
A Tunneling Treatment Approach to Gingival Recession
A twofold tunneling technique can yield predictable outcomes when treating multiple recession defects.
This course was published in the December 2021 issue and expires December 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the role of platelet-rich fibrin (PRF) in guided tissue regeneration.
- Describe the technique of tunneling using acellular dermal matrix and PRF membrane for multiple gingival recessions.
- Discuss the role of the dental hygienist in treating patients with gingival recession.
A smile is worth a thousand words, as the saying goes. However, an unesthetic smile due to anterior gingival recession becomes magnified when multiple teeth are involved. As treatment of gingival recession is a precise art, practitioners who choose to treat sites of gingival recession are advised to keep abreast of advances in mucogingival surgery. The subepithelial connective tissue graft introduced by Langer and Langer1 is considered the gold standard for root coverage procedures. Raetzke2 proposed the envelope technique, which eliminated the need for vertical incisions, while Zabalegui et al3 introduced a combination technique in which a mucosal partial-thickness tunnel encompassing multiple teeth is reflected to place the subepithelial connective tissue graft.
More recently, the use of acellular dermal matrix for root coverage procedures has become an alternative to the subepithelial connective tissue graft. Harris and Harris4 reported 99% root coverage using both a subepithelial connective tissue graft via a partial-thickness, double-pedicle graft and acellular dermal matrix via a coronally advanced flap. Modaressi and Wang5 suggested the use of acellular dermal matrix via tunneling as a promising alternative to the gold standard technique in treating multiple gingival recession defects in the esthetic zone.
Platelet-Rich Fibrin
Platelet-rich fibrin (PRF) is a platelet-rich concentrate from autologous blood that is compressed into a membrane form to be used in periodontal surgeries. This membrane releases growth factors, including PDGF, TGF-β1, VEGF, EGF, FGF, and IGF, and its use has shown to eliminate potential disease transmission and immunogenic reactions due to its autologous nature.6,7

The physical properties of PRF enable it to be used as a biologic scaffold for guided tissue regeneration in bony defects around teeth affected by periodontal destruction. In fact, PRF is preferred over platelet-rich plasma because the fibrin membrane has been shown to more slowly release growth factors and cytokines during wound healing.8 Additionally, a recent report has identified a role for platelet-rich concentrates from autologous blood, along with acellular dermal matrix, to achieve root coverage in sites of gingival recession.9
Clinical Presentation
A 31-year-old woman presented to the Department of Periodontology clinic at the Indiana University School of Dentistry with a chief complaint of an unesthetic smile due to exposed root surfaces in the upper and lower arch extending from premolar to premolar (Figure 1). The patient reported a dental history of orthodontic correction of misaligned teeth, with a noncontributory medical history. The patient had an initial plaque score of 9%, with a clinically noninflamed gingival appearance. She reported brushing twice a day with a soft-bristled toothbrush and used a more than required pressure when asked to demonstrate.

On clinical examination, teeth #5, 6, 9, 10, 11, and 12, and 20 to 29 presented with type 1 (Miller’s Class I and Class II) gingival recession.10 Class V restorations were noted on teeth #5, 6, 11, and 12, which also denote a history of aggressive brushing. Periodontal diagnosis (per the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions) was clinical gingival health on a reduced periodontium in a nonperiodontitis patient.
The patient’s expectations were for root coverage, and she expressed interest in alternate techniques to soft tissue harvesting from the palate. The treatment option presented was root coverage with acellular dermal matrix and PRF membranes, using a tunneling approach to achieve adequate root coverage from teeth #5, 6, 9, 10, 11, and 12, and 20 to 29, with improved soft tissue healing. The maxillary arch was chosen to be treated prior to the mandibular arch, as the patient was more concerned about the maxillary arch for esthetic reasons.
Case Management
Phase I therapy included dental prophylaxis and patient education in oral hygiene practices, such as proper brushing technique and frequency. Prior to surgery, preoperative instructions were provided and the procedure was explained. Written consent was obtained for the surgery. Next, venous blood (40 ml) was collected from the patient’s right median cubital vein and centrifuged at 1,200 rpm for 12 minutes. The collected fibrin clots were compressed to form four leukocyte-PRF membranes (Figure 2).

