KIEFERPIX/ISTOCK/GETTY IMAGES PLUS
KIEFERPIX/ISTOCK/GETTY IMAGES PLUS
Supporting Oral Health Among Breastfed Infants
Exclusively breastfed babies may be at increased risk for vitamin D deficiency, which can affect enamel development and caries risk.
This course was published in the February 2021 issue and expires February 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe the relationship between vitamin D deficiency, enamel development and caries risk in infants and young children.
- Explain recommended vitamin D serum levels and supplementation guidelines for mothers and infants.
- In the context of vitamin D levels and oral health, discuss dental professionals’ role in prenatal and postnatal care.
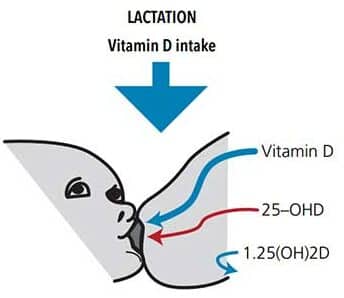
Breastfeeding within the first year of life is encouraged because it decreases health risks and provides nutritional benefits for the infant and mother. The American Academy of Pediatrics recommends “exclusive breastfeeding for 6 months, followed by continued breastfeeding as complementary foods are introduced, with continuation of breastfeeding for 1 year or longer as mutually desired by mother and infant.”1 Among children born in 2016, 47.5% were exclusively breastfed for 3 months, and 25% were exclusively breastfed until 6 months.2 While breastfeeding exclusively is recommended for infants and provides a higher intake of nutrients than other feeding practices, the vitamin D concentration in breast milk is usually insufficient to meet the infant’s needs.3 For example, very low concentration of vitamin D (approximately 10 IU/L to 80 IU/L) passes into human breast milk, which reflects 1.5% to 3% of the maternal level (Figure 1); this may contribute to vitamin D deficiency in the infant.4–8 This paper will describe the relationship between vitamin D deficiency and enamel development, provide national supplementation recommendations for mothers and children, and discuss the role of oral health professionals in promoting dental health among these patients.
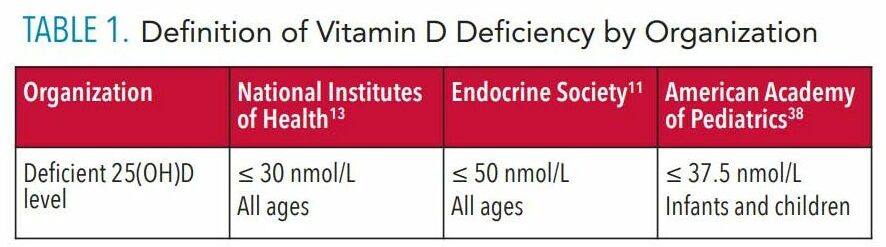
Among United States women of childbearing age (20 to 44), a national study revealed 10% to 12% are vitamin D deficient, and 25% to 27% have inadequate levels of vitamin D.9 A high prevalence of maternal deficiency persists, despite the daily intake of prenatal vitamins containing 400 IU vitamin D.5 However, providing vitamin D-deficient pregnant and lactating women with supplements containing high concentrations of vitamin D (1,000 IU to 2,000 IU, and up to 4,000 IU in latter cases) is thought to be safe.10 Deficiencies typically present when intake is lower than recommended levels—25‐hydroxyvitamin D [25(OH)D] ≤ 30 to ≤ 50 nanomoles per liter (nmol/L)—over time (Table 1). Vitamin D deficiency is common across all age groups.11 Contributing factors include limited sunlight exposure and restricted diets due to allergies or intolerance (eg, dairy), veganism, or impaired absorption (eg, digestive disorders).12 According to the National Institutes of Health, serum vitamin D levels ≥ 50 nmol/L in all populations is considered adequate for bone and general health.13
Inadequate levels of vitamin D during rapid phases of enamel formation (in utero for primary dentition, and post-natal for permanent dentition) increase the risk of interruptions in the enamel matrix, which can lead to defects, such as enamel hypoplasia.14 These enamel defects increase susceptibility to caries, a process that is led by Streptococcus mutans bacteria colonized within dental plaque.15 Within this plaque, bacteria can easily adhere to a defective enamel surface, creating an environment prime for lesion development.14,16 Dental caries is considered the most common preventable chronic disease of childhood, with 21.4% of children younger than 5 experiencing disease.17 The literature suggests a relationship between low vitamin D levels during the prenatal period and caries in the primary dentition.18,19 In addition, developmental defects—including enamel hypoplasia—have been associated with caries in the primary dentition.14,18 While caries is a multifactorial process, vitamin D-deficient infants have a greater risk for developing enamel defects, thus increasing caries risk.
