Periodontal Care for Older Adults
Treating periodontally involved teeth and maintaining existing dentition are cost-effective approaches to periodontal care among older adults.
This course was published in the July 2015 issue and expires July 31, 2018. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the risk factors that affect periodontal and peri-implant health in older adults.
- Discuss why it may be more cost-effective to treat periodontally involved teeth as opposed to replacing them with implants or other prostheses.
- Explain the treatment planning concepts for treating periodontal diseases in older adults.
INTRODUCTION
Older adults make up one of the fastest growing segments of the world’s population. When examining and treatment planning for older adults, it is vital to develop appropriate prevention and treatment modalities. A cohesive approach to treating this important patient population includes evaluating an individual’s level of dependency—regardless of chronological age—to determine his or her level of function and the amount of care needed to accomplish everyday tasks. We hope you find this practical approach to exploring periodontal diseases to be a valuable resource in helping you provide a more integrated and focused means of assessing the need for dental services. The Colgate-Palmolive Company is delighted to have provided an unrestricted educational grant to support “Periodontal Care for Older Adults” in collaboration with the American Academy of Periodontology.
—Matilde Hernandez, DDS, MS, MBA
Dental Science Liaison Colgate Oral Pharmaceuticals
FROM THE AMERICAN ACADEMY OF PERIODONTOLOGY
Adults age 65 and older have the highest incidence of periodontal disease in the United States. When treating periodontal disease in older adults, the philosophy of saving teeth takes on an increased level of importance. In this article “Periodontal Care for Older Adults,” educator and American Academy of Periodontology (AAP) member Sivaraman Prakasam, BDS, MDS, PhD, explores the unique considerations facing periodontists and dental hygienists as they plan treatment for this patient population, including the risks of peri-implantitis and the financial implications of treatment.
The common misconception that losing teeth is a normal part of aging is just that—a misconception. Patients of all ages can keep their natural teeth for a lifetime with the proper care and timely treatment from dental professionals. In the event that periodontal disease is present, a periodontist is the specialist best suited to treat and prevent this serious threat to oral health, which can lead to tooth loss if left unaddressed. Dental hygienists play an invaluable role in the care of older adults as they educate patients on the importance of an effective and consistent at-home oral hygiene routine. Once again, the AAP is proud to work with Dimensions of Dental Hygiene and Colgate-Palmolive to help you turn research into real-life application for your practice and the patients you treat.
—Joan Otomo-Corgel, DDS, MPH, President, American Academy of Periodontology
Clinical Professor, University of California, Los Angeles School of Dentistry
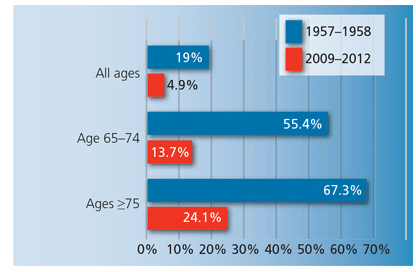
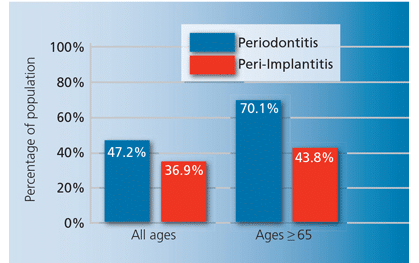
The population of older adults (age 65 or older) in the United States is growing, with numbers increasing from 35 million in 2001 to 40.3 million in 2010.1 In 2010, older adults represented about 13% of total population.1 In 2030, this will grow to 19%.1 While advances in health care have increased life expectancy in the US, the prevalence of chronic diseases also has increased.2 Similarly, advances in dental care have reduced the prevalence of edentulism. While approximately 19% of US adults were edentulous in the late 1950s, only 4.9% had experienced complete tooth loss from 2009 to 2012 (Figure 1).3 Similar trends are seen in older adults, with the rate of edentulism among individuals age 65 to 74 decreasing from 55.4% in 1985 to 13.7% in 2012.3 With an increase in tooth retention comes a rise in the prevalence of chronic periodontal diseases. In fact, the prevalence of periodontitis mirrors the prevalence of other chronic diseases, with nearly half of US adults exhibiting some form of periodontal disease.4 The prevalence of periodontal diseases increases with age—about 70.1% of older adults have some form of periodontitis (Figure 2), with approximately 64.2% experiencing moderate to severe forms of the disease.4
