Alternative Injection Techniques
The use of the infraorbital, anterior middle superior alveolar, and maxillary nerve blocks provide safety and efficiency benefits during the administration of local anesthesia.
This course was published in the April 2016 issue and expires April 20, 2019. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the indications and contraindications of the infraorbital (IO), anterior middle superior alveolar (AMSA), and maxillary nerve blocks.
- Note the areas anesthetized by the IO, AMSA, and maxillary nerve blocks.
- Discuss the suggested technique for administering these alternative injections.
Local anesthesia is an area of clinical practice that should be continually evaluated to ensure safety and efficiency. While there are a multitude of avenues to improve the administration of local anesthesia—from buffering to the use of computer-controlled local anesthesia devices (CCLAD)—this article will focus on the use of alternative injection techniques to address both safety and efficiency.
When using traditional injection techniques to anesthetize a maxillary quadrant, up to five injections are required: posterior superior alveolar (PSA), middle superior alveolar (MSA), and anterior superior alveolar (ASA) nerve blocks and greater palatine (GP) and nasopalatine (NP) injections. This approach is time consuming and can cause patient discomfort. By utilizing the infraorbital (IO), anterior middle superior alveolar (AMSA), and maxillary nerve blocks, clinicians can reduce the amount of local anesthetic administered, decrease the time spent administering local anesthesia, and minimize the number of needle penetrations required for successful pain control.
As with all anterior anesthesia, a supplemental infiltration may be needed at the midline due to cross-innervation with these nerve blocks. Prior to administering an injection, the tissues should be dried and prepared with topical anesthetic. Because such injections numb areas of the face—including the upper lip, cheek, side of the nose, and lower eyelid—patients should be advised of this possibility prior to the administration of local anesthesia.
INFRAORBITAL NERVE BLOCK
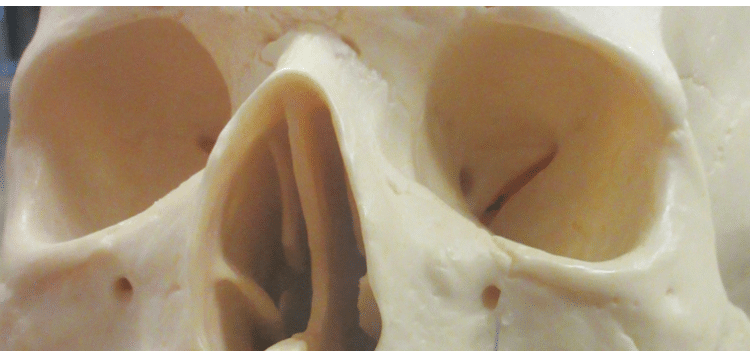
The IO nerve block is administered at the IO foramen (Figure 1) where the IO nerve exits the skull. This block anesthetizes both the ASA and MSA nerves with one injection, reducing the number of needle penetrations and the amount of anesthetic required to cover the area.1–3
Indications:
- Procedures involving multiple maxillary anterior or premolar teeth such as quadrant dentistry or periodontal therapy
- When infiltrations are contraindicated due to infection4 or the density of cortical bone;1 bone density is not usually a concern on the maxilla
Contraindications:
- Isolated areas of treatment (one tooth or two teeth only)
- When hemostasis is desired (the block is administered at the IO foramen; no hemostasis in the gingiva is observed)1
Areas anesthetized:
- Pulpal anesthesia to incisors and canines on the side anesthetized1
- In patients where the MSA nerve is present (approximately 72%), premolars and the mesiobuccal root on the first molar on the side anesthetized1
- Facial periosteum and soft tissues adjacent to these teeth
- Skin—including the upper lip, cheek, side of the nose, and lower eyelid on the side of injection

Identifying landmarks:
The target site for this injection is the IO foramen. To locate the IO foramen, the clinician should first palpate extraorally across the superior aspect of the infraorbital rim to locate the IO notch. It is usually found below the pupil when the patient is looking straight ahead (Figure 2). The IO foramen lies directly inferior to the IO notch on the inferior aspect of the infraorbital rim. During the injection, the clinician should place a finger on the IO notch as a guideline for the angle.