Given the relationship between vitamin D and enamel development, oral health professionals must provide expectant mothers and caregivers with the resources needed to minimize the risk of vitamin D deficiency in infants who will be exclusively breastfed.
ENAMEL DEVELOPMENT
Maternal concentrations of vitamin D directly relate to the recommended 25(OH)D serum level available to transfer to human breast milk. Infants who are exclusively breastfed by women with vitamin D intake of 400 IU/day (standard prenatal vitamin quantity) typically attain a circulating 25(OH)D concentration in the “marginally sufficient” to “severely deficient” (< 12.5 nmol/L) range.20
Vitamin D plays a critical role in enamel, dentin, and oral bone formation, as ameloblasts and odontoblasts are target cells for 1,25-dihydroxyvitamin D, the active form of vitamin D.21 Adequate amounts of vitamin D during rapid phases of tooth development can prevent enamel defects, such as hypocalcification, which is also associated with caries.14,18,22,23 An enamel surface with compromised mineralization, porosity, and irregularities is a predisposing risk for plaque accumulation. Defective enamel (eg, pitting, grooves or irregularities, including hypoplasia) increases the risk of early colonization by cariogenic bacteria, resulting in caries.18 There is an increased risk of developing enamel defects in a vitamin D-deficient environment.
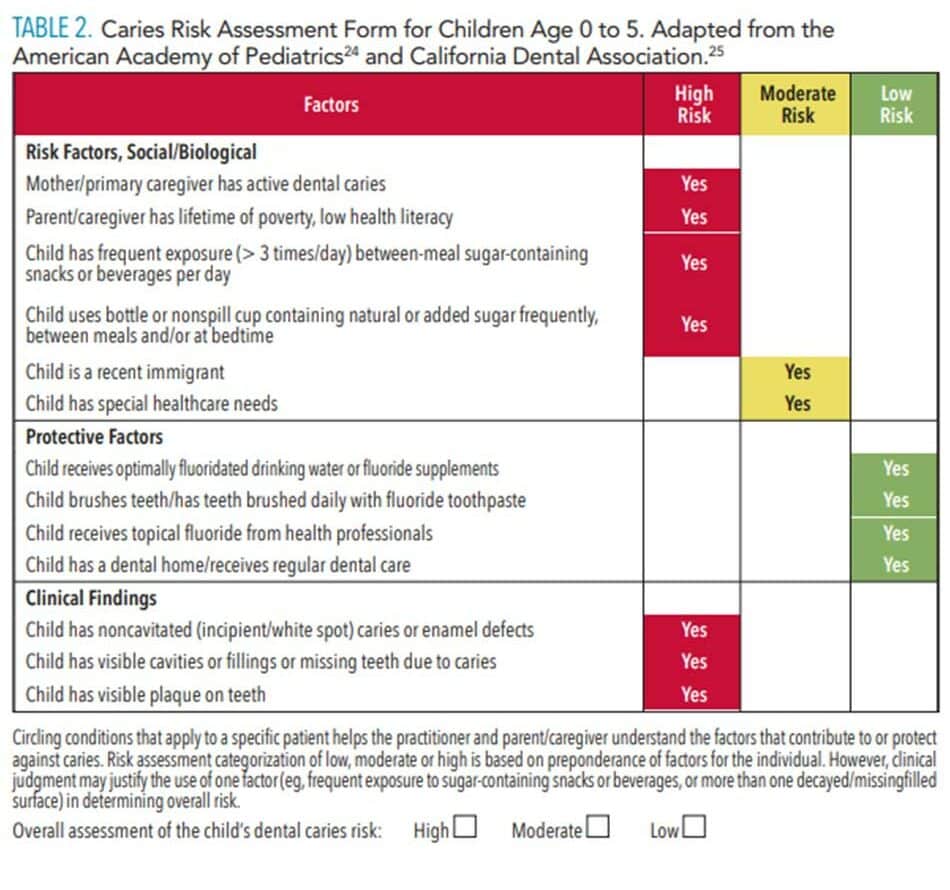
The most recent revision of the caries risk assessment form includes enamel defects as a risk factor in both pediatric age groups (0 to age 5, and 6 and older), and places children with defects into a high-risk category.24,25 This risk assessment tool can be useful for oral health education and anticipatory guidance with the caregiver and child during the initial and subsequent dental visits. When moderate- to high-risk factors are identified at a young age, early interventions can be discussed and implemented to reduce caries risk (Table 2).24,25
![Caries Risk Assessment Form]() VITAMIN D SUPPLEMENTATION
VITAMIN D SUPPLEMENTATION
Infants born to vitamin D-deficient mothers are often vitamin D deficient at birth and at increased risk for enamel hypoplasia.18,19,26–29 Thus, adequate maternal vitamin D levels during the last trimester of pregnancy are essential in establishing the infant’s vitamin D reserves.10–30 These stored levels of 25(OH)D are depleted in the neonate within 6 weeks to 8 weeks post-partum, and the infant must depend solely on vitamin D from external sources, such as supplementation.22,31 Vitamin D supplementation during enamel development is essential for infants who are identified as vitamin-D deficient. To reduce the risk of vitamin D deficiency, the American