CBCT and the Orthodontic Patient
Cone-beam computed tomography offers key benefits in all phases of orthodontics—from diagnosis to post-treatment.
This course was published in the August 2014 issue and August 31, 2017. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the role of imaging in orthodontics.
- Identify strategies for weighing the benefits of cone-beam computed tomography (CBCT) against its risks in orthodontic patients.
- List the advantages of using CBCT in orthodontics.
The use of cone-beam computed tomography (CBCT) in the dental setting offers low-cost, in-office diagnostic imaging technology capable of demonstrating three-dimensional (3D) dental and skeletal relationships, which far exceed the maxillofacial assessment capabilities of two-dimensional (2D), or traditional, radiography. In orthodontics, imaging data are integral to the clinical diagnosis of skeletal and dental conditions, soft tissues, and their inter-relationships. Increasingly, dental hygienists will be involved in educating patients about the need for CBCT examination, obtaining consent, and taking CBCT scans. This article outlines the role of CBCT imaging in orthodontics, including its advantages. The final installment of this series will discuss specific indications for CBCT in orthodontics, and will appear in a future issue.
THE ROLE OF IMAGING IN ORTHODONTICS
Imaging for orthodontic patients serves a number of purposes, depending on the stage of therapy at which it is performed. At the diagnostic stage, imaging is used as an adjunctive diagnostic modality to provide a pretreatment assessment of the orthodontic patient. Radiography can assist in determining how the osseous tissue and dental elements contribute to malocclusion or craniofacial anomaly. Information about the relationship of the soft tissue envelope to the underlying hard tissue and the soft tissue’s role in the development of malocclusion may also be gained. In addition to clinical data, radiographic images assist clinicians in formulating a provisional diagnosis and tentative treatment plan.
In the treatment stage, imaging may be used to monitor the effects of therapy on the development of the jaws; the position of the teeth, including dental root angulation; and the influence of orthopedic and orthodontic therapies on the facial profile. This is especially important prior to beginning the surgical phase of orthognathic therapy.
Imaging in the post-treatment stage is utilized to quantify the immediate outcome of treatment and to monitor the stability of the dentition over time. Imaging is also used to compare post-treatment results to the pretreatment predicted outcomes.
BENEFITS VS RISKS
The use of radiography in orthodontics should not be considered routine, as it is a modality that involves the use of ionizing radiation—a known carcinogen. For each patient, the potential benefits of the imaging series should be weighed against the risks. The known radiation risks of radiography and CBCT imaging, in particular, are described in part one of this series.1 Determining the potential benefits of a radiographic technique for an orthodontic patient involves consideration of these four sequential questions:
1. Will the radiograph complement or supplement the clinical findings? The initial decision to perform radiography is governed by the practitioner’s need to support a clinical diagnosis or provide additional information to confirm or improve a clinical impression. Justifying every radiographic exposure is never a matter of routine, and involves consideration of the following: patient’s initial physical presentation as determined by a thorough clinical examination; patient’s chief complaint; a comprehensive medical and dental history; an analysis of study models; review of previous radiographs; and identification of preliminary treatment goals based on a working diagnosis.
2. What specific imaging modality or series of radiographic examinations will provide diagnostically adequate, clinically useful information? Once the decision is made to use dental imaging, choosing the radiographic procedure that provides the necessary information with minimum patient radiographic exposure is next. This necessitates that practitioners understand the advantages, indications for, and limitations of specific radiographic procedures.
3. What are the best exposure settings for the chosen imaging procedure? After the most appropriate radiographic procedure has been decided, the right exposure parameters must be selected to provide an image of optimal diagnostic quality. Choosing the appropriate radiographic procedure, imaging modality, and optimal exposure factors to address a clinical problem are universal factors in all fields of radiology. By following this process, clinicians meet the principle of “as low as reasonably achievable,” or ALARA.
4. What does the image show? Finally, a systematic interpretation of the entire image, series, or volumetric dataset (in the case of CBCT) should be performed, and specific images generated and quantitative analysis, if necessary, made. Appropriate image formatting should be directed toward answering the specific clinical question that prompted the initial use of the radiographic procedure.
