf). This checklist was developed to reduce human errors during surgical procedures and is modeled after the airline industry’s in-flight safety checklists.24–26 It includes three phases: sign in before induction of anesthesia; time out before skin incision; and sign out before the patient leaves the operating room. The operating team checks off each item before proceeding to the next phase.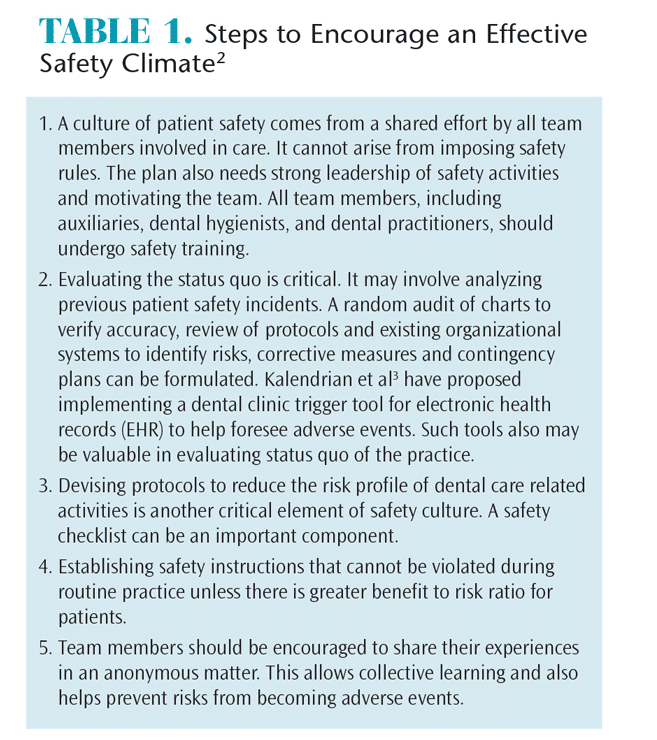
With complex clinical decision-making systems, health care practitioners face two main challenges: fallibility of memory and attention and the inadvertent skipping of clinical steps.24,27 Despite receiving extensive training, some clinicians assume that certain critical steps may not always be essential.24 This is why making key procedures explicitly routine is key. In addition, checklists provide clinicians with clear reminders of the minimum steps necessary in the procedures with the aim of avoiding or catching any significant procedural errors.24
Several studies have demonstrated the effectiveness of the WHO checklist. Many well-controlled studies have shown beneficial effects of implementing checklists in reducing patient morbidity and mortality in various hospital settings.28–30 In contrast, Urbach et al31 reported that a law mandating surgical checklist use in Ontario hospitals resulted only in a modest, statistically insignificant reduction in mortality. In light of this report, Haugen et al32 conducted a randomized clinical trial of the surgery checklist, which confirmed that its use resulted in substantial improvement in outcomes. More important, the authors detailed several factors that may have improved the efficacy of the list. First, customizing the checklist to fit the practice setting was key to its success. Also, testing the checklist on a small scale and then making further modifications was helpful. Practitioners should be free to make observations and suggestions in order to create opportunities for additional education and reinforcement.32,33
IMPLANT CHECKLIST
*Click to view
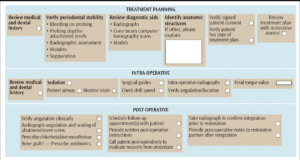
As dental implant placement is more akin to medical surgical procedures than routine dental procedures, Christman et al34 created a preliminary surgical safety checklist for dental implant placement.34–36 The expectation was that dental practitioners could then customize the preliminary framework based on individual practice needs. In the following sections, the process by which the checklist was created will be briefly discussed and key findings of this publication will be summarized.
The process involved obtaining consensus from a panel of experts to create a checklist that would provide a preliminary framework for avoiding risks. The authors administered the survey to 24 board-certified periodontists who came to a consensus on the appropriate clinical steps for the successful restoration of edentulous areas with dental implants. The panel ultimately determined that 20 items were essential to the checklist and arranged them in three phases: treatment planning, intraoperative, and post-operative (Figure 1). The broad consensus among the panelists was:
- In preparing treatment plans for patients, clinicians should verify periodontal stability, conduct a proper diagnostic work-up, and engage in effective communication with restorative partners.
- Review of the patient medical and dental history before placing implants and the use of safety checks are important.
- Post-operative care includes appropriate communication with restorative partners and patients.
- Implant maintenance is an integral part of follow-up care for patients.
In terms of treatment planning, panelists indicated that verification of patients’ periodontal stability was critical, and they emphasized the need for thorough clinical and radiographic evaluation to establish this stability. The experts also encouraged the use of appropriate diagnostic aids—such as radiographs and cone-beam computed tomography—for identification of key anatomical structures. The consequences of failing to identify and protect key anatomical structures are documented extensively in the literature. In a meta-analysis of complications related to implant placement, the most common surgical problems were associated with hemorrhage.12 The incidence of persistent or long-term altered sensation of the mental nerve after implant surgery varies from 1% to 43%.37,38
Panelists also suggested that reviewing the patient’s medical and dental history is critical to preventing medical emergencies, as well as identifying relative or absolute contraindications to implant placement. The experts agreed that formal treatment plans should be determined for complex cases. Panelists also emphasized that obtaining a signed consent form from patients for proposed treatment is necessary to protect clinicians from legal action.
