
The Meaning of Tooth Migration
While the presence of space between teeth is common among children, pathologic tooth migration in adults may be indicative of oral disease.
This course was published in the July 2015 issue and expires July 31, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the concept of pathologic tooth migration.
- Identify the factors involved in tooth migration.
- Explain the treatment options for migrating teeth.
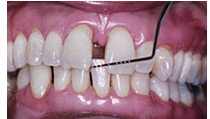
Diastemata are a normal sequela of jaw growth and development. The most common diastemata occur between the maxillary central incisors. The prevalence of diastemata in young children is very high, ranging from 43% to 97%.1–3 The prevalence decreases by the time children reach age 11 and is gradually eliminated by age 15 in most children. Diastemata result from discrepancies between the growth of the jaws and the sizes of the erupted teeth. The transition from the primary to the permanent dentition is characterized by an enlargement of the jaws with the creation of additional space to accommodate permanent teeth that differ significantly in size and number from the deciduous dentition. Thus, diastemata between the maxillary central incisors is commonplace during the mixed dentition years. In most cases, such diastemata resolve following eruption of the permanent maxillary lateral incisors and canines (Figure 1 to Figure 3).4
In some individuals, however, diastemata may persist into adulthood.5 Etiologies are typically multifactorial but commonly reflect discrepancies between the sizes of the teeth and dimensions of the jaw. The causes for such discrepancies are usually genetic. Other contributing etiologies may include the presence of an enlarged aberrant frenal attachment or pernicious oral habits—such as lower lip biting and finger sucking. These may cause the maxillary incisors to flare facially, leading to a midline diastema.6,7 Also, a tongue thrust or too-large tongue (macroglossia) may also disrupt the delicate muscular balance, thereby flaring the incisors as the teeth tip or migrate to a new equilibrium position. Other etiologies, such as a peg laterals, unerupted mesiodens, retained primary incisors, congenitally missing lateral incisors, and naso-palatine cysts, may play a role in midline spacing.8
 FIGURE 1. Primary dentition of a 5-year-old boy
FIGURE 1. Primary dentition of a 5-year-old boy
 FIGURE 2. A midline diastema formation on the same boy from Figure 1 following the eruption of his permanent central incisors at age 7
FIGURE 2. A midline diastema formation on the same boy from Figure 1 following the eruption of his permanent central incisors at age 7
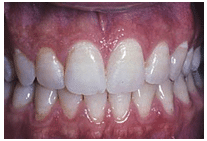 FIGURE 3. Closure of the diastema seen in Figure 2 following eruption of the canines at age 12
FIGURE 3. Closure of the diastema seen in Figure 2 following eruption of the canines at age 12
If these etiologic factors are not properly addressed during the mixed dentition phase, the spaces may become permanent. The acceptance of the maxillary midline diastema varies greatly among individuals. Some consider the presence of one or more diastemata to be unesthetic. These patients may seek closure of these spaces through orthodontic or prosthodontic means (Figure 4 and Figure 5). Other patients, however, find a midline diastemata attractive. Therefore, oral health professionals should ask patients with diastemata to determine their esthetic preferences in the context of the functional health status of the dentition and periodontium.

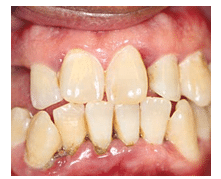
FIGURE 4. Moderate periodontitis and pathologic tooth migration in a 51-year-old woman
 FIGURE 5. Closure of the diastema seen in Figure 4 following periodontal and prosthodontic therapy
FIGURE 5. Closure of the diastema seen in Figure 4 following periodontal and prosthodontic therapy
ADULT DIASTEMATA FORMATION
An acquired diastema may be a warning sign signaling the presence of advanced periodontitis. Gingival inflammation, reduced bony support, and tooth mobility may contribute to the drifting of teeth—a condition called pathologic tooth migration.9 This typically affects the anterior teeth and can manifest in various forms. The most common form is facial flaring of incisors, followed by rotation, extrusion, mesial or distal tipping, or a combination of these changes.10 Studies of patient populations with moderate and severe periodontitis indicate that pathologic migration is a common finding, with a prevalence ranging from 30.03% to 55.8%.10,11 Tooth migration can be disfiguring, and it often is a major motivating factor for patients to seek dental care.12
CAUSES OF PATHOLOGIC TOOTH MIGRATION
While much of the dental literature centers on the potential role of traumatic occlusal forces in the etiology and progression of periodontitis, little has been written regarding the impact of periodontitis on dental alignment and occlusion. Weinstein et al13 suggest that a tooth’s position in the dental arch is controlled by intra- and extraoral musculatures forces; the presence, absence, and position of adjacent teeth; and the quality of the tooth’s attachment apparatus. Functional and parafunctional forces exerted on the clinical crowns are transmitted to the periodontium. Equilibrium is a state of rest in which the position of the tooth is a reflection of all the forces acting upon it. According to Weinstein et al, every tooth is in equilibrium with its surroundings, which include the adjacent teeth, tongue, perioral musculature, magnitude and frequency of occlusal forces, parafunctional forces, and health status of the periodontium. When the forces acting against the crown are self-negating, the tooth is at equilibrium position. A stable occlusion is more likely if the periodontium is healthy. Indeed, periodontitis, with its attendant bone loss, may disrupt the delicate balance of forces, thereby resulting in pathologic tooth migration (Figure 6) as the tooth seeks a position of maximal equilibrium. If positional equilibrium cannot be achieved, a tooth will remain chronically mobile.