The introduction of CBCT technology in orthodontics does not invalidate the need for applying an “imaging necessity” analysis and appropriateness criteria to every patient. Because of the ease with which CBCT scans can be performed and the attraction of finding some potentially important diagnostic information, some advocate that current conventional imaging modalities (eg, panoramic and lateral cephalometric radiography) should be replaced by CBCT for standard orthodontic diagnosis and treatment.2–4 This is based on illustrative, but anecdotal, case reports without support of the current published evidence base. Nor does this position adequately address the risks involved—particularly those associated with radiation exposure.1 There is no doubt that CBCT provides greater clinician decision confidence in specific clinical orthodontic circumstances,5 as well as additional diagnostic information. There is a growing but limited body of evidence that demonstrates the information gained from CBCT imaging is more useful in treatment planning than data provided by conventional imaging in specific situations.5–9
THE ADVANTAGES OF CBCT IMAGING IN ORTHODONTICS
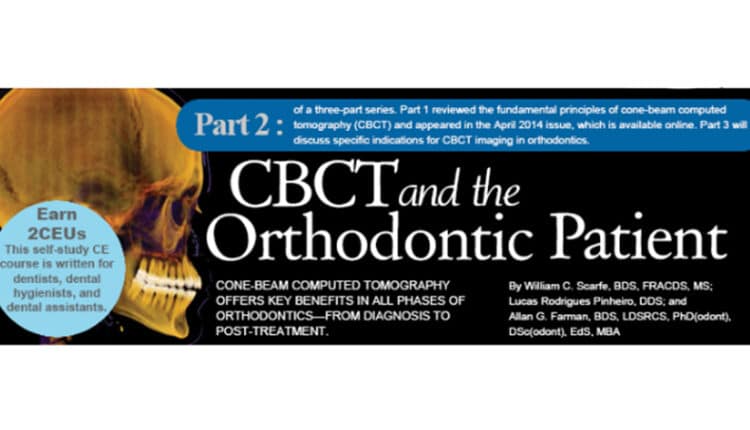
CBCT imaging provides many unique features and advantages to orthodontic practice over conventional extraoral imaging, such as panoramic and lateral cephalometric radiography. CBCT offers greater clinical imaging efficiency. Full field-of-view CBCT imaging provides volumetric data acquisition of the entire maxillofacial skeleton in a single radiographic procedure. These data can be easily reformatted to provide simulated radiographic (eg, lateral and posterior-anterior cephalometric, panoramic) or comparable volumetric images (Figure 1) currently used in orthodontic diagnosis, cephalometric analysis, and treatment planning. This provides for greater clinical imaging efficacy. In less complex cases, however, this level of imaging may not be necessary.10,11
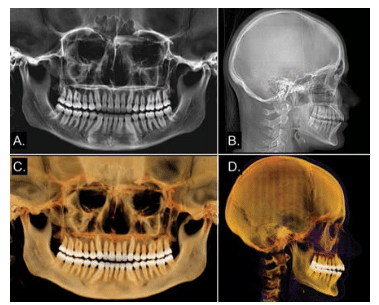
CBCT data can be reconstructed to provide unique, inter-relational, undistorted orthogonal (ie, axial, sagittal, and coronal) images previously unavailable for orthodontic assessment (Figure 2). Other imaging processing can also be performed, such as maximum intensity projection and surface or volumetric rendering, which provides an interactive volumetric model. Virtual maxillofacial models show the inter-relationship of craniofacial structures, including the maxillofacial skeleton and soft tissue boundaries, such as the airway and facial outline.
Unlike traditional extraoral and panoramic radiography, CBCT images are almost anatomically true (1:1 in size) representations from which slices can be displayed at any angle for all parts of the maxillofacial skeleton. Therefore, actual measurements can be obtained without the need for magnification or projection discrepancies.
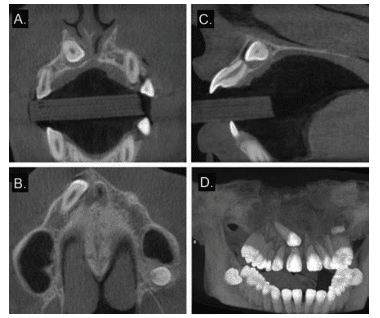
Orthodontics and orthopedics involve the maxillofacial skeleton, dentition, and soft-tissue integument, or the facial mask. CBCT data can be used as a platform onto which other inputs can be fused with acceptable clinical accuracy. These data sources include light-based surface data, such as photographic facial images (Figure 3), or high-resolution surface models of the dentition produced by direct scans intraorally or indirectly by scanning impressions or study models.12 The integration of hard and soft tissues can provide a greater understanding of the inter-relationship of the dentition and soft tissues to the underlying osseous frame and vice versa.
