 ANDREYPOPOV/ISTOCK/GETTY IMAGES PLUS
ANDREYPOPOV/ISTOCK/GETTY IMAGES PLUS
Using Silver Diamine Fluoride To Improve the Oral Health of Older Adults
Adult populations at increased caries risk can greatly benefit from SDF application.
This course was published in the April 2021 issue and expires April 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the impact of caries on global oral health.
- Explain the mechanism of action of silver diamine fluoride (SDF).
- Identify the risk factors for developing dental caries in older adult populations.
- Discuss SDF applications in older adults.
Globally, dental caries is the most preventable chronic disease—affecting 97% of the population—and an estimated 2.5 million people have untreated caries in their permanent teeth regardless of age, race, gender, or sex. Dental caries remains a public health concern for children and older adults, particularly among low-income populations. In the United States, 96% of older adults age 65 and older have untreated decay.1 Topical fluoride solutions, which provide a balance between protective and pathogenic factors, are the gold standard in preventing and/or arresting dental caries.1–6
Silver has been used in dentistry and medicine since the 1800s due to its outstanding anticaries, antimicrobial, and antirheumatic properties.7–9 A broad spectrum antimicrobial and antibacterial agent, silver also offers low toxicity. Blending silver and fluoride together in a solution stabilized by alkaline ammonia forms silver diamine fluoride (SDF). The dual action of SDF meets the criteria for a safe, effective, efficient, and equitable approach to caries treatment and intervention. The US Food and Drug Administration (FDA) approved 38% SDF as a Class II medical device for treating dental sensitivity with an off-label use for managing dental caries. SDF was also granted a breakthrough therapy status by the FDA.2,10–12
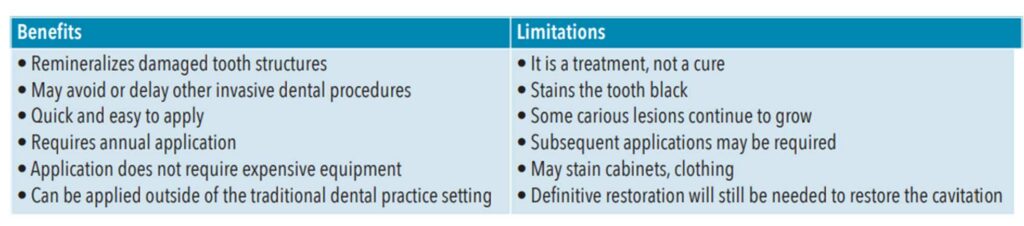
SDF is a promising medicament for arresting and preventing decay for older adults living in community-dwelling facilities and/or medically frail patients who cannot endure conventional dental treatments.4 Table 1 lists the benefits and limitations of SDF use in clinical practice.
MECHANISM OF ACTION
At concentrations of 20 parts per million (ppm), silver inhibits the growth of Streptococcus mutans and Actinomyces naeslundii, two of the most active bacteria in dental caries.1,8,13,14 The American Dental Association (ADA) Council on Scientific Affairs recommends high-concentration fluoride dentifrices, either self-applied or professionally applied, to assist with caries prevention.2 SDF (38%) contains 44,800 ppm and approximately 253,870 ppm silver.11,12 The combination of silver and fluoride inhibits the growth of bacterial pathogens, leading to the arrest and prevention of carious lesions.1,8,10,12,13–15 For older adults, a regimen that includes SDF may be a safe and minimally invasive option for preventing and arresting caries.
SDF has three microbial effects on the dental caries process:12,16
- Silver ions destroy the cell wall structure of the bacteria.
- Silver can hinder enzyme activities, which directly impacts the metabolic process.
- Silver inhibits the replication of bacterial DNA.
Additionally, the bactericidal agents in SDF have been shown to reduce the growth of cariogenic bacteria by interfering with the activity of matrix metalloproteinases and cystine cathepsins by preventing collagen degradation. Furthermore, SDF promotes the remineralization of hydroxyapatite, calcium, and phosphate ions in both enamel and dentin. This is achieved by reacting with hydroxyapatite in teeth to create silver phosphate ions and calcium, forming an insoluble layer of fluorapatite.16 SDF hardens the enamel, which reduces the damage caused by daily dietary and pharmaceutical challenges common in older adults.