Technique:
A 25- or 27-gauge long needle is recommended for the IO nerve block.1 The penetration site is the height of the mucobuccal fold, adjacent to the maxillary first premolar. The barrel of the syringe should be positioned along a line following the long axis of the maxillary first premolar to the IO notch (Figure 3). The needle needs to be advanced slowly, aiming toward the guide finger and maintaining an angle parallel to the long axis of the maxillary first premolar until gently contacting the IO rim (approximately 16 mm in adults or1⁄2 of a long needle). It is important to advance the needle until bone is contacted, which may be less than 16 mm in some individuals. The needle should then be withdrawn 1 mm.
Aspiration in two planes is recommended. As such, the syringe can be rotated with a ¼ turn and re-aspirated if the first aspiration is negative. If both aspirations are negative, the anesthetic can be deposited. The anesthetic should be delivered slowly: 0.9 mL to 1.2 mL of anesthetic (1⁄2 to ¾ of a cartridge) at a rate of one cartridge per minute (30 seconds to 45 seconds). Pressure should be applied by the index finger positioned directly over the foramen and pushing gently toward the IO foramen for a minimum of 1 minute to 2 minutes to aid diffusion of the anesthetic solution into the IO foramen (Figure 4).

ANTERIOR MIDDLE SUPERIOR ALVEOLAR NERVE BLOCK
The AMSA nerve block is often used in esthetic dentistry. It anesthetizes the ASA, MSA, GP, and NP nerves with a single injection. Because this injection is delivered on the palate, the upper lip is not anesthetized. An unaltered smile-line is sometimes needed if the dentist needs to evaluate the margins of anterior crowns or veneers.
While the AMSA nerve block can be performed with a manual syringe, a CCLAD makes this injection easier to administer, more ergonomic for the practitioner, more comfortable for the patient, and exerts fewer side effects than traditional syringe delivery because the rate of administration and pressure associated with delivery remain constant. In addition, administering the AMSA nerve block with a CCLAD reduces the incidence of hand fatigue compared to a traditional syringe because of the recommended administration time (approximately 3 minutes).1,5–7
Indications:
- When anesthesia is needed for multiple areas of the maxilla1,2
- Esthetic dentistry procedures that require a smile-line evaluation1,2,7,8
- If infiltrations have been ineffective due to cortical bone density1
Contraindications:
- Patient is unable to tolerate a long injection time1,2
- Procedures in which more than 90 min-utes of anesthesia are necessary1
- If the palatal tissue is too thin;1 spongy sites better accommodate the necessary volume of solution (a cotton-tip applicator can be used to find a depressible site)9
Special considerations:
- Four percent anesthetic solutions such as articaine and prilocaine increase the risk of paresthesia; therefore, no more than 0.9 mL (1⁄2 cartridge) of these solutions should be administered9
- High concentrations of vasoconstrictors (1:50,000) can increase the risk of excessive blanching, possibly leading to tissue necrosis; these formulations should be avoided1,9
- Rapid deposition can lead to excessive blanching and patient discomfort; rate of deposition is 0.5 mL per minute (approximately ¼ cartridge per minute)1,9
Areas anesthetized:
- Pulpal anesthesia of central and lateral incisors, canine, and first and second premolars on the side of the injection
- Anterior and posterior palatal anesthesia on the side anesthetized to the midline
- Facial periosteum and soft tissues associated with these teeth

Technique:
A 27-gauge short needle is recommended for this injection. The penetration site for the AMSA is located on the hard palate between the apices of the first and second premolars, halfway between the midline and the gingival margin (Figure 5). Because this is a palatal injection, the use of a cotton-tip applicator to apply pressure adjacent to the penetration site may increase patient comfort.10 Pressure should be applied for a minimum of 30 seconds prior to the injection, and maintained during the injection until additional blanching from the anesthetic diffusion is observed.