The prevalence of peri-implantitis—an inflammatory disease that leads to the loss of implant-supporting bone—is anticipated to rise, as replacement of teeth with dental implants is popular.5 A recent systematic review and meta-analysis on the global prevalence of peri-implantitis revealed that 63.4% of participants had peri-implant mucositis—an inflammatory disease process involving soft tissue surrounding an implant—while 18.8% were diagnosed with peri-implantitis.5,6 A study of Belgian adults reported that the prevalence of peri-implantitis was higher among older adults (43.8%) than younger adults (30.9%).4,7
These epidemiological data suggest a need for special emphasis on the care of periodontal and peri-implant health among older adults. This focus is further warranted considering the presence of additional risk factors in this age group. Older adults are at high risk of xerostomia and hyposalivation.8,9 Reduced salivary flow increases the risk of microbial colonization of teeth and implants and can lead to caries, periodontal diseases, and peri-implantitis.10 Older adults typically take multiple medications due to their comorbidities, which not only raises the risk of hyposalivation but also can complicate treatment planning.10 Many of the medical conditions and comorbidities present in this population impact periodontal health. The four leading chronic diseases among older adults are diabetes mellitus, chronic respiratory diseases, cardiovascular disease, and cancer, all of which increase the risk for oral diseases.10 An unhealthy diet, poor oral hygiene, and tobacco use may exacerbate the effects of aging on periodontal health.10
PERIODONTAL TREATMENT TO RETAIN TEETH
As the occurrence of periodontal diseases increases with age, some may wonder why teeth with active periodontitis should be retained instead of being replaced with dental implants. Part of the answer lies in the fact that peri-implantitis shares the same risk factors as periodontitis. Patients with active periodontitis and even stabilized periodontiums have increased prevalence of peri-implantitis. Martin et al11 did a cost-effectiveness analysis of periodontal treatment vs a three-unit bridge or single tooth replacement.11 They found that the cost of periodontal treatment divided by the number of teeth preserved ranged from $1,405 to $4,895 for patients at high and moderate risk combined with severity of chronic periodontitis. The cost of a three-unit bridge was $3,416, and the cost of a single tooth replacement was $4,787. They concluded that treating periodontal diseases could be justified solely based on the ability to preserve teeth, regardless of disease severity.11 Consequently, preservation of teeth with periodontal treatment as opposed to replacement with implants may be particularly relevant for older adults whose comorbidities may limit their ability to perform adequate oral hygiene and/or inhibit their compliance. In fact, Fardal and Grytten12 reported that the cost of maintaining dental implants was five times higher than the expense of maintaining teeth with periodontal diseases. Therefore, it may be safe to conclude periodontal treatment is becoming increasingly necessary for older adults.
TREATMENT PLANNING CONCEPTS IN OLDER ADULTS
While chronological age often is used when treatment planning for older adults, Ettinger and Beck13 suggest that aging populations should be divided into three groups based on their ability to seek dental care: functionally independent older adults, frail older adults, and functionally dependent older adults.14 Functionally independent older adults live in their communities without assistance. They can access dental care on their own and make decisions based on their financial ability and values. As functionally independent older adults often present with chronic medical conditions, treatment planning must involve a thorough review of medical history, consultation with patients’ physicians, and comprehensive assessment of how their medical conditions and medications may influence dental care.
Frail older adults usually live in their own communities, but they may need support from family/friends or professional services. Access to dental care for these individuals usually is dependent on the help of patients’ support structures. The systemic health of frail older adults must also be evaluated. Additionally, an assessment of their ability to perform oral hygiene independently and to tolerate dental care must be part of treatment planning.