PREVALENCE OF CARIES IN OLDER ADULTS
The older adult population (age 65 and older) in the US accounts for more than 13% of the total population, and is at high risk for chronic disease and disability, including dental caries. Oral health professionals must be prepared to provide services to the increasing number of medically compromised and cognitively impaired older adults. Early detection and interventions, such as fluoride treatments, can assist in reducing caries risk among this population.17,18 Due to the multifactorial challenges of aging, the overall incidence of root caries increases, especially untreated root caries, among older adults.5,19 Root caries increases exponentially when mobility challenges are compounded with poor nutrition. Geriatric diets often lack fresh fruit and vegetables and are frequently concentrated in processed carbohydrates and sugars. The US Centers for Disease Control and Prevention reports that nearly all adults age 65 and older have caries experience (96%), and one in five (20%) have current, untreated tooth decay. Additionally, two out of three adults (68%) have periodontal diseases, which may increase the incidence of recession and root caries.20,21 While root caries can be treated with meticulous toothbrushing and fluoride toothpaste, current research suggests that SDF may be more effective at arresting or preventing root caries among older adults.5,19,22,23
The rate of edentulism has declined by as much as 50% since the 1950s, as most older adults retain some or all of their natural teeth. With more natural dentition, older adults are at increased risk for dental caries due to age-related salivary changes, poor diet, and exposure of root surfaces through gingival recession.24 A large portion of dental decay in older adults is from reoccurring decay associated with failing restorations frequently found along the gingival margin.11 Poor oral health occurs more often among older adults due to the loss of dental insurance and low incomes.25,26 A major benefit of SDF is its cost-effectiveness and minimally invasive properties, which may be ideal for treating dental caries in the aging population.
SILVER DIAMINE TREATMENTS
Untreated caries negatively affects the quality of life for older adults, and affordable and effective treatment modalities are needed to manage untreated caries on root surfaces.27 Three Hong Kong-based research studies found that a 38% solution of SDF was effective in preventing new root caries among community dwelling older adults.19,22,23 The studies compared SDF with sodium fluoride (NaF) varnish or chlorhexidine (CHX) varnish. SDF demonstrated similar benefits as NaF and CHX; however, unlike NaF and CHX which require biannual or quarterly applications, SDF is effective with only annual application. The researchers concluded that SDF could be used for older adults who present with increased prevalence of root caries alone or in conjunction with oral hygiene education to reduce further progression. Two of the studies found the use of SDF decreased the initiation of root caries.19,22
SDF is safe, simple, and effective in preventing and arresting root caries. As a large portion of older adults reside in long-term care facilities with minimum access to oral healthcare, SDF may be an economical and efficient method for arresting and preventing decay. Application of SDF is a simple procedure and requires no expensive equipment or infrastructure support.12 The ease of use combined with annual application allows SDF to be used in limited-access settings such as long-term care facilities and nursing homes where mobility issues often prevent patients from receiving timely dental treatments. When applied annually, it can be an effective means for preventing and slowing the progression of carious lesions without adding additional stresses required when traveling to a dental facility for treatment. Table 2 lists the clinical applications of SDF.

APPLICATION OF SILVER DIAMINE FLUORIDE
Applying SDF to a cavitated lesion is a quick and simple process. While it is not necessary to excavate prior to application, gross debris should be removed to allow the SDF to come into direct contact with the lesion. Prepare the patient by placing a thin layer of petroleum jelly to the lips to prevent discoloration.28 Isolate the working area with cotton rolls and dry the area where the SDF will be applied. A small microbrush provides more control when applying SDF to prevent inadvertently staining adjacent teeth. When using a single use ampule of SDF, dip the microbrush into the ampule. If applying with a multi-use package, dispense a single drop of SDF into a dappen dish. Begin by dipping the microbrush into the SDF and then carefully squeeze the excess SDF out of the tip by pressing the tip of the microbrush against the side of the dappen dish. Apply the SDF directly to the cavitated lesion using the microbrush. With a clean cotton roll or rolled gauze, remove the excess SDF to limit possible systemic absorption. For older adults, application time should be 1 minute, however, young children need shorter application times. For best results, keep the area isolated for 3 minutes.28 Lightly dry the area with air and apply sodium fluoride varnish. Monitor the areas post-operatively at each recare visit and reapply as necessary.