Academy of Pediatrics recommends all children who are breastfed, or consume less than 1 liter of formula per day, receive vitamin D supplements (400 IU/day) beginning in the first few days of life through the first year.32 From 2009 to 2012, less than one in five US breastfed infants age 0 to 11 months met the American Academy of Pediatrics’ recommendations of 400 IU/day of vitamin D supplementation. Among this group, a supplement medicament was the most common form of consumption other than the use of formula.33 In general, supplementation should continue until the infant receives a minimum of 1 liter per day of vitamin D-fortified formula or whole milk.34,35 Supplementing exclusively breastfed infants daily with 400 IU of vitamin D provides consistent serum concentrations of 25(OH)D at ≥ 50 nmol/L.36 Oral supplementation options for infants in the US are dispensable in the form of liquid drops or milliliter dosing, and are prepared at 400 IU/day.23 Caregivers should be encouraged to utilize the manufacturer-provided dispenser and follow dosing instructions.23,35 The use of oral supplementations can be integrated during diaper changes, bottle preparations, or any daily routine that can be easily adopted by the caregiver.
ROLE OF ORAL HEALTH PROFESSIONALS
With more than 80% of new mothers attempting to breastfeed,2 oral health professionals are in a unique position to provide oral health education to expectant mothers and caregivers during the first 6 months to 12 months post-partum. While prenatal providers and pediatricians are the primary prescribers of vitamin D treatment regimens, dental teams should also be current with vitamin D supplementation recommendations. Understanding the pathways and etiologies leading to developmental defects in the enamel—which may increase caries susceptibility—is essential.
In addition to interactions within the dental office, in 38 states dental hygienists have expanded functions that include providing services in medical settings, federally funded centers, public health offices, community health centers, and clinics.37 The inclusion of preventive dental services and oral health education in these diverse settings provides an opportunity to engage pregnant and post-partum women, caregivers, and infants. In addition, alternative practice settings allow for interprofessional collaborative practice with primary care and prenatal providers who provide health services to women and children. Oral health professionals can promote vitamin D supplementation for mothers and children by:
- Working collaboratively with pediatricians and prenatal and primary care physicians to provide current, evidence-based information on the implications of breast milk and vitamin D deficiency.
