Reduce Radiation Risk
What the updated American Dental Association recommendations say about patient selection in dental radiography.
This course was published in the April 2013 issue and expires April 2016. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the guidelines for patient selection in dental radiography.
- Identify agencies involved in establishing recommendations for radiation safety.
- List criteria used when determining patient selection for dental radiographic examination.
Ionizing radiation is used for medical and dental diagnosis when pathology is not clinically apparent. Radiographs have an additional role in treatment planning, monitoring disease progression, and assessing treatment efficacy. However, an integral risk in radiology is exposure of patients and, potentially, clinical staff to ionizing radiation. No exposure to X-rays can be considered completely free of risk. The effects of radiation are accumulative, so repeated exposure over one’s lifetime can add to the risks from radiation. As such, the use of ionizing radiation in dental offices is accompanied by a responsibility to limit exposures and to ensure appropriate protections.1
Children are more radiosensitive than adults and may be at increased risk of thyroid cancer due to ionizing radiation.2 Compared to medical imaging, dentists may use dental X-rays more often on children and young adults,3,4 so the need for judicious use is paramount. The biologic effects of ionizing radiation are well known, which has led government agencies to develop guidelines to protect patients and practitioners from unnecessary exposure.2,3 The decision to prescribe dental radiographs should be made by a dentist, not other members of the dental office staff.3,4 Dentists should use professional judgment, in conjunction with these guidelines, when deciding on the appropriate use of diagnostic imaging. The American Dental Association (ADA) Council on Scientific Affairs (CSA), in collaboration with the United States Food and Drug Administration (FDA) published updated guidelines ‘Dental Radiographic Examinations: Recommendations for Patient Selection and Limiting Radiation Exposure’ in December 2012.4 The recommendations were peer-reviewed by multiple dental and nondental professional groups.4
PREVIOUS GUIDELINES
In 2003, the National Council on Radiation Protection and Measurements updated its recommendations on radiation protection in dentistry,2 and in 2004, the FDA, in collaboration with the ADA, updated selection criteria for dental radiographs.3 The newest version, 2012’s ‘Recommendations for Patient Selection and Limiting Radiation Exposure’ is not meant to serve as a standard of care but rather to assist the dentist in proper selection of patients to receive ionizing radiation.4 Dentists are encouraged to consider individual patient risk and medical history, rather than using a ‘one-size fits all’ regimen for deciding when to take dental radiographs.5
One of the main purposes for defining criteria for patient selection is to reduce unnecessary patient exposure from dental radiographs. The ‘as low as reasonably achievable’ (ALARA) principle should always be followed to minimize radiation exposure.4 In 2007, the International Commission on Radiological Protection (ICRP) revised estimates of the radio sensitivity of tissues, including those in the maxillofacial region.6 Ludlow et al conducted a study to reassess human risk related to common dental radiographic exposures.
Results demonstrated that the 1990 ICRP dose estimates were 32% to 42% lower than the doses that used the 2007 ICRP guidelines.7 This means that the radiation dose in the head and neck area was higher than formerly thought, and that the 1990 dose estimates underestimated (by 32% to 42%) the real radio sensitivity in the head and neck region. Ludlow et al stressed the need for dental practitioners to reduce ionizing radiation doses substantially by using digital receptors or F-speed film instead of D-speed film, rectangular collimation instead of round collimation, and implementing reasonable radiographic selection criteria.7 The ICRP guidelines suggest that practitioners consider how the exposure will benefit their patients and whether the necessary information can be obtained in ways that do not include radiation exposure.
SUMMARY OF ADA CSA RECOMMENDATIONS
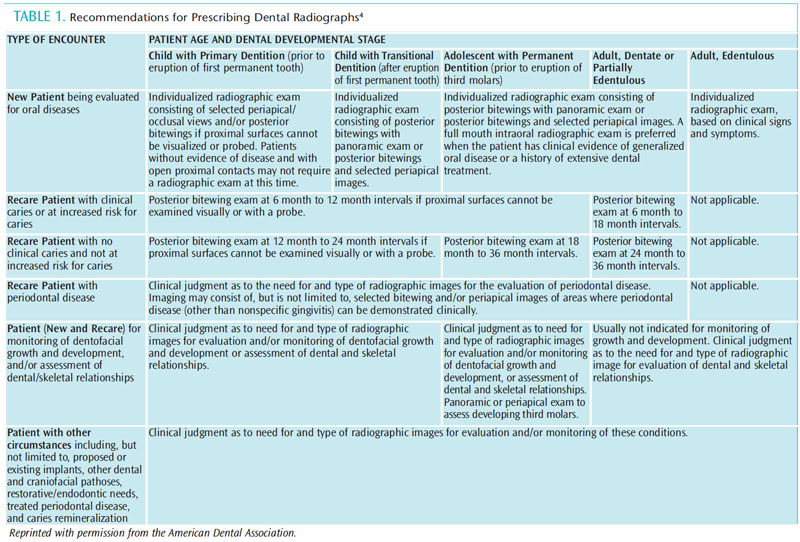
The ADA CSA ‘Recommendations for Patient Selection and Limiting Radiation Exposure’ are categorized by the types of patient encounters: new patient being evaluated for oral disease; recare patient with caries or who is at risk of caries; recare patient with no caries and is at no increased risk of caries; recare patient with periodontal disease; recare patient who needs monitoring of dentofacial growth and development and/or assessment of dental or skeletal relationships; and patients with special circumstances, such as implants, other pathology, endodontic needs, etc.4 The age and dental developmental stage of children, adolescents, adults, and edentulous individuals have specific recommendations, based on these encounter categories (Table 1). Although the guidelines state that radiographs should not be based on time alone, intervals between 6 months and 3 years are suggested for specific clinical situations. The table of recommendations is subject to clinical judgment and may not apply to every patient, as the decision to prescribe X-rays should be made by dentists only after reviewing the health history and completing a clinical examination.