The needle is typically held at a 45° angle to the palate with the bevel facing the bone. The tissue should be penetrated gently and the needle slowly advanced. Clinicians should administer a small amount of anesthetic as the needle is advanced, as well as rotate the needle during progression to the site of deposition to aid in patient comfort.1 The needle needs to be advanced until bone is gently contacted. If both aspirations are negative, proceed with depositing the anesthetic. A minimum of 0.9 mL to 1.2 mL (1⁄2 to ¾ cartridge) of anesthetic2 up to a full cartridge of 1.8 mL can be administered.1 Because palatal tissues are dense, the rate of deposition for the AMSA is slower than all other intraoral injections. The rate of administration is 0.5 mL per minute (approximately1⁄4 cartridge per minute).1,2 This will require an injection time of 120 seconds to 210 seconds total. Tissue blanching indicates that the anesthetic is being successfully delivered (Figure 6). If there is excessive blanching (loss of all pinkness in the tissues), the clinician should pause in administering anesthetic to allow blood flow to return to the tissues. Failure to do so can result in an ulcerated tissue lesion that is self-limiting and will resolve within 7 days to 14 days.7

MAXILLARY OR SECONDDIVISION NERVE BLOCK
The maxillary block anesthetizes the entire maxillary branch (often referred to as V2 or the second division) of the trigeminal nerve, which results in profound anesthesia of the entire maxillary quadrant.11 With the maxillary block, profound anesthesia is achieved for the entire quadrant in one injection for facial and lingual structures. This approach reduces the amount of anesthetic solution needed to only one cartridge (1.8 mL), increasing patient safety. There are two common intraoral approaches for this injection: the facial or high-tuberosity approach and the GP or palatal approach.
Only the high-tuberosity approach will be discussed here, as it is similar to the PSA nerve block and is typically easier to implement than the palatal approach. The primary disadvantage of the high-tuberosity approach is an increased risk of hematoma.12
The target area for this injection is the pterygopalatine fossa, which contains the pterygoid plexus of veins and the maxillary artery that supply much of the oral cavity and face. If the maxillary artery is nicked during administration, the resulting hematoma can be significant, although self-limiting.2
Indications:
- Quadrant dentistry or periodontal therapy
- When infection on the maxilla prevents the use of traditional maxillary injections13
- Patient fear of multiple injections
Contraindications:
- Increased risk of bleeding1
![]()
FIGURE 6. Tissue blanching indicates that the anesthetic is being successfully delivered. - Patients on anticoagulant therapy2
- Patients who bruise easily
- Uncooperative patients
- Infection in the area of injection
- Pediatric patients due to prolonged administration time and because children often have difficulty remaining still1
Special considerations:
- While the high-tuberosity approach is not difficult, clinicians need to strictly adhere to the guidelines because there are no bony landmarks to help determine the depth of penetration. Over-insertion is possible and because the deposition site is near a highly vascular area, multiple, repeated aspirations are indicated during this injection

Areas Anesthetized:
- Maxillary teeth to the midline (third molar to central incisor)
- Facial periosteum and soft tissues to the midline
- Bone and soft tissues of the hard palate to the midline
- Skin including the upper lip, cheek, side of the nose, and lower eyelid on the side of injection
Technique:
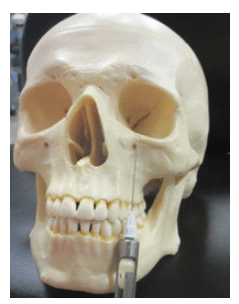