Functionally dependent older adults no longer live independently. They usually need transportation to dental offices, or services may need to be provided in their institutional setting.
An important consideration when formulating treatment plans for older adults is their ability to provide informed consent. Approximately 71% of adults age 60 and older have trouble understanding print materials, which may present a serious barrier to obtaining informed consent.15 Short-term memory loss and early cognitive deficits also can impact consent capacity.14 Therefore, closely reviewing medical history and closely working with their medical providers/caregivers are critical.
Shay16 proposed a useful system for planning oral care in older adults using the oral, systemic, capability, autonomy, and reality (OSCAR) tool. It provides a framework for evaluating patients’ oral and systemic health status; evaluating their functional capability or availability of support structure to access dental care and provide at-home oral care; assessing their ability to give informed consent; and evaluating the reality of their situations.
Berkey et al17 suggested a series of questions to help treatment plan for older adults that incorporates the patient’s desires and expectations, type and severity of dental need and its impact on quality of life, likelihood of positive outcomes, availability of reasonable treatment options, ability to tolerate treatment, capability to perform oral self-care, financial constraints, capabilities of dental care provider, and other issues.
Several diseases and conditions are known to impact oral health. Uncontrolled diabetes can result in increased attachment loss and recurrent periodontal abscesses and tooth loss.18,19 Uncontrolled hypertension limits treatment options, such as the possibility of elective periodontal surgery and choice of local anesthetic. Systemic conditions that may contraindicate surgery or affect wound healing also limit treatment options.18,19
Many medications prescribed to older adults impact periodontal health. Older adults often are on several anti-inflammatory drugs, some of which may promote periodontal health.20 Several nonsteroidal anti-inflammatory drugs also inhibit alveolar bone loss.21 In contrast, long-term corticosteroid use has no obvious influence on periodontal diseases.22 Anti-TNF-? therapies are now used routinely to treat chronic inflammatory diseases (eg, rheumatoid arthritis, psoriasis). One anti-TNF-? medication has been shown to inhibit bone resorption in patients at risk of periodontal diseases, with probing depths remaining unaffected and the severity of gingival inflammation increased.23 Other studies with smaller sample sizes have shown improved periodontal health in patients who undergo anti-TNF-α infusions.24
Another common drug that may impact oral care is bisphosphonates. Patients on intravenous bisphosphonates may be at increased risk of osteonecrosis of the jaw after invasive periodontal or oral surgeries. Oral bisphosphonates seem to carry a minuscule risk, but drug holidays may be considered in consultation with the medical team when surgeries are planned in these patients.20 Anti-platelet and anti-coagulant drugs can increase bleeding during or after periodontal surgery and, therefore, should be discussed with the medical team prior to performing treatment.25,26 Statins also are widely prescribed in older adults, and they may have some beneficial effects on periodontal diseases.20 Some older adults may be receiving cancer treatment, and the impact of these medications on oral health need to be assessed in consultation with the prescribing physician.
Once appropriate assessments are completed, a careful clinical examination and diagnostic workup must be performed. Wennstrom27 proposed a simplified algorithm for treating periodontal diseases in older adults that is applicable to routine periodontal therapy for any age group. Following a careful medical and dental diagnostic workup, clear goals of therapy are defined and informed consent is obtained from the patient. Appropriate, nonsurgical therapy involving both mechanical debridement and adjunctive local or systemic pharmacological therapy is performed. Re-evaluation is conducted at 4 weeks to 6 weeks. The need for further nonsurgical management and appropriate surgical management is then evaluated and active therapy performed. In addition to this algorithm, Wennstrom’s decision tree incorporates the element of remaining alveolar bone after active therapy for older adults. If bone levels are not age appropriate, Wennstrom recommends continued supportive therapy until clinical stability is reached or, alternatively, examining the need for reinitiating active therapy.27 A more elaborate but generic oral care algorithm developed by Ettinger and Beck14 also is a useful tool in treatment planning for older adults.