SIDE EFFECTS AND CONTRAINDICATIONS
SDF’s most significant side effect is staining. A dark brown or black stain occurs when the silver ions encounter a carious lesion.17,22 Patients must be informed of this effect. Some have suggested the application of potassium iodide following SDF may be helpful, but research does not show this method reduces the stain. Composite materials may be placed over arrested lesions, improving esthetics.17,22 Temporary staining of the skin is also possible. Oral health professionals must take extra precautions when handling and applying SDF because it will stain operatory surfaces.29
Patients may also experience a metallic taste post-application and irritation around the gingival margin, but these side effects last for only a few days.29,30 Oral health professionals should explain the risks vs benefits to patients so they can make informed decisions.
While an allergy to silver is the only known contraindication SDF, other factors need to be considered.31 Teeth with evidence of pulpitis or pupal necrosis should not be treated with SDF. Likewise, pupal irritation or reactions may occur if SDF is used to treat teeth with deep carious lesions that extend into the dentin. This is due to the presence of ammonia and the high pH of SDF.31
CONCLUSION
The addition of ammonia into mixtures of silver and fluoride create an alkaline solution chemically known as SDF. While it is well-known that the biannual application of fluoride supports caries prevention, SDF applications may be more beneficial among older adults. SDF’s silver and fluoride ions can destroy cariogenic bacteria in dental plaque. Current epidemiological research suggests an aging population with complex medical histories including polypharmacy, advance treatment modalities for diseases, and a decrease in edentulism, results in an increase in carious lesions. Additionally, as the population ages, gingival recession may occur, placing older adult patients at increased risk for root caries. This risk may increase among patients who reside in community living facilities with minimal or no access to care, limited financial resources, and an inability to express dental needs.
Living with untreated dental caries can impact the health and well-being of older adults. Medical and oral health professionals should consider the use of SDF for treatment and prevention of root surface caries, especially limitations to conventional care exist.
REFERENCES
- Yellowitz J, Schneiderman M. Elder’s oral health crisis. J Evid Base Dent Pract. 2014;145:191–200.
- Slayton RL, Urquhart O, Araujo MWB, et al. Evidence-based clinical practice guideline on nonrestorative treatments for carious lesions. J Am Dent Assoc. 2018;149:837–849.
- Berg, J. The marketplace for new caries management products: dental caries detection and caries management by risk assessment. BMC Oral Health. 2006;6:56.
- Kassebaum N, Bernabe E, Dahiya M, Bhadari B, Murray C, Marcenes W. Global burden of untreated caries: a systematic review and meta-regression. J Dent Res. 2015;94:650–658.
- Griffin S, Jones J, Brunson D, Griffin P, Biley W. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health. 2012;102:411–418.
- Weyant R, Tracy S, Anselmo T. Topical fluoride for caries prevention: executive summary of the updated clinical recommendations and supporting systematic review. J Am Dent Assoc. 2014;13:1279–1291.
- Peng J, Botelho M, Matinlinna J. Silver compounds used in dentistry for caries management: a review. J Dent. 2012;40:531–541.
- Sarvas E. The history and use of silver diamine fluoride in dentistry: a review. J Calif Dent Assoc. 2018;46:19–22.
- Lansdown A. Silver in healthcare: antimicrobial effects and safety in use. Curr Probl Dermatol. 2006:33:17–34.
- Mei M, Li O, Chu C, You C, Lo E. The inhibitory effects of silver diamine fluoride on dentine remineralization and collagen degradation. J Dent. 2013;41:809–817.