SAFE PRACTICES
The ADA CSA recommendations also stress that safe practices should be used for dental patients and dental staff to reduce unnecessary exposure to ionizing radiation. Dentists are advised to ‘weigh the benefits of dental radiographs against the consequences of increasing the patient’s exposure to radiation, the effects of which accumulate from multiple sources over time.’4
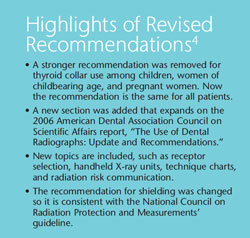
Implementation of safe practices includes selecting patients based on the chief complaint and after a clinical exam indicates need. In addition to the use of protective lead apron, a thyroid collar is also recommended for all patients. Aprons and collars must be stored properly so effective protection is not compromised. Other safety issues include selecting high speed radiographic film (F-speed) which, along with using digital equipment for radiography, can reduce patient radiation exposure by up to 60%, compared to D-speed film.8 A radiographic film manufacturer recently reported that D-speed film still accounts for 70% of US sales.9 Radiation dose can also be lowered using rectangular collimation and beam filtration. Additional exposure from retaking films is reduced by using film holder devices. Occupational exposure can be decreased by standing behind lead-lined screens and refraining from holding the X-ray film in the patient’s mouth during exposure. The document also includes safety procedures for handheld radiographic devices, which are relatively new to the market.4
There is little evidence to support radiographic exposure of all areas of the oral cavity in search of occult pathoses in the asymptomatic patient.10–12 Studies show that basing selection criteria on clinical evaluations for asymptomatic patients, combined with taking selected periapical radiographs for symptomatic patients, can result in a 43% reduction in the number of radiographs exposed without increasing the rate of undiagnosed disease.13,14 Patient selection should be based on caries risk, periodontal status, stage of growth and development, and other circumstances. Dentists should not prescribe routine dental radiographs at preset intervals (ie, every 6 months, every year) for all patients.2,4
QUALITY ASSURANCE AND PROPER TECHNIQUE
Although a large number of dental radiographs are exposed within primary dental care, a large proportion of these films exhibit poor image quality.15–17 One study reported that 42% of dental practitioners in the United Kingdom practice routine screening of new adult patients using panoramic radiography without any clinical findings to support such a radiographic examination.15 Of these screening panoramic films, when the yield from posterior bitewing and the radiological findings of no relevance to treatment were excluded, 57% of patients received no benefit from the panoramic films.
Film faults are not confined to panoramic radiography. A recent study reported levels of unacceptable intraoral films ranging from 45.2% to 56.4%.16 A study by the US government estimated that the elimination of ‘nonproductive’ examinations could lead to the reduction of the collective population dose from medical radiography by 30%.17
EDUCATION ON RADIATION SAFETY
The new ADA CSA recommendations discuss the need for dental staff who take radiographs to receive continuing education on the subject.4 Education should include proper technique to minimize retaking of films, thereby reducing radiation exposure to patients. Other topics should include safe practices when exposing radiographs in the dental office.
When children need radiographic imaging, the FDA advises parents to ask questions regarding the safety of equipment, credentials of personnel exposing the child to ionizing radiation, and if there are other procedures not involving ionizing radiation that could provide the information needed to assist in the diagnosis.18 The FDA has promoted education for parents and health care professionals regarding special precautions required for children undergoing radiological imaging through a resource called Image Gently (www.pedrad.org). This group is part of the Alliance for Radiation Safety in Pediatric Imaging, which strives to raise awareness about the opportunities to lower radiation dose in the imaging of children through educating each member of the health care/dental team.