A 25-gauge long needle is recommended for this injection but a 27-gauge is acceptable.1 The penetration site for the maxillary block is the height of the mucobuccal fold distal to the maxillary second molar (the same penetration site used for the PSA nerve block). Prior to placing topical anesthetic, it is important to use a finger to feel along the facial aspect of the maxilla to find the zygomatic process, which is usually located above the first maxillary molar. It is important to insert distal to the zygomatic process or the maxillary bone may be scraped during administration. The angle of the syringe should be 45° from the mid-sagittal plane, as well as 45° apically from the maxillary occlusal plane. A helpful visual guide for this angle is a line running from the lateral periphery of the ala of the nose to the inside corner of the opposite eyebrow (Figure 7). The average depth of penetration for the maxillary block is 30 mm. With a 32 mm long needle, 2 mm of needle should remain visible outside the tissue (Figure 8). The bone should not be contacted on this injection, and the needle should progress smoothly through the tissues. The clinician should know the exact length of the needle, as different manufacturers produce different needle lengths. If both aspirations are negative, 1.8 mL (one cartridge) of anesthetic should be slowly deposited, re-aspirating every 1?4 of the cartridge to make sure a blood vessel has not been penetrated. The clinician should administer this injection slowly (taking more than 60 seconds to deliver the full amount) because of the highly vascular nature of the pterygopalatine fossa. Should the clinician inadvertently enter a blood vessel, slow administration will help distribute the anesthetic throughout the body, avoiding a large volume injection directly into the bloodstream.14

CONCLUSION
Each of these alternative injection techniques can reduce the total amount of local anesthetic administered, decrease the time spent on administration, and minimize the number of needle penetrations required for treatment. As with all injections, it is important to review the anatomical structures, indications, and contraindications prior to administration. The use of these injections may improve the experience of local anesthesia administration for both clinicians and patients.
References
- Malamed S. Handbook of Local Anesthesia. 6th ed. St. Louis: Elsevier Mosby; 2013.
- Bassett K, DiMarco A, Naughton D. Local Anesthesia for Dental Professionals. 2nd ed. Upper Saddle River, New Jersey: Pearson; 2015.
- Logothetis D. Local Anesthesia for the Dental Hygienist. St. Louis: Elsevier Mosby; 2012.
- Ogle OE, Mahjoubi G. Local anesthesia: agents, techniques, and complications. Dent Clin North Am. 2012;56:133–148.
- Fukayama H, Yoshikawa F, Kohase H, Umino M, Suzuki N. Efficacy of anterior and middle superior alveolar (AMSA) anesthesia using a new injection system: The wand. Quintessence Int. 2003;34:537–541.
- Nusstein J, Lee S, Reader A, Beck M, Weaver J. Injection pain and postinjection pain of the AMSA injection administered with the WAND or conventional syringe. Oral Surg Oral Med Oral Pathol Oral Radiol Endo. 2004;98:124–131.
- Friedman MJ1, Hochman MN. The AMSA injection: a new concept for local anesthesia of maxillary teeth using a computer-controlled injection system. Quintessence Int. 1998;29:297–303.
- Friedman MJ, Hochman MN. Using AMSA and P-ASA nerve blocks for esthetic restorative dentistry. Gen Dent. 2001;49:506–511.
- Bassett K, DiMarco AC. Effective use of the AMSA nerve block. Dimensions of Dental?Hygiene. 2010;8(7):30–34.
- Fehrenbach M, Herring S. Illustrated Anatomy of the Head and Neck. 4th ed. St. Louis: Elsevier; 2012:317.
- Poore TE, Carney MT. Maxillary nerve block: a useful technique. J Oral Surg. 1973;31:749–755.
- Hawkins JM, Isen D. Maxillary nerve block: The pterygopalitine canal approach. J Calif Dent Assoc. 1998;26:658–664.
- Mercuri LG. Intraoral second division nerve block. Oral Surg Oral Med Oral Pathol. 1979;47:109–113.
- Meyer FU. Complications of local dental anesthesia and anatomical causes. Ann Anat. 1999;181:105–106.
From Dimensions of Dental Hygiene. April 2016;14(04):42–44,47.