- Staying current with evidence-based supplementation recommendations.
- Providing educational materials/information about the benefits of vitamin D supplementation and the effects on oral health.
CONCLUSION
Among healthcare providers, the relationship between breastfeeding exclusively and vitamin D deficiency in infants requires a collaborative approach and ongoing conversations during prenatal and postnatal care. Early interventions—such as prescribing vitamin D supplements and recognizing risk factors for caries—are essential to promoting positive oral and overall health outcomes for the infant.
REFERENCES
- Johnston M, Landers S, Noble L, Szucs K, Viehmann L. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–e841.
- United States Centers for Disease Control and Prevention. Results: Breastfeeding rates. National Immunization Survey. Available at: cdc.gov/breastfeeding/data/nis_data/results.html. Accessed January 14, 2021.
- Daaboul J, Sanderson S, Kristensen K, Kitson H. Vitamin D deficiency in pregnant and breast-feeding women and their infants. J Perinatol. 1997;17:10–14.
- Ala-Houhala M. 25-Hydroxyvitamin D levels during breast-feeding with or without maternal or infantile supplementation of vitamin D. J Pediatr Gastroenterol Nutr. 1985;4:220–226.
- Dawodu A, Tsang RC. Maternal vitamin D status: Effect on milk vitamin D content and vitamin D status of breastfeeding infants. Adv Nutr. 2012;3:353–361.
- Hollis BW, Pittard WB, Reinhardt TA. Relationships among vitamin D, 25-hydroxyvitamin D, and vitamin D-binding protein concentrations in the plasma and milk of human subjects. J Clin Endocrinol Metab. 1986;62:41–44.
- Hollis BW, Roos BA, Draper HH, Lambert PW. Vitamin D and its metabolites in human and bovine milk. J Nutr. 1981;111:1240–1248.
- Thandrayen K, Pettifor J. Maternal vitamin D status: implications for the development of infantile nutritional rickets. Endocrinol Metab Clin North Am. 2010;39:303–320.
- Zhao G, Ford ES, Tsai J, Li C, Croft JB. Factors associated with vitamin D deficiency and inadequacy among women of childbearing age in the United States. ISRN Obstet Gynecol. 2012;2012:691486.
- The American College of Obstetricians and Gynecologists. Committee Opinion. Vitamin D screening and supplementation during pregnancy. Available at: acog.org/-/media/project/acog/acogorg/clinical/files/committee-opinion/articles/2011/07/vitamin-d-screening-and-supplementation-during-pregnancy.pdf. Accessed January 14, 2021.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–1930.
- Naidu RS, Nunn JH. Prevalence of enamel developmental defects and relationship with early childhood caries in Trinidad. J Dent Child (Chic). 2016;83:108–113.
- National Institutes of Health. Office of Dietary Supplements. Vitamin D. Available at: ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/. Accessed January 14, 2021.
- Hong L, Levy S, Warren J, Broffitt B. Association between enamel hypoplasia and dental caries in primary second molars: A cohort study. Caries Res. 2009;43:345–353.
- Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Rev. 1986;50:353–380.
- Carvalho J, Silva E, Gomes R, Fonseca J, Mestrinho H. Impact of enamel defects on early caries development in preschool children. Caries Res. 2011;45:353–360.
- Fleming E, Afful J. Prevalence of total and untreated dental caries among youth: United States, 2015–2016. Available at: cdc.gov/nchs/data/databriefs/db307.pdf. Accessed January 14, 2021.
- Schroth RJ, Lavelle C, Tate R, Bruce S, Billings RJ, Moffatt M. Prenatal vitamin D and dental caries in infants. Pediatrics. 2014;133:e1277–e1284.
- Singleton R, Day G, Thomas T, et al. Association of maternal vitamin D deficiency with early childhood caries. J Dent Res. 2019;98:549–555.