Following the achievement of adequate anesthesia using 2% lidocaine with 1:100,000 epinephrine, thorough root surface instrumentation was performed using site-specific Gracey curets from teeth #4 to 13, followed by the application of 17% ethylenediaminetetraacetic acid for 2 minutes for root conditioning to eliminate the smear layer. The recipient site was prepared with a tunneling approach (Figure 3A through Figure 3C).

The graft was serially hydrated in saline, and then in a solution of saline with tetracycline for 10 minutes each. The graft was inserted and passed through the tunnel, followed by the insertion of the PRF membranes over the acellular dermal matrix (Figure 4 and Figure 5). A 1.5×1-mm perforation was evident apical to tooth #8 following flap elevation.

Continuous sling sutures using 6-0 polypropylene were performed for graft and tissue stabilization (Figure 6).
Verbal and written post-surgical instructions were provided. Recare appointments were scheduled at 1, 2, and 3 weeks post-operatively, and sutures were removed at the third post-operative week. The patient was counseled again regarding proper toothbrushing techniques (modified Bass technique) and oral hygiene maintenance during Phase I therapy, and these instructions were reiterated post-operatively at every follow-up appointment to prevent any future recession. The patient was also advised to keep up with regular prophylaxis appointments to maintain periodontal health.

Clinical Outcomes
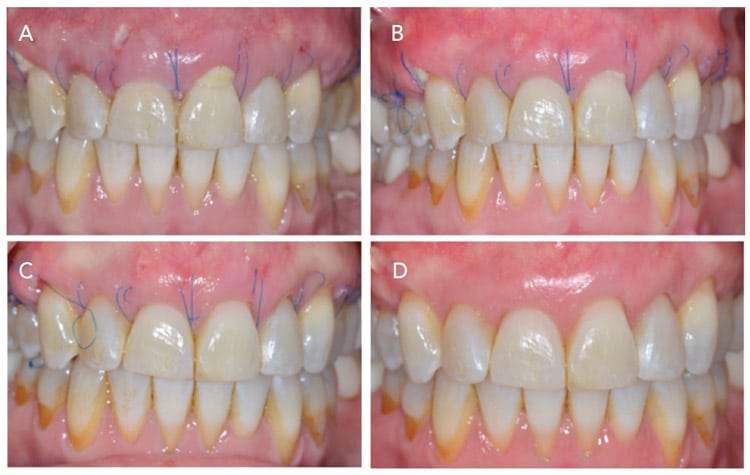
Soft tissue healing was uneventful and appeared to be enhanced from week 1 (Figure 7A through Figure 7D). The facial surface of teeth #9 and 6 had graft membrane exposure at the 1-week and 2-week pos-operative appointments. At the 3-week appointment, the gingival margin was slightly apical to the cementoenamel junction at tooth #9, and hence 1 mm of recession was noted in this area at the 3-month post-operative appointment. At the 2-week and 3-week appointments, slight apical migration of the gingival margin at teeth #5, 6, 11, and 12 that had Class V composite restorations were noted.
However, clinical results show more than 90% root coverage on teeth #7, 8 , 9, and 10 at the 3-week post-operative appointment, which was stable at the 3-month post-operative visit. Teeth #5, 6, 11, and 12 with Class V composite restorations presented with the gingival margin levels at or apical to their corresponding restorative margins (Figure 7D).
Discussion
The purpose of the presented case is to demonstrate the treatment protocol and evaluate the healing outcome of tunneling using acellular dermal matrix and PRF membrane for multiple gingival recessions. This technique is proposed for the surgical treatment of multiple gingival recession defects when an allogenic graft is preferred and an enhanced healing outcome is desired.
This case report indicates that tunneling using acellular dermal matrix and PRF membrane can be used as an alternative method to cover multiple recession-type defects. In addition, it offers an enhanced healing rate. The case presented involves the treatment of multiple teeth, and it was advisable to use acellular dermal matrix in place of an autogenous graft, thus bypassing the anatomical limitation of the patient’s palate. The uniform dimension of the graft material contributes to the clinician’s ergonomic advantage with the tunneling technique.
The acellular dermal matrix used in this procedure provided stability and ease of handling. Due to the large span of the area that was treated, it also allowed the patient to heal without possible donor site complications. As noted, PRF is a reservoir of growth factors and cytokines that demonstrates enhanced healing capabilities when used in periodontally affected sites. The membrane form of this platelet concentrate has proven substantivity for growth factor release, along with the physical advantage that enables it to be used as a biologic scaffold in hard and soft tissue regeneration. The materials used in this case report showed clinically enhanced healing capabilities, as well as reduced pos-operative morbidities.
Removal of Class V restorations prior to grafting was not considered due to the availability of argumentative literature that both supports and refutes the need for it. However, on retrospective evaluation of the clinical results, removal of Class V restorations prior to grafting might have increased the percentage of root coverage in the restored sites.
The mandibular arch was treated with the same approach. The procedure was performed before the clinics were closed due to the COVID-19 pandemic. While limited follow-up appointments were scheduled, limitations in clinic time due to the pandemic precluded additional photographic documentation.