Another explanation for tooth migration is the chronic inflammatory process first proposed by Hirschfield14 in 1933. He suggested the inflamed gingiva had a higher interstitial fluid pressure due to an increase in blood flow and vascular permeability.15 According to Hirschfield, gingival inflammation and edema may increase the pressure inside the periodontal pocket, which is then transmitted to the periodontal ligament. This theory is supported, in part, by the clinical observation of a tooth tending to migrate away from its deepest pocket. This is demonstrated in Figure 7 and Figure 8, in which tooth #9 presented with a distal infrabony defect and formation of diastema on its distal.
Plaque-associated gingival overgrowth and severe inflammation or drug-induced enlargements due to phenytoin, cyclosporin A, and calcium channel blockers have also been implicated in tooth displacement and acquired diastemata formation.16 Posterior bite collapse, occlusal interferences, and bruxism17 also are possible etiologic factors for tooth migration. Additionally, various oral habits, such as lip and tongue habits, fingernail biting, thumb sucking, and playing wind instruments have been associated with pathologic tooth migration.18
TREATMENT OPTIONS
Identification of the causative factors involved in pathologic tooth migration is crucial for a successful treatment outcome. In early cases, a spontaneous correction of the tooth position has been described in several case reports following nonsurgical19,20 and surgical periodontal procedures.21–24 These cases indicate that migrated teeth sometimes return to their original positions after the etiologic factor has been eliminated (eg, gingival inflammation, occlusal interferences, or drug-induced gingival overgrowth). The return of teeth to their original positions, however, is unpredictable and depends on multiple factors. Gaumet et al25 reported the outcome of patients with acquired anterior diastemata who underwent nonsurgical and surgical periodontal interventions. They reported a complete closure of diastemata in 51.5% of patients while the remaining subjects exhibited various degrees of repositioning. The preoperative dimension of the diastema dictated the likelihood of its closure. Best results were noted in patients with a preoperative diastema of ? 1 mm in dimension. Rohatgi et al26 reported similar results following periodontal treatment where 32.3% of sites showed complete repositioning. They reported an inverse relationship between the severity of pathologic migration and the likelihood of spontaneous repositioning of teeth and closure of diastemata.

Managing moderate to severe cases of acquired diastemata may necessitate a complex and a sequential intervention involving periodontic, orthodontic, and prosthodontic measures.27,28 Such interdisciplinary approaches can be successful in restoring health, function, and esthetics, but they may also be time-consuming and financially difficult for many patients. Management of such cases typically requires periodontal therapy (nonsurgical and sometimes surgical) aimed at stabilizing the periodontium prior to orthodontic and restorative therapy. In cases of severe pathologic tooth migration, extraction of hopeless teeth with severe clinical attachment loss and mobility may be necessary in order to achieve optimal oral function and esthetics.
Several studies29,30 have stressed the importance of a stable and healthy periodontium prior to, during, and after orthodontic therapy. This is because orthodontic movement in the presence of periodontitis is thought to potentially intensify periodontitis, leading to additional bone and attachment loss.
ROLE OF THE DENTAL HYGIENIST
Dental hygienists may encounter patients with diastemata. As patients often feel more comfortable asking dental hygienists questions regarding their oral health, clinicians should be able to recognize pathologic tooth migration and address these concerns with patients. If minor pathologic tooth migration appears to be the result of periodontitis, thorough scaling and root planing and improved self-care may reverse it completely. If the migration fails to resolve, periodontal surgery as well as orthodontic and prosthetic measures may be necessary. Dental hygienists should stress the importance of regular maintenance visits to prevent any relapse and reappearance of the diastema, especially in patients with a history of periodontitis.
CONCLUSION
While the presence of diastemata in children is common and a normal sequela of growth and development, the formation of new diastemata in adults is not. Tooth drifting, supereruption, and rotation of teeth in adults are warning signs of advanced periodontitis and are generally termed pathologic tooth migration. Identification and mitigation of all causative factors are essential to proper management of these cases.
Although the process is unpredictable, spontaneous resolution of small amounts of pathologic tooth migration is possible in mild cases after the causative factors have been removed. Moderate to severe cases of pathologic tooth migration usually necessitate an interdisciplinary approach of periodontal therapy in combination with restorative or orthodontic treatment.