When appropriate, periodontal surgery should be considered as a viable treatment option. In fact, age is not a contraindication to periodontal surgery.28 Post-operative healing outcomes are no different in older adults when compared to younger individuals.28 The most critical factor in determining success of periodontal surgery is the patient’s ability to maintain adequate oral hygiene and the frequency of professional care.29–31
The presence of a disability may affect patient compliance with an oral hygiene regimen. In the US, 51.8% of older adults have at least one disability and 36.9% have a severe disability.32 Among adults older than 80, 71% have some disability and 29.2% need assistance for daily activities.32 As such, it’s important to evaluate the ability of an older patient to maintain oral hygiene when considering surgical therapy. Whenever possible, regenerative procedures should be considered. If resective procedures are planned, strategies to minimize root caries14—including plaque control measures, fluoride application, and dietary counseling—should be recommended.27
One of the key components of periodontitis management is supportive periodontal maintenance therapy.33,34 According to Kerry,33 supportive periodontal therapy has three objectives: to prevent progression or recurrence of periodontitis in treated patients; to reduce or prevent tooth loss; and to increase the probability of identifying and treating other oral conditions. While the prevalence of periodontal diseases appears to increase with age, especially in individuals without systematic periodontal care,35 periodontal disease is not evident in properly treated and maintained older adults.36,37 A 3-month to 6-month interval for customized maintenance recare appointments may be appropriate for older adults depending on their periodontal status and their ability to perform adequate oral hygiene. Wennstrom27 also advocates topical application of chlorhexidine for 4 weeks after maintenance visits to extend the necessary interval between supportive care.
Although studies on periodontal treatment outcomes in older adults are sparse, existing research does not support the conclusion that age is a significant risk factor. In fact, most studies indicate that the development of periodontal disease in older adults can be prevented or stabilized with treatment to control dental plaque.
CASE STUDY
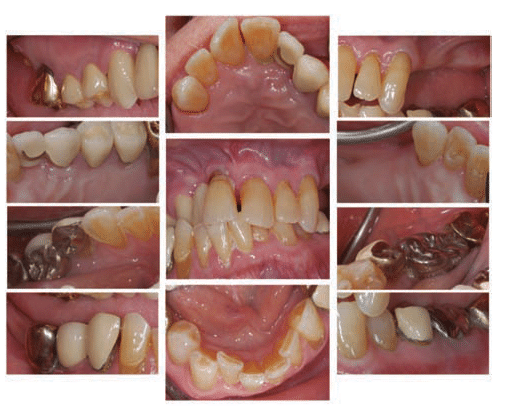
In this case study, treatment planning concepts for older adults are illustrated using Ettinger’s framework.14 A 90-year-old white man was referred by his general dentist because of spontaneous pain in his front right tooth, but the pain had since resolved. He presented to the appointment requesting improved esthetics in his front teeth. The patient had experienced some tooth loss despite receiving regular prophylaxes. He also had an extensive medical history, undergoing a right leg angioplasty 4 years prior, followed by a left leg arterial bypass and triple bypass surgeries in the same year. The patient had a history of prostate cancer that was now in remission, in addition to depression, for which he was taking medication. He also was taking several medications related to his cardiovascular state and prostate problems. The extraoral exam did not reveal any significant findings. Intraoral exams and complete periodontal charting was done. Clinical and radiographic evaluations also were conducted (Figure 3). The patient had an O’Leary plaque score of 65% and a bleeding score of 35%.
Treatment Planning Framework: The patient was classified as functionally independent. No cognitive impairments were noted. The patient was able to understand the risks and benefits and provide informed consent. Consultation with his medical team was necessary given his complex medical history and polypharmacy.
Patient’s Desire and Expectations: His expectations were somewhat unrealistic given his initial presentation. Careful counseling may be necessary to temper his expectations to the reality of his current oral health status.
Type and Severity of Dental Need: Patient was diagnosed with localized severe chronic periodontitis and generalized mild chronic periodontitis. He had several missing teeth. Radiographs revealed bone loss extending to two threads to three threads on the lower right implants, which also had deep probing depths and bleeding on probing (peri-implantitis). He was diagnosed with secondary occlusal trauma and mucogingival defects around several teeth.