CONCLUSION
Radiographs are used to assist the dental practitioner in the evaluation and diagnosis of oral conditions that cannot be viewed clinically. However, dental imaging does add to patients’ cumulative exposure to ionizing radiation. For this reason, radiographic guidelines for appropriate selection of patients and recommendations to limit radiation exposure have been proposed. Dental radiographs should never be taken according to preset time intervals. The decision to expose the patient to ionizing radiation should be made based on a clinical exam, consideration of caries risk, and review of the chief complaint and health history. Radiographs should not be used as a screening tool on asymptomatic patients. When the decision has been made that radiographs are necessary the number and location should be selected carefully. The dentist should use the radiographic examination with the lowest dose options needed for diagnostic needs.
In addition, a quality assurance protocol is recommended to ensure safe radiographic practices and a safe environment. Thyroid collars should be used during intraoral radiography, particularly for individuals younger than 20. Rectangular collimation reduces exposure by 50% compared to round collimation. Use of digital imaging or E/F-speed film also reduces patient exposure. Dental professionals exposing radiographs need to remain up to date on best practices through continuing education. Under the ADA CSA 2012 guidelines, dentists should decide which patients need dental X-rays and what radiographs are needed. This comes with a responsibility to follow the ALARA principle to minimize radiation exposure to patients.
REFERENCES
-
- Frommer HH. Radiology for Dental Auxiliaries.7th ed. St. Louis: Mosby; 2001:59–77,279–284.
- National Council for Radiation Protection and Measurements. Report No 145—Radiation Protection in Dentistry. Bethesda, Md: National Council on Radiation Protection and Measurements; 2003.
- American Dental Association Council on Dental Benefit Programs, US Department of Health & Human Services, Food and Drug Administration. The selection of patients fordental radiographic examinations. Available at: www.fda.gov/downloads/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures/MedicalImaging/MedicalX-Rays/ucm116505.pdf. Accessed March 4, 2013.
- Council on Scientific Affairs. American Dental Association, US Department of Health and Human Services, Food and Drug Administration. Dental radiographic examinations: Recommendations for patient selection and limiting radiation exposure. 2012. Available at: www.ada.org/sections/professionalResources/pdfs/Dental_Radiographic_Examinations_2012.pdf. Accessed March 4, 2013.
- American Dental Association. ADA updates dental radiograph recommendations. Available at: www.ada.org/news/7996.aspx. Accessed March 4, 2013.
- The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37:1–332.
- Ludlow JB, Davies-Ludlow LE, White SC. Patient risk related to common dental radiographic examinations: the impact of 2007 International Commission on Radiological Protection recommendations regarding dose calculation. J Am Dent Assoc. 2008;139:1237–1243. US Food and Drug Administration Center forDevices and Radiological Health. Dentalradiography: Doses and film speed. Available at: www.fda.gov/RadiationEmittingProducts/ RadiationSafety/NationwideEvaluationofX-RayTrendsNEXT/
ucm116524.htm. Accessed March 4, 2013. - Carestream Dental. Dental X-ray Film andRadiation Dose. 2010. Available at:www.carestreamdental.com/xraydose. Accessed March 4, 2013.
- Brooks SL. A study of selection criteria forintraoral dental radiography. Oral Surg Oral Med Oral Pathol. 1986;62:234–239.
- Brooks SL, Cho SY. Validation of a specific selection criterion for dental periapica lradiography. Oral Surg Oral Med Oral Pathol. 1993;75:383–386.
- Matteson SR, Morrison WS, Stanek EJ, PhillipsC. A survey of radiographs obtained at the initial dental examination and patient selection criteria for bitewings at recall. J Am Dent Assoc.1983;107:586–590.
- Atchison KA, White SC, Flack VF, Hewlett ER,Kinder SA. Efficacy of the FDA selection criteria for radiographic assessment of the periodontium. J Dent Res. 1995;74:1424–1432.
- Atchison KA, White SC, Flack VF, Hewlett ER.Assessing the FDA guidelines for ordering dental radiographs. J Am Dent Assoc.1995;126:1372–1383.
- Rushton VI, Horner K, Worthington HM.Aspects of the use of panoramic radiography in general dental practice. Br Dent J.1999;186:342–344.
- Helminen SE, Vehkalahti M, Wolf J,Murtomaa H. Quality evaluation of young adults radiographs in Finnish public oral health service.J Dent. 2000;28:549–555.
- Brown RF, Shaver JW, Lamel DA. Theselection of patients for x-ray examination. FDA-80-8104. Rockville, Md: Bureau of RadiologicalHealth; 1980.
- FDA Consumer Health Information.Radiology and Children: Extra Care Required.Available at www.fda.gov/downloads/ForConsumers/ConsumerUpdates/ucm048599.pdf. Accessed March 4, 2013.
From Dimensions of Dental Hygiene. April 2013; 11(4): 52, 55–57.



