Reducing the Mechanical Demand
How to maintain musculoskeletal health while generating sufficient force for effective periodontal instrumentation.
The repetitive, mechanical tasks that encompass scaling and root planing among other dental hygiene duties put hygienists at high risk for cumulative trauma disorders.1,2 Several neuromuscular and biomechanical risk factors are linked to these work-related musculoskeletal disorders,3,4 including large reaction forces at the hand/instrument interface, repetitive motion of the upper extremity, and sustaining awkward body positioning for prolonged durations.5-7 As periodontal care becomes more challenging, the ability of the neuromuscular system to control joint motion and adequately accommodate the mechanical demand imposed on the musculoskeletal system becomes more difficult. Dental hygienists can protect their own health by using instruments and techniques that reduce or redistribute the mechanical demand imposed on the body in ways that complement the capabilities of their own musculoskeletal system.

Dental hygienists need to deliver quality patient care without incurring detrimental loading that may result in pain or injury to their musculoskeletal systems. During physically demanding periodontal tasks, like deep scaling of calculus, large forces are repeatedly applied along the length of the tooth. This task becomes particularly challenging when done in difficult-to-reach locations. Biomechanical principles can be used to modify periodontal techniques to help reduce or redistribute the mechanical demand imposed on your musculoskeletal system without compromising patient care.8,9
APPLYING FORCE WITHOUT GENERATING PAIN
From a mechanical perspective, effective periodontal instrumentation requires that the dental hygienist precisely position and repeatedly apply forces along the tooth using a pinch grip on a hand instrument. The magnitude and direction of force applied by the instrument on the tooth is equal in magnitude but opposite in direction to the force applied by the tooth on the instrument held by the dental hygienist.10 The force applied to the dental hygienist at the tooth/instrument interface is called a reaction force.
Generating the reaction force between the instrument and tooth during the scaling motion requires precise muscular control of all the joints involved, including those that provide a stable base from which to exert force.11-13 Awkward postures often arise when the dental hygienist is unable to ideally position his or her own body relative to the patient’s jaw because of the workplace environment or a patient’s anatomy. The workspace layout, the muscle force-generating capacity of the dental hygienist in specific body configurations, and task specific mechanical demands and control requirements are important factors that affect the musculoskeletal system.2,3,14-17
1. Find the body positions that are easiest for you to generate the forces necessary for scaling and root planing. If you are fatigued or experiencing pain, find alternative positions that avoid taxing compromised regions of your musculoskeletal system. In general, keep the point of force application at the instrument/tooth interface low relative to your body (below navel/elbow level, Figure 1b). Learn how to achieve this force position in each of your work environments. Positioning the point of force application low often requires some combination of lowering the jaw of the patient in the chair and elevating your body position, eg, standing.
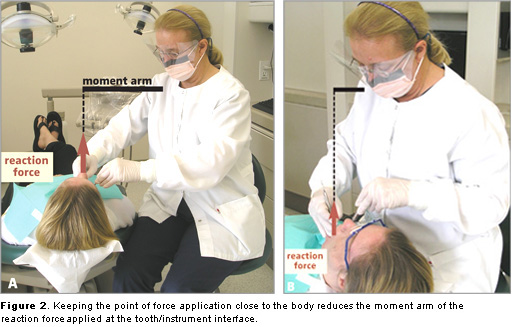
2. Reduce the need for muscle forces by moving your body close to the point of force application while keeping the joints in mid-range. Reaching away from the body to apply force at the instrument/tooth interface increases the moment arm (the perpendicular distance between the line of action of the reaction force and the axis of rotation of the reaction force, Figure 2a).

Decreasing the length of the moment arm by moving closer to the point of force application reduces the mechanical demand imposed on the musculoskeletal system. You can reduce the length of this moment arm by moving your whole body closer to the patient. For example, using dental chairs with a narrow width keeps the dental hygienist close to the patient. This closer body position keeps the joints at mid-range, muscles at more ideal lengths for generating forces, and reduces the moment arm of the reaction force applied at the instrument/tooth interface.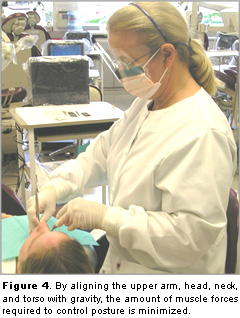
Keeping the joints in the mid-range helps distribute the load transmitted between segments more evenly across the structures surrounding the joints.3,15 Avoiding fully flexed or fully extended joint positions keeps the muscles used to control joint motion at more ideal muscle lengths for generating force (Figure 3b).18,19
3. Align your body with gravity. By aligning the upper arm, head, neck, and torso with gravity, the amount of muscle forces required to maintain your posture is minimized (Figure 4). For example, keeping the upper arm aligned with an upright trunk minimizes the use of the shoulder muscles. In cases where scaling requires visual guidance, maintaining head alignment relative to an upright spine may be facilitated by selecting appropriate instruments, eg, magnification loupes or mirrors, to enhance visual guidance without flexion or excessive rotation of the spine. Flexing the neck in order to see the instrument/tooth interface requires that the neck and trunk extensor muscles generate force to counter the rotation created by the weight of the head. Maintaining alignment of the head center of mass over the spine aligns the weight of the head with the cervical vertebrae, thereby distributing the force across the vertebral bodies and reducing the strain on the trunk and neck muscles.
 4. Replace the need for muscle forces with reaction forces. Is there a way to control your segment motion by making contact with the patient or chair? Generating force along the side of the tooth often requires rotation of the forearm. The forearm position during force generation needs to be stabilized either by muscle or reaction forces. Extraoral contact points with the patient provide a steady fulcrum for rotation as well as reaction forces for stabilization of forearm motion especially during these periods of high force generation at the instrument/tooth interface (Figure 5). Likewise, contact between the body and the chair may provide assistance in maintaining arm and trunk alignment.
4. Replace the need for muscle forces with reaction forces. Is there a way to control your segment motion by making contact with the patient or chair? Generating force along the side of the tooth often requires rotation of the forearm. The forearm position during force generation needs to be stabilized either by muscle or reaction forces. Extraoral contact points with the patient provide a steady fulcrum for rotation as well as reaction forces for stabilization of forearm motion especially during these periods of high force generation at the instrument/tooth interface (Figure 5). Likewise, contact between the body and the chair may provide assistance in maintaining arm and trunk alignment.
5. Add sources of force by using other sources like the other hand. Can the other hand be used to supplement the force needed for the periodontal task? Traditional scaling techniques can be modified by adding reinforcement with the other hand (Figure 6). Using other body parts as sources of forces redistributes load among other components of the musculoskeletal system, as a result reducing the load in any one region.