The Dental Hygienist’s Perspective
As patients often present to the dental practice seeking treatment options for gingival recession, dental hygienists play an important role in facilitating this discussion. Dental hygienists can help guide patients appropriately after discussions with the dental practitioner.
Points to consider include:
- Etiology. The dental hygienist is well-suited to help patients understand why gingival recession occurs. The discussion may include, the influence of tooth anatomy and position, oral hygiene habits, -acute/chronic trauma, position of frenum attachment, occlusal trauma, and orthodontic treatment, among other clinical conditions.
- Dentinal hypersensitivity. Dental hygienists know that hypersensitive teeth are common among individuals with generalized recession. Oral health professionals should be prepared to recommend at-home or professionally applied agents to manage dentinal hypersensitivity as they are cost-effective, safe, and convenient.
- Local anesthesia. Patients with gingival recession may experience extreme sensitivity to exploring, probing, and scaling. It is likely that these patients will require anesthesia, either local or topical to facilitate treatment
- Caries risk. Patients with exposed roots often are at increased risk of root caries formation. Discussion on prevention should be initiated.
- Esthetics. One of the reasons why patients seek care for the correction of gingival recession in the maxillary anterior region of the mouth is because of esthetics. Dental hygienists should be informed about treatment options so they can help facilitate care.
- Referral to a periodontist. Once the patient-dentist discussion has occurred, referral to a specialist who routinely treats gingival recession, such as a periodontist, should be considered.
- Post-surgical treatment. Communication between the periodontist and the dental hygienist for continuing care should be established. Discussion may include: appropriate oral hygiene instructions, using an extra soft brush in the post-operative phase of treatment utilizing the modified Bass technique, and the importance of preventing any etiologic habits that may have contributed to the recession.
Summary
This case report presents a novel approach for the treatment of multiple gingival recessions in which a combination of autologous and allogenic materials is used. The purpose of the material selection was for root coverage, as well as for enhanced soft tissue healing. Adequate soft tissue reflection for encompassing the bulk of the acellular dermal matrix and PRF materials is an important determinant in the success of the treatment outcome. Some of the primary limitations include inadequate periosteal elevation, preoperative keratinized tissue deficiency, proper stabilization of the graft materials, and achieving primary closure.
References
- Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56:715–720.
- Raetzke PB. Covering localized areas of root exposure employing the “envelope” technique. J Periodontol. 1985;56:397–402.
- Zabalegui I, Sicilia A, Cambra J, Gil J, Sanz M. Treatment of multiple adjacent gingival recessions with the tunnel subepithelial connective tissue graft: a clinical report. Int J Periodontics Restorative Dent. 1999;19:199–206.
- Harris RJ, Harris AW. The coronally positioned pedicle graft with inlaid margins: a predictable method of obtaining root coverage of shallow defects. Int J Periodontics Restorative Dent. 1994;14:228–241.
- Modarressi M, Wang HL. Tunneling procedure for root coverage using acellular dermal matrix: a case series. Int J Periodontics Restorative Dent. 2009;29:395–403.
- Choukroun J, Diss, A, Simpmpieri A, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part V: histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:299–303.
- Thorat M, Pradeep AR, Pallavi B. Clinical effect of autologous platelet‐rich fibrin in the treatment of intra‐bony defects: a controlled clinical trial. J Clin Periodontol. 2011;38:925–932.
- Kobayashi E, Flückiger L, Fujioka-Kobayashi M, et al. Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin Oral Investig. 2016;20:2353–2360.
- Pratiwi R, Setiawatie EM. Multiple gingival recession coverage treated with vista technique using acellular dermal matrix (ADM) Combined with platelet rich fibrin (PRF): a case report. Odonto Dent J. 2019;6:56–61.
- Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: an explorative and reliability study. J Clin Periodontol. 2011;38:661–666.
From Dimensions of Dental Hygiene. December 2021;19(12)40-43.