In terms of intraoperative steps, all panelists concurred that a review of current medications and an exploration of any changes to the patient’s dental or medical history must be done on the day of surgery. They agreed that protection of the airway is critical, with the caveat that achieving this goal may be difficult due to space restrictions. The dental literature contains reports of sporadic occurrences of surgical instrument aspiration and associated life-threatening complications.14,39 Panelists advocated the use of safety maneuvers, such as placing gauze at the back of the throat, and reiterated the importance of monitoring vital signs during administration of conscious sedation.
Consistent with Greenstein and colleagues,40 several panel members suggested that sound clinical judgment and evaluation of bone quality are the most important factors in determining drill speeds and torque values, but no consensus was achieved. Reported causes of initial integration failures include high heat levels due to drilling and excessive pressure at the implant-bone interface (greater torque values) at the time of implant insertion, which may result in retrograde peri-implantitis lesions.41
Panelists indicated that intraoperative radiographs are essential in areas with limited space due to anatomical constraints, and they suggested that verifying implant angulation and positioning with the help of a qualified assistant and obtaining final radiographs after implant placement are good clinical practices.
Tarnow et al42 reported that improper mesio-distal angulation and positioning of implants can lead to lateral bone loss, as well as unacceptable esthetic results. Invasion of the periodontal ligament space and devitalization of adjacent teeth due to improper angulation and positioning are additional concerns related to improper placement of implants.43
In terms of post-operative steps, the panelists advocated prescribing chlorhexidine mouthrinses, providing patients with written post-operative instructions, communicating after surgery with restorative partners, making follow-up telephone calls to patients, and scheduling follow-up appointments as being essential clinical practices.8,40 Reported post-operative infection rates are low, but they can lead to serious adverse events beyond the oral cavity.8 Therefore, following a prescribed, standardized safety checklist may prove useful in reducing errors associated with implant placement.
CONCLUSION
While the medical field is making tremendous strides in promoting a safety culture, dentistry is behind in this area. Some of the factors that are instrumental to initiating a safety culture in the dental setting include:
- Create strategies that promote group orientation and reduce influence of hierarchy.
- Provide and promote multidisciplinary training as part of dental education and continuing education programs.
- Develop quality improvement tools to gather databases of PSIs, as well as further development, improvement, and implementation of checklists.
- Customize checklists and encourage ownership by all members of the dental team.
Christman et al34 made the first attempt to design a standardized safety checklist for dental implant surgeries. Further research is needed to evaluate improvements in outcomes. Unique implementation challenges related to dentistry need to be identified. While adverse events may occur less frequently in dentistry than in medicine, they can still exert serious consequences on patient health and quality of life. A culture of safety and the use of checklists will not only benefit patients but practitioners, as well.
REFERENCES
- Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
- Yamalik N, Perea Pérez B. Patient safety and dentistry: what do we need to know? Fundamentals of patient safety, the safety culture and implementation of patient safety measures in dental practice. Int Dent J. 2012;62:189–196.
- Kalenderian E, Walji MF, Tavares A, Ramoni RB. An adverse event trigger tool in dentistry: a new methodology for measuring harm in the dental office. J Am Dent Assoc. 2013;144:808–814.
- Hiivala N, Mussalo-Rauhamaa H, Murtomaa H. Patient safety incidents reported by Finnish dentists; results from an internet-based survey. Acta Odontol Scand. 2013;71:1370–1377.
- Chantler C. The role and education of doctors in the delivery of health care. Lancet. 1999;353:1178–1181.
- Zitzmann NU, Hagmann E, Weiger R. What is the prevalence of various types of prosthetic dental restorations in Europe? Clin Oral Implant Res. 2007;18:20–33.
- American Academy of Implant Dentistry. Dental Implant Facts and Figures. Available at: aaid.com/about/press_room/dental_implants_faq.ht ml. Accessed May 22, 2015.
- Greenstein G, Cavallaro J, Romanos G, Tarnow D. Clinical recommendations for avoiding and managing surgical complications associated with implant dentistry: a review. J Periodontol. 2008;79:1317–1329.
- Stillman N, Douglass CW. The developing market for dental implants. J Am Dent Assoc. 1993;124:51–56.
- Vasak C, Fiederer R, Watzek G. Current state of training for implant dentistry in Europe: a questionnaire-based survey. Clin Oral Implants Res. 2007;18:668.
- Melo MD, McGann G, Obeid G. Survey of implant training in oral and maxillofacial surgery residency programs in the United States. J Oral Maxillofac Surg. 2007;65:2554–2558.
- Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121–132.