Impact on Quality of Life: Lack of posterior support on the left side of the mouth along with his inadequate oral hygiene contributed to deterioration of his oral health and potentially affected his nutritional status.
The Probability of Positive Outcomes: With treatment and proper motivation, probability of positive outcomes was high.
Reasonable Treatment Alternatives: Treatment options included achieving periodontal stability either nonsurgically or surgically after strategic extractions and replacement of edentulous areas with partial dentures or with implants supported by fixed partial or hybrid dentures.
Ability to Tolerate the Stress of Treatment: Given the patient’s extensive medical history, stress reduction protocols were recommended. Monitoring of vitals may be necessary before, during, and after the procedure.
Capability to Maintain Oral Health: The patient had the potential to maintain oral health given adequate motivation and instructions.
Financial and Other Resources: The patient had the ability to pay for his care and the necessary support structure.
Capabilities of the Oral Health Professionals: The patient’s health care providers need to be aware of limitations in their capabilities and seek additional referrals when necessary.
SUMMARY
Treating periodontally involved teeth and maintaining existing dentition are cost-effective strategies compared with tooth removal and replacement. Therefore, periodontal care must be given serious consideration when developing treatment plans for older adults. Several frameworks are available to aid in the care of this patient population. An optimistic but realistic periodontal treatment plan geared toward retaining a patient’s dentition is a viable option for older adults.
REFERENCES
- Vincent GK, Velkoff VA. The Next Four Decades, The Older Population in the United States: 2010 to 2050. Available at: census.gov/prod/2010pubs/p25-1138.pdf. Accessed June 17, 2015.
- Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis. 2013;10:E65.
- Slade GD, Akinkugbe AA, Sanders AE. Projections of US edentulism prevalence following 5 decades of decline. J Dent Res. 2014;93:959–965.
- Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91:914–920.
- Christman A, Schrader S, John V, Zunt S, Maupome G, Prakasam S. Designing a safety checklist for dental implant placement: A Delphi study. J Am Dent Assoc. 2014;145:131–140.
- Atieh MA, Alsabeeha NH, Faggion Jr CM, Duncan WJ. The frequency of peri-implant diseases: a systematic review and meta-analysis. J Periodontol. 2013;84:1586–1598.
- Marrone A, Lasserre J, Bercy P, Brecx MC. Prevalence and risk factors for peri-implant disease in Belgian adults. Clin Oral Implant Res. 2013;24:934–940.
- Van der Putten G-J, Brand HS, De Visschere LM, Schols JM, de Baat C. Saliva secretion rate and acidity in a group of physically disabled older care home residents. Odontology. 2013;101:108–115.
- Ciancio SG. Medications’ impact on oral health. J Am Dent Assoc. 2004;135:1440–1448.
- Van der Putten GJ, De Visschere L, van der Maarel-Wierink C, Vanobbergen J, Schols J. The importance of oral health in (frail) elderly people—a review. European Geriatric Medicine. 2013;4(5):339–344.
- Martin JA, Fardal Ø, Page RC, et al. Incorporating severity and risk as factors to the fardal cost-effectiveness model to create a cost–benefit model for periodontal treatment. J Periodontol. 2014;85:31–39.
- Fardal Ø, Grytten J. A comparison of teeth and implants during maintenance therapy in terms of the number of disease-free years and costs—an in vivo internal control study. J Clin Periodontol. 2013;40:645–651.
- Ettinger RL, Beck JD. Geriatric dental curriculum and the needs of the elderly. Spec Care Dent. 1984;4:207–213.
- Ettinger RL. Treatment planning concepts for the aging patient. Aust Dent J. 2015;60(Suppl 1): 71–85.
- Rudd R, Horowitz AM. The role of health literacy in achieving oral health for elders. J Dent Educ. 2005;69:1018–1021.
- Shay K. Identifying the needs of the elderly dental patient. The geriatric dental assessment. Dent Clin North Am. 1994;38:499–523.