- Ziegler EE, Hollis BW, Nelson SE, Jeter JM. Vitamin D deficiency in breastfed infants in Iowa. Pediatrics. 2006;118:603–610.
- Berdal A, Bailleul-Forestier IB, Davideau J-L, Lézot F. Dento-alveolar bone complex and vitamin D. In: Feldman D, ed. Vitamin D. 2nd ed. Cambridge, Massachusetts: Academic Press; 2005:599–607.
- Mulligan ML, Felton SK, Riek AE, Bernal-Mizrachi C. Implications of vitamin D deficiency in pregnancy and lactation. Am J Obstet Gynecol. 2010;202:429.e1–e9.
- Wagner CL, Greer FR. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142–1152.
- American Academy of Pediatric Dentistry. Caries-risk assessment and management for infants, children, and adolescents. Best Practices: Caries-Risk Assessment and Management. Available at: aapd.org/globalassets/media/policies_guidelines/bp_cariesriskassessment.pdf. Accessed January 14, 2021.
- California Dental Association. CAMBRA. Caries Management by Risk Assessment. Available at: cdafoundation.org/Portals/0/pdfs/cambra_handbook.pdf. Accessed January 14, 2021.
- Cockburn F, Belton NR, Purvis RJ, et al. Maternal vitamin D intake and mineral metabolism in mothers and their newborn infants. Br Med J. 1980;281:11–14.
- Nørrisgaard PE, Haubek D, Kühnisch J, et al. Association of high-dose vitamin D supplementation during pregnancy with the risk of enamel defects in offspring: A 6-year follow-up of a randomized clinical trial. JAMA Pediatr. 2019;173:924–930.
- Reed S, Voronca D, Wingate J, et al. Prenatal vitamin D and enamel hypoplasia in human primary maxillary central incisors: a pilot study. Pediatr Dent J. 2017;27:21–28.
- Seminario AL, Velan E. Vitamin D and dental caries in primary dentition. J Dent Child (Chic). 2016;83:114–119.
- Schoenmakers I, Pettifor J, Peña-Rosas J, et al. Prevention and consequences of vitamin D deficiency in pregnant and lactating women and children: A symposium to prioritise vitamin D on the global agenda. J Steroid Biochem Mol Biol. 2016;164:156–160.
- Hillman LS, Haddad JG. Human perinatal vitamin D metabolism I: 25-hydroxyvitamin D in maternal and cord blood. J Pediatr. 1974;84:742–749.
- Folsom LJ, DiMeglio LA. Recommendations released on prevention, management of rickets. Available at: aappublications.org/news/2017/02/10/Rickets021017. Accessed January 14, 2021.
- Ahrens KA, Rossen LM, Simon AE. Adherence to vitamin D recommendations among US infants aged 0 to 11 months, NHANES, 2009 to 2012. Clin Pediatr (Phila). 2016;55:555–556.
- United States Centers for Disease Control and Prevention. Vitamin D. Available at: cdc.gov/breastfeeding/breastfeeding-special-circumstances/diet-and-micronutrients/vitamin-d.html. Accessed January 14, 2021.
- Jay L, Hoecker MD. Does your baby need a vitamin D supplement? Available at: mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/expert-answers/vitamin-d-for-babies/faq-20058161. Accessed January 14, 2021.
- Wagner CL, Hulsey TC, Fanning D, Ebeling M, Hollis BW. High-dose vitamin D3 supplementation in a cohort of breastfeeding mothers and their infants: a six-month follow-up pilot study. Breastfeed Med. 2006;1:59–70.
- American Dental Hygienists’ Association. Dental Hygiene in Medical Settings and Health Clinics. Available at: adha.org/resources-docs/Dental_Hygiene_in_Medical_Settings.pdf. Accessed January 14, 2021.
- Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M, Drug and Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine Society. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics. 2008;122:398–417.
From Dimensions of Dental Hygiene. February 2021;19(2):26-28,31.