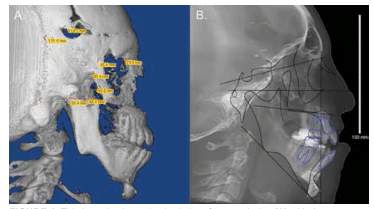
The digital imaging and communications in medicine, or DICOM, file format allows importation of CBCT data into third-party software that is capable of visualizing the dataset and volumetric 3D cephalometric analysis (Figure 4).13,14 The effects of therapy, particularly orthognathic surgery, can be reviewed by superimposing volumetric 3D images.15,16 Because of the time necessary to perform the analysis, high cost of software program, and limited evidence for the diagnostic efficacy of this approach, the application of 3D cephalometry is currently limited to the presurgical and post-operative analysis of patients with complex maxillofacial abnormalities.17
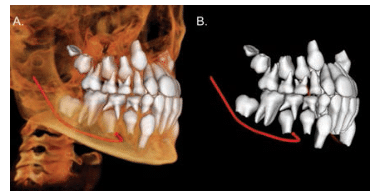
Most orthodontic software programs can be used to create virtual 3D models of the maxillofacial region for manipulation and visualization within the program (Figure 5). Three-dimensional surface models can also be created, from which dimensions can be calculated. In vitro investigations show that surface virtual models are very accurate for most CBCT units (98.9% of measurements being within 1 mm deviation and 92.8% within 0.5 mm),18 and comparable to optical scanning of dental impressions.19,20 However, the separation of bony or tooth structures from the volumetric dataset, which is referred to as segmentation, is a time-consuming technique, prone to artifacts, and may result in the clinical inaccuracy of 3D surface models—particularly in areas of thin bone, such as the condylar region and lingual cortex of the mandible.21,22
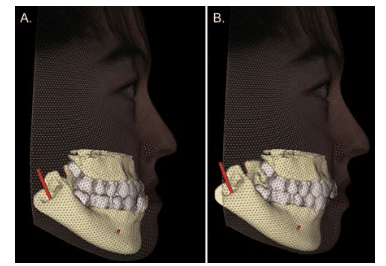
A virtual 3D visual treatment objective (VTO) is a predictive computer-assisted simulation that uses CBCT data to provide a pictorial digital 3D representation of the optimal post-therapy treatment result based on virtual repositioning of either dental and/or maxillofacial skeletal components (Figure 6). Establishing a VTO facilitates decision making on proposed treatment feasibility, optimizes case management, and increases the patient’s understanding and acceptance of the proposed treatment. The final location of these hard tissue elements is based on orthodontic and orthopedic principles. However, the soft tissue response to these movements, especially those involving the skeletal envelope or facial mask, is simulated by software based on preprogrammed hard-to-soft tissue ratios, which differ among available programs. Proprietary dental software programs for treatment simulations of both tooth-related and skeletal conditions for CBCT data are highly reliable.23,24
SUMMARY
CBCT is a valuable supplemental imaging modality to 2D radiography for the assessment and diagnosis of many specific conditions in orthodontic patients. While the advantages of CBCT are many, clinicians must weigh the risks vs benefits when determining whether CBCT is the best suited imaging modality for individual patient needs.
ACKNOWLEDGEMENT
Some of this information was provided with permission from the American College of Radiology (ACR) and taken from the ACR Appropriateness Criteria®. The ACR is not responsible for any deviations from the original ACR Appropriateness Criteria content.
References
- Scarfe WC, Pinheiro LR, Farman AG. Conebeam computed tomography. Dimensions of Dental Hygiene. 2014;12(4):60–64.
- Hechler SL. Cone-beam CT: applications in orthodontics. Dent Clin N Am. 2008;52:753–759.
- Mah JK, Huang JC, Choo H. Practical applications of cone-beam computed tomography in orthodontics. J Am Dent Assoc. 2010;141(Suppl 3):7S–13S.
- Larson BE. Cone-beam computed tomography is the imaging technique of choice for comprehensive orthodontic assessment. Am J Orthod Dentofacial Orthop. 2012;141:402–406.