- Berkey DB, Berg RG, Ettinger RL, Mersel A, Mann J. The old-old dental patient: the challenge of clinical decision-making. J Am Dent Assoc. 1996;127:321–332.
- Reynolds MA. Modifiable risk factors in periodontitis: at the intersection of aging and disease. Periodontol 2000. 2014;64:7–19.
- Boehm TK, Scannapieco FA. The epidemiology, consequences and management of periodontal disease in older adults. J Am Dent Assoc. 2007;138(Suppl):26S–33S.
- Heasman PA, Hughes FJ. Drugs, medications and periodontal disease. Br Dent J. 2014;217:411–419.
- Feldman RS, Szeto B, Chauncey HH, Goldhaber P. Non-steroidal anti-inflammatory drugs in the reduction of human alveolar bone loss. J Clin Periodontol. 1983;10:131–136.
- Safkan B, Knuuttila M. Corticosteroid therapy and periodontal disease. J Clin Periodontol. 1984;11:515–522.
- Pers J-O, Saraux A, Pierre R, Youinou P. Anti-TNF-alpha immunotherapy is associated with increased gingival inflammation without clinical attachment loss in subjects with rheumatoid arthritis. J Periodontol. 2008;79:1645–1651.
- Smolen JS, Han C, Bala M, et al. Evidence of radiographic benefit of treatment with infliximab plus methotrexate in rheumatoid arthritis patients who had no clinical improvement: a detailed subanalysis of data from the anti-tumor necrosis factor trial in rheumatoid arthritis with concomitant therapy study. Arthritis & Rheum. 2005;52:1020–1030.
- Elad S, Chackartchi T, Shapira L, Findler M. A critically severe gingival bleeding following non-surgical periodontal treatment in patients medicated with anti-platelet. J Clin Periodontol. 2008;35:342–345.
- Thomason JM, Seymour RA, Murphy P, Brigham KM, Jones P. Aspirin-induced post-gingivectomy haemorrhage: a timely reminder. J Clin Periodontol. 1997;24:136–138.
- Wennström JL. Treatment of periodontal disease in older adults. Periodontol 2000. 1998;16:106–112.
- Lindhe J, Socransky S, Nyman S, Westfelt E, Haffajee A. Effect of age on healing following periodontal therapy. J Clin Periodontol. 1985;12:774–787.
- Axelsson P, Lindhe J. Effect of controlled oral hygiene procedures on caries and periodontal disease in adults. J Clin Periodontol. 1981;8:239–248.
- Lindhe J, Nyman S. The effect of plaque control and surgical pocket elimination on the establishment and maintenance of periodontal health. A longitudinal study of periodontal therapy in cases of advanced disease. J Clin Periodontol. 1975;2:67–79.
- Westeelt E, Nyman S, Socransky S, Lindhe J. Significance of frequency of professional tooth cleaning for healing following periodontal surgery. J Clin Periodontol. 1983;10:148–156.
- Brault MW. Americans with Disabilities: 2010. Available at: oppi.gobierno.pr/Censo_C_SPAN_Slides_Disability2012.pdf. Accessed June 17, 2015.
- Kerry GJ. Supportive periodontal treatment. Periodontol 2000. 1995;9:176–185.
- Wilson TG. Supportive periodontal treatment introduction–definition, extent of need, therapeutic objectives, frequency and efficacy. Periodontol 2000. 1996;12:11–15.
- Papapanou PN, Wennström JL, Gröndahl K. A 10–year retrospective study of periodontal disease progression. J Clin Periodontol. 1989;16:403–411.
- Wennström JL, Serino G, Lindhe J, Eneroth L, Tollskog G. Periodontal conditions of adult regular dental care attendants. J Clin Periodontol. 1993;20:714–722.
- Axelsson P, Lindhe J, Nyström B. On the prevention of caries and periodontal disease. J Clin Periodontol. 1991;18:182–189.
From Dimensions of Dental Hygiene. July 2015;13(7):45–50.