REFERENCES
- Taylor JE. Clinical observations relating to the normal and abnormal frenum labii superioris. Am J Orthodont Oral Surg. 1939;25:646–650.
- Gardiner JH. Midline spaces. Dent Pract Dent Rec. 1967;17:287–298.
- Weyman J. The incidence of median diastema during the eruption of the permanent teeth. Dent Pract Dent Rec. 1967;17:276–278.
- Baum AT. The midline diastema. J Oral Med. 1966;21:30–39.
- Broadbent BH: The face of the normal child (diagnosis, development). The Angle Orthodontist. 1937;7(4):183–208.
- Dewel BF. The labial frenum, midline, diastema, and palatine papilla: a clinical analysis. Dent Clin N Am. 1966;10:175–184.
- Johnson ED, Larson BE. Thumb-sucking: classification and treatment. ASDC J Dent Child. 1993;60:392–398.
- Huang WJ, Creath CJ. The midline diastema: a review of its etiology and treatment. Pediatr Dent. 1995;27:171–179.
- Chasens AI. Periodontal disease, pathologic tooth migration and adult orthodontics. N Y J Dent. 1979;49:40–43.
- Towfighi PP, Brunsvold MA, Storey AT, Arnold RM, Willman DE, McMahan CA. Pathologic migration of anterior teeth in patients with moderate to severe periodontitis. J Periodontol. 1997;68:967– 972.
- Martinez-Canut P, Carrasquer A, Magán R, Lorca A. A study on factors associated with pathologic tooth migration. J Clin Periodontol. 1997;24:492– 497.
- Demetriou N, Tsami-Pandi A, Parashis A. Is it possible for periodontal patients to recognize periodontal disease? Stomatologia (Athenai). 1991;47:284–295.
- Weinstein S, Haack DC, Morris LY, Snyder BB, Attaway HE. On an equilibrium theory of tooth position. The Angle Orthodontist. 1963;33(1):1–26.
- Hirschfeld L. The dynamic relationship between pathologically migrating teeth and inflammatory tissue in periodontal pockets: A clinical study. J Periodontol. 1933;4:35–47.
- Del Fabbro M, Francetti L, Bulfamante G, Cribiu M, Miserocchi G, Weinstein RL. Fluid dynamics of gingival tissues in transition from physiological condition to inflammation. J Periodontol. 2001;72:65–73.
- Fu E, Nieh S, Wikesjö UM, Lin FG, Shen EC. Gingival overgrowth and dental alveolar alterations: possible mechanisms of cyclosporin-induced tooth migration. An experimental study in the rat. J Periodontol. 1997;68:1231–1236.
- Brunsvold MA. Pathologic tooth migration. J Periodontol. 2005;76:859–866.
- Chasens AI. Incisal guidance and the management of esthetic and dysfunctional problems. Alpha Omegan. 1980;73:43–46.
- Brunsvold MA, Zammit KW, Dongari AI. Spontaneous correction of pathologic migration following periodontal therapy. Int J Periodontics Restorative Dent. 1997;17:182–189.
- Sato S, Ujiie H, Ito K. Spontaneous correction of pathologic tooth migration and reduced infrabony pockets following nonsurgical periodontal therapy: a case report. Int J Periodontics Restorative Dent. 2004;24:456–461.
- Kumar V, SA, Thomas C. Reactive repositioning of pathologically migrated teeth following periodontal therapy. Quintessence Int. 2009;40:355– 358.
- Singh J, Deshpande RN. Pathologic migration– spontaneous correction following periodontal therapy: a case report.Quintessence Int. 2002;33:65–68.
- Dadlani H, Ramachandra SS, Mehta DS. Spontaneous correction of pathologically migrated teeth with periodontal therapy alone. J Indian Soc Periodontol. 2013;17:531–534.
- Manor A, Kaffe I, Littner MM. “Spontaneous” repositioning of migrated teeth following periodontal surgery. J Clin Periodontol. 1984;11:540–545.
- Gaumet PE, Brunsvold MI, McMahan CA. Spontaneous repositioning of pathologically migrated teeth. J Periodontol. 1999;70:1177–1184.
- Rohatgi S, Narula SC, Sharma RK, Tewari S, Bansal P. Clinical evaluation of correction of pathologic migration with periodontal therapy. Quintessence Int. 2011;42:e22–e30.
- Duncan WJ. Realignment of periodontallyaffected maxillary teeth–a periodontist’s perspective. Part II: Case reports. N Z Dent J. 1997;93:117–123
- Oh SL. An interdisciplinary treatment to manage pathologic tooth migration: a clinical report. J Prosthet Dent. 2011;106:153–158.
- Re S, Corrente G, Abundo R, Cardaropoli D. Orthodontic treatment in periodontally compromised patients: 12-year report. Int J Periodontics Restorative Dent. 2000;20:31–39.
- Artum J, Urbye KS. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofac Orthop. 1988;93:143–148.
From Dimensions of Dental Hygiene. July 2015;13(7):53–56.