- Alqerban A, Willems G, Bernaerts C, Vangastel J, Politis C, Jacobs R. Orthodontic treatment planning for impacted maxillary canines using conventional records versus 3D CBCT. Eur J Orthod. 2014 Jan 9. Epub ahead of print.
- Haney E, Gansky SA, Lee JS, et al. Comparative analysis of traditional radiographs and conebeam computed tomography volumetric images in the diagnosis and treatment planning of maxillary impacted canines. Am J Orthod Dentofacial Orthop. 2010;137:590–597.
- Botticelli S, Verna C, Cattaneo PM, Heidmann J, Melsen B. Two- versus three-dimensional imaging in subjects with unerupted maxillary canines. Eur J Orthod. 2011;33:344–349.
- Alqerban A, Hedesiu M, Baciut M, et al. Presurgical treatment planning of maxillary canine impactions using panoramic vs cone beam CT imaging. Dentomaxillofac Radiol. 2013;42:20130157.
- Hodges RJ, Atchison KA, White SC. Impact of cone-beam computed tomography on orthodontic diagnosis and treatment planning. Am J Orthod Dentofacial Orthop. 2013;143:665–674.
- Nijkamp P, Habets L, Aartman I, Zentner A. The influence of cephalometrics on orthodontic treatment planning. Eur J Orthod. 2008;30:630– 635.
- Devereux L, Moles D, Cunningham SJ, McKnight M. How important are lateral cephalometric radiographs in orthodontic treatment planning? Am J Orthod Dentofacial Orthop. 2011;139:175–181.
- Jayaratne YS, McGrath CP, Zwahlen RA. How accurate are the fusion of cone-beam CT and 3-D stereophotographic images? PLoS One. 2012;7:49585.
- Frongia G, Piancino MG, Bracco P. Conebeam computed tomography: accuracy of threedimensional cephalometry analysis and influence of patient scanning position. J Craniofac Surg. 2012;23:1038–1043.
- Schlicher W, Nielsen I, Huang JC, Maki K, Hatcher DC, Miller AJ. Consistency and precision of landmark identification in three-dimensional cone beam computed tomography scans. Eur J Orthod. 2012;34:263–275.
- Cevidanes LH, Alhadidi A, Paniagua B, et al. Three-dimensional quantification of mandibular asymmetry through cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:757–770.
- Cevidanes LH, Oliveira AE, Grauer D, Styner M, Proffit WR. Clinical application of 3D imaging for assessment of treatment outcomes. Semin Orthod. 2011;17:72–80.
- Pittayapat P, Limchaichana-Bolstad N, Willems G, Jacobs R. Three-dimensional cephalometric analysis in orthodontics: a systematic review. Orthod Craniofac Res. 2013 Dec 22. Epub ahead of print.
- Vandenberghe B, Luchsinger S, Hostens J, Dhoore E, Jacobs R, SEDENTEXCT Project Consortium. The influence of exposure parameters on jawbone model accuracy using cone beam CT and multislice CT. Dentomaxillofac Radiol. 2012;41:466–474.
- Kau CH, Littlefield J, Rainy N, Nguyen JT, Creed B. Evaluation of CBCT digital models and traditional models using the Little’s Index. Angle Orthod. 2010;80:435–439.
- White AJ, Fallis DW, Vandewalle KS. Analysis of intra-arch and interarch measurements from digital models with 2 impression materials and a modeling process based on cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;137:456–457.
- Fourie Z, Damstra J, Schepers RH, Gerrits PO, Ren Y. Segmentation process significantly influences the accuracy of 3D surface models derived from cone beam computed tomography. Eur J Radiol. 2012;81:524–530.
- Engelbrecht WP, Fourie Z, Damstra J, Gerrits PO, Ren Y. The influence of the segmentation process on 3D measurements from cone beam computed tomography-derived surface models. Clin Oral Investig. 2013;17:1919–1927.
- Tucker S, Cevidanes LHS, Styner M, et al. Comparison of actual surgical outcomes and 3-dimensional surgical simulations. J Oral Maxillofac Surg. 2010;68:2412–2421.
- Cevidanes LH, Tucker S, Styner M, et al. Three-dimensional surgical simulation. Am J Orthod Dentofacial Orthop. 2010;138:361–371.
From Dimensions of Dental Hygiene. August 2014;12(8):18–21.