SELF-EVALUATION
Take a look at how you position yourself in your work environment. Videotape yourself during the course of the working day. How do your body positions change with different periodontal tasks, patients, over time? While observing your posture and movements, ask yourself the following questions:
Am I working in my regions of strength? Am I working in a position favorable for generating force, eg, instrument/tooth interface low relative to your body? Have I reduced the moment arm of the reaction force applied at the instrument/tooth interface? Do my visual and scaling instruments allow me to maintain alignment with gravity? Are my joints (shoulders, elbow, and wrist) in mid-range? Am I using contact points with the patient as a fulcrum or to stabilize segment motion? Are there other sources of force, eg, other hand, that will allow me to better distribute load within my musculoskeletal system?
In summary, put yourself in a position of strength, reduce the need for muscle forces, and prepare your body for the mechanical demands imposed by periodontal tasks you face on a regular basis.
Acknowledgements: Thank you to Anna Pattison, RDH, MS; Peggy Tsutsui, RDH, MS; Becky Thaler-Tobin, RDH, BS; Erick Heygood; Roongtiwa Vachalatithi, PhD, PT; and the research assistants in the Biomechanics Research Laboratory at USC. This work was funded in part by USC Women in Science & Engineering and Intel.
REFERENCES
- Stock SR. Workplace ergonomic factors and the development of musculoskeletal disorders of the neck and upper limbs: a meta-analysis. Am J Ind Med. 1991;19:87-107.
- Akesson I, Hansson GA, Balogh I, Moritz U, Skerfving S. Quantifying work load in neck, shoulders and wrists in female dentists. Int Arch Occup Environ Health. 1997;69:461-474.
- Loslever P, Ranaivosoa A. Biomechanical and epidemiological investigation of carpal tunnel syndrome at workplaces with high risk factors. Ergonomics. 1993;36:537-555.
- Viikari-Juntura E, Silverstein B. Role of physical load factors in carpal tunnel syndrome. Scand J Work Environ Health. 1999;25:163-185.
- Rucker LM, Sunell S. Ergonomic risk factors associated with clinical dentistry. J Calif Dent Assoc. 2002;30:139-148.
- Szymanska, J. (2002). Disorders of the musculoskeletal system among dentists from the aspect of ergonomics and prophylaxis. Ann Agric Environ Med. 2002;9:169-173.
- Marklin RW, Cherney K. Working postures of dentists and dental hygienists. J Calif Dent Assoc. 2005;33:133-136.
- Michalak-Turcotte, C. Controlling dental hygiene work-related musculoskeletal disorders: the ergonomic process. J Dent Hyg. 2000;74:41-48.
- Smith CA, Sommerich CM, Mirka GA, George MC. An investigation of ergonomic interventions in dental hygiene work. Appl Ergon. 2002;33:175-184.
- Winter DA. Biomechanics and Motor Control of Human Movement . Hoboken, NJ: John Wiley & Sons Inc; 2005.
- Landsmeer JM. The metacarpophalangeal joints and the insertion of the interosseous muscles. Ned Tijdschr Geneeskd . 1955;99:2689-2690.
- Johanson ME, Valero-Cuevas FJ, Hentz VR. Activation patterns of the thumb muscles during stable and unstable pinch tasks. J Hand Surg. 2001;26:698-705.
- Dong H, Barr A, Loomer P, Rempel D. The effects of finger rest positions on hand muscle load and pinch force in simulated dental hygiene work. J Dent Educ. 2005;69:453-460.
- Jonsson, B. Measurement and evaluation of local muscular strain in the shoulder during constrained work. J Hum Ergol. 1982;11:73-88.
- Lungbord G. Nerve Injury and Repair. Edinburgh, Scotland; Churchill Livingstone; 1988:102-124.
- Oberg T, Karsznia A, Sandsjo L, Kadefors R. Work load, fatigue, and pause patterns in clinical dental hygiene. J Dent Hyg. 1995;69:223-229.
- Li G, Haslegrave CM. Seated work postures for manual, visual and combined tasks. Ergonomics. 1999;42:1060-1086.
- Lieber RL, Friden J. Musculoskeletal balance of the human wrist elucidated using intraoperative laser diffraction. J Electromyogr Kinesiol. 1998;8:93-100.
- Loren GJ, Shoemaker SD, Burkholder TJ, Jacobson MD, Friden J, Lieber RL. Human wrist motors: biomechanical design and application to tendon transfers. J Biomech. 1996;29:331-342.
From Dimensions of Dental Hygiene. March 2006;4(3): 18-21.