- Bartling R, Freeman K, Kraut RA. The incidence of altered sensation of the mental nerve after mandibular implant placement. J Oral Maxillofac Surg. 1999;57:1408–1410.
- Bergermann M, Donald PJ, àWengen DF. Screwdriver aspiration: a complication of dental implant placement. Int J Oral Maxillofac Surg. 1992;21:339–341.
- Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implant Res. 2007;18:97–113.
- Kourtis SG, Sotiriadou S, Voliotis S, Challas A. Private practice results of dental implants. Part i: survival and evaluation of risk factors-part ii: surgical and prosthetic complications. Implant Dent. 2004;13:373-385.
- Lambert PM, Morris HF, Ochi S. Positive effect of surgical experience with implants on second-stage implant survival. J Oral Maxillofac Surg. 1997;55(Suppl 5):12–18.
- Edwards A. Dentist sued after tools fall in patient. The Orlando Sentinel. July 19, 2009. 19. United States Department of Health and Human Services. Data Bank Annual Report: 2002. Available at: npdb.hrsa.gov/resources/annualRpt.jsp. Accessed May 22, 2015.
- Givol N, Taicher S, Halamish-Shani T, Chaushu G. Risk management aspects of implant dentistry. Int J Oral Maxillofac Implant. 2002;17:258–262.
- Reason J. Human error: models and management. BMJ. 2000;320:768–770.
- Bailey E, Tickle M, Campbell S. Patient safety in primary care dentistry: where are we now? Br Dent J. 2014;217:339–344.
- Milne JK, Bendaly N, Bendaly L, Worsley J, Fitzgerald J, Nisker J. A measurement tool to assess culture change regarding patient safety in hospital obstetrical units. J Obstet Gynaecol Can. 2010;32:590–597.
- Gawande A. The Checklist Manifesto: How to Get Things Right. New York: Metropolitan Books; 2010.
- Semel ME, Resch S, Haynes AB, et al. Adopting a surgical safety checklist could save money and improve the quality of care in US hospitals. Health Aff. 2010;29:1593–1599.
- Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. New Engl J Med. 2009;360:491–499.
- Gawande AA, Thomas EJ, Zinner MJ, Brennan TA. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126:66–75.
- Van Klei WA, Hoff RG, Van Aarnhem EEHL, et al. Effects of the introduction of the WHO “Surgical Safety Checklist” on in-hospital mortality: a cohort study. Ann Surg. 2012;25:44–49.
- De Vries EN, Prins HA, Crolla RM, et al. Effect of a comprehensive surgical safety system on patient outcomes. New Engl J Med. 2010;363:1928–1937.
- Neily J, Mills PD, Young-Xu Y, et al. Association between implementation of a medical team training program and surgical mortality. JAMA. 2010;304:1693–1700.
- Urbach DR, Govindarajan A, Saskin R, Wilton AS, Baxter NN. Introduction of surgical safety checklists in Ontario, Canada. New Engl J Med. 2014;370:1029–1038.
- Haugen AS, Søfteland E, Almeland SK, et al. Effect of the World Health Organization checklist on patient outcomes. Ann Surg. 2015;261:821–828.
- Pinsky HM, Taichman RS, Sarment DP. Adaptation of airline crew resource management principles to dentistry. J Am Dent Assoc. 2010;141:1010–1018.
- Christman A, Schrader S, John V, Zunt S, Maupome G, Prakasam S. Designing a safety checklist for dental implant placement: A Delphi study. J Am Dent Assoc. 2014;145:131–140.
- Whittle JG, Grant AA, Sarll DW, Worthington HV. The Delphi technique: its use in dental health services research assessed in a study to improve care for elderly mentally ill patients. Community Dent Health. 1987;4:205–214.
- Cramer CK, Klasser GD, Epstein JB, Sheps SB. The Delphi process in dental research. J Evid Based Dent Pract. 2008;8:211–220.
- Ellies LG, Hawker PB. The prevalence of altered sensation associated with implant surgery. Int J Oral Maxillofac Implants. 1993;8:674–679.
- Wismeijer D, Van Waas MAJ, Vermeeren J, Kalk W. Patients’ perception of sensory disturbances of the mental nerve before and after implant surgery: a prospective study of 110 patients. Br J Oral Maxillofac Surg. 1997;35:254–259.
- Worthington P. Ingested foreign body associated with oral implant treatment: report of a case. Int J Oral Maxillofac Implant. 1996;11:679–681.
- Greenstein G, Cavallaro JS Jr, Tarnow DP. Clinical pearls for surgical implant dentistry: Part I. Dent Today. 2010;29:124–127.
- Quirynen M, Mraiwa N, Van Steenberghe D, Jacobs R. Morphology and dimensions of the mandibular jaw bone in the interforaminal region in patients requiring implants in the distal areas. Clin Oral Implant Res. 2003;14:280–285.
- Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71:546–549.
- Sussman HI. Tooth devitalization via implant placement: a case report. Periodontal Clin Investig. 1998;20:22–24.
From Dimensions of Dental Hygiene. June 2015;13(6):67–70.