- Horst J, Ellenikiotis H, Milgrom P. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications, and consent. J Calif Dent Assoc. 2016;44:16–28.
- Rosenblatt A, Stamford TCM, Niederman R. Silver diamine fluoride: a caries “silver-fluoride bullet.” J Dent Res. 2009;88:116–125.
- Stebbins E. What value has argenti nitras as a therapeutic agent in dentistry? Int Dent J. 1891;12:661–670.
- Thibodeau E, Handleman S, Marouis R. Inhibition and killing of oral bacteria by silver ions generated with low intensity direct cuttent. J Dent Res. 1978;57:922–926.
- Russell A, Hugo W. Antimicrobiological activity and action of silver. Prog Med Chem. 1994;31:351–370.
- Margolis J, Moreno E. Composition and cariogenic potential of dental plaque fluid. Crit Rev Oral Bio Med. 1994;5:1–25.
- Griffin S, Griffin P, Swann J, Zlobin N. Estimating rates of new root caries in older adults. J Dent Res. 2004;83:634–638.
- United States Administration on Aging. 2019 Profile of Older Americans. Available at: acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2019ProfileOlderAmericans508.pdf. Accessed March 12, 2021.
- Tan H, Lo E, Dyson J, Luo Y, Corbet E. A randomized trial on root caries prevention in elders. J Dent Res. 2010;89:1086–1090.
- Elani H, Harper S, Allison P, Bedos C, Kaufman J. Socioeconomic inequalities and oral health in Canada and the United States. J Dent Res. 2012;91:865–870.
- United States Centers for Disease Control and Prevention. Oral Adult Oral Health. Available at: cdc.gov/oralhealth/basics/adult-oral-health/adult_older.htm. Accessed March 12, 2021.
- Zhang W, McGrath C, Lo E, Li J. Silver diamine fluoride and education to prevent and arrest root caries among community-dwelling elders. Caries Res. 2013;47:284–290.
- Li R, Lo ECM, Liu BY, Wong MCM, Chu CH. Randomized clincal trial on arresting dental root carieTs through silver diamine fluoride applications in community-dwelling elders. J Dent. 2016;51:15–20.
- Wyatt C, Want S, Aleksejuniene J. Incidence of dental caries among susceptible community dwelling older adults using fluoride toothpaste: 2-year follow-up study. J Can Dent Assoc. 2014;80:1–7.
- Colby SL, Ortman JM. Projections of the size and composition of the US population: 2014 to 2060. Population Estimates and Projections. Current Population Reports. P25-1143. Available at: eric.ed.gov/?id=ED578934#:~:text=Colby%2C%20Sandra%20L.%3B%20Ortman%2C%20Jennifer%20M.&text=Between%202014%20and%202060%2C%20the,reaching%20400%20million%20in%202051. Accessed March 12, 2021.
- Nyvad B, Fejerskov O. Active root surface caries converted into active caries as a response to oral hygiene. Scand J Dent Res. 1986;94:281–284.
- Oliveria B, Cunha-Cruz J, Rajendra A, Niederman R. Controlling caries in exposed root surfaces with silver diamine fluoride. J Am Dent Assoc. 2018;148:671–678.
- Ellenikiotis H. Silver diamine fluoride: a practitioner’s perspective. What you need to know, what your patient want to know. Available at: elevateoralcare.com/site/images/ Silverbulletins/EleniCuttingEdge.pdf. Accessed March 12, 2021.
- Mikhail C, Williams JC. Reducing caries risk with topical fluoride. Dimensions of Dental Hygiene. 2020;18(6):22–23.
- Fung M, Wong M, Lo E, Chu C. Arresting early childhood caries with silver diamine fluoride-a literature review. J Oral Hyg Health. 2013;1:117.
- Mei M, Lo E, Chu C. Clinical use of silver diamine fluoride in dental treatment. Compend Contin Educ Dent. 2016;37:93–98.
From Dimensions of Dental Hygiene. April 2021;19(4):32–35.



