 YAKUBOVALIM/ISTOCK/GETTY IMAGES PLUS
YAKUBOVALIM/ISTOCK/GETTY IMAGES PLUS
Reduce Dental Aerosols
Use of silver diamine fluoride and the atraumatic restorative technique can help minimize aerosols during dental procedures.
In early 2020, the COVID-19 pandemic negatively impacted dental care worldwide. Globally, dental offices were initially forced to close, allowing for emergency treatment only. Supply and demand chains were woefully unprepared to deal with the pandemic, further complicating the delivery of oral healthcare. With the introduction of vaccines for SARS-CoV-2,1 the United States’ economy is slowly recovering and dental practices are seeing patient visits return to pre-pandemic levels. As a result of ongoing disease, however, an emphasis on reducing viral transmission continues.
The primary known mode of transmission for COVID-19 is through respiratory droplets.2 According to the US Centers for Disease Control and Prevention, COVID-19 can be detected in saliva, but whether aerosolized saliva can infect a susceptible host is yet to be determined.3 As the pandemic continues, clinicians have sought alternate ways to minimize the risk of COVID-19 transmission in oral healthcare settings, including minimization of dental aerosols.
Oral health professionals are already familiar with some of the techniques used to eliminate or limit dental aerosol production, particularly those who engage in community service or mission work. Examples include use of silver diamine fluoride (SDF) or the atraumatic restorative technique (ART), which both help reduce exposure. Among other methods of minimizing or limiting aerosols is the use of high-volume evacuators and air management systems, such as air purifiers.
Clinicians who treat patients with special needs, older adults, and other vulnerable populations commonly employ treatment modalities that limit aerosol production.4, Minimizing or limiting aerosols is vital because medically vulnerable individuals may have other chronic conditions leading to a weak respiratory system, putting them at increased risk for respiratory infections, such as aspiration pneumonia.5 This is a condition that can be fatal in individuals with compromised respiratory issues, such as chronic obstructive pulmonary disorder, asthma, chronic bronchitis, emphysema, and lung cancer. Therefore, as a preventive dental measure, the use of SDF and ART may be beneficial for the broader population during the pandemic.

SILVER DIAMINE FLUORIDE
With an action similar to fluoride varnish,6 SDF was approved as a desensitizing agent in 2014 and as a breakthrough therapy for the treatment of dental caries in 2016 by the US Food and Drug Administration.7,8
A 2016 systematic review revealed that the application of 38% SDF in children arrested 65% of active lesions when applied at least once a year (Figure 1).9 If applied twice a year, SDF has been shown to arrest more than 90% of caries.7 As such, SDF is now used as a desensitizing agent, preventive agent, and a caries-arresting agent, either alone or in conjunction with a restoration (Table 1). While fluoride varnish is most effective in remineralization of the enamel, SDF is most effective at arresting caries of the dentin and root surfaces.10 This material is noninvasive, easy to apply, cost effective, and is safe for most patients;11 in fact, among some geriatric, pediatric and public health dentists, SDF is referred to as the “silver bullet.”12
While the majority of studies on SDF effectiveness have been done with pediatric, geriatric, and other vulnerable populations, the potential benefits of using SDF more broadly outweigh the adverse effects, namely, staining—which is a concern, especially with anterior teeth.13 The major shortcoming of SDF is that it will stain caries and plaque a dark brown-to-black color. Newer products have added potassium iodide to reduce staining issues.14 Because it is taken up by saliva, the stain may affect caries and plaque in areas that were not originally intended for treatment.15 There are no specific post-operative instructions. If reapplication is needed depending on the original diagnosis, treatment plan and prognosis, application is recommended twice per year for caries arrest and prevention.
SDF can be used to desensitize teeth/roots and prevent or arrest caries in primary and permanent teeth, whether due to early childhood caries or xerostomia.11,16,17 It is also an effective treatment option for other vulnerable patients with behavioral or medical management concerns. Use of this material allows the provider to treat more lesions in one visit, which limits access-to-care barriers for patients who have difficulties visiting a dental office.12
There are contraindications to SDF administration, including:
- Patients with an allergy to silver or other heavy metals may experience adverse effects with SDF.
- This medicament should not be used on teeth with pulpal involvement, and it is not recommended for use on teeth with large caries or exposed pulp18—although it is indicated for remineralization of tooth structure to prevent pulpal exposure.19 Similarly, it is not recommended for teeth with diagnosis of irreversible pulpitis, necrotic pulp or periapical disease.20
While there are no reported health complications for suitable patients, a reaction to the silver ingredient may be possible. As a standard of clinical care, the use of protective eyewear is recommended for the application of SDF.21 Lastly, because SDF can stain operatory surfaces, proper handling and disposal are important.
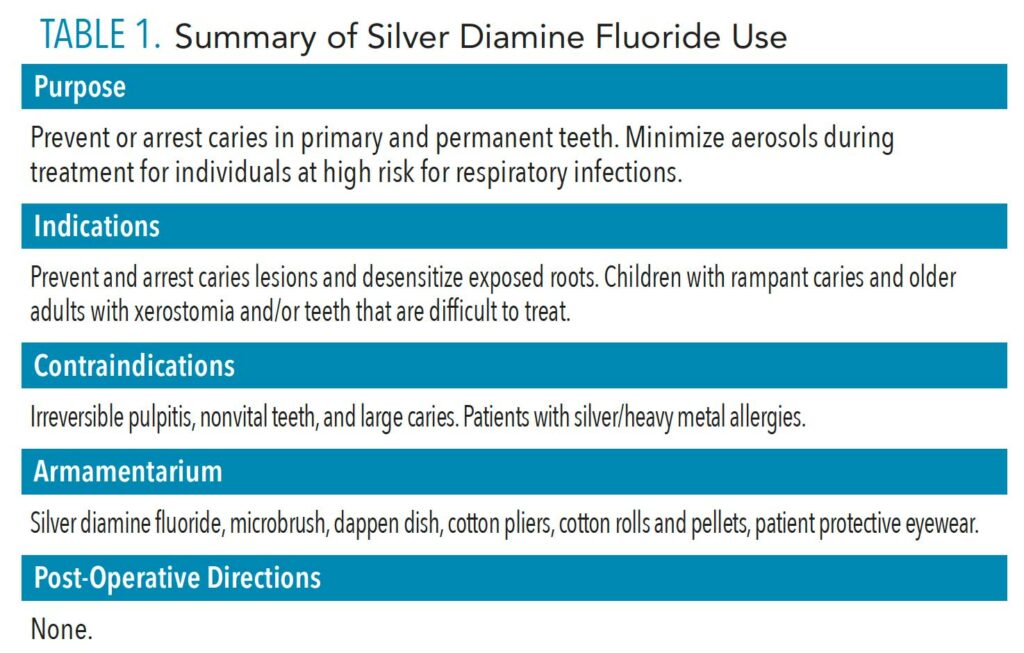
The American Dental Association’s Code on Dental Procedures and Nomenclature (CDT) lists codes that can be used to bill insurance companies for SDF application:
- D1208: Topical application of fluoride for prevention
- D9910: Topical application of desensitizing medicament for sensitivity
- D1354: Interim caries arresting medicament of fluoride varnish for treating caries/per tooth application
ATRAUMATIC RESTORATIVE TECHNIQUE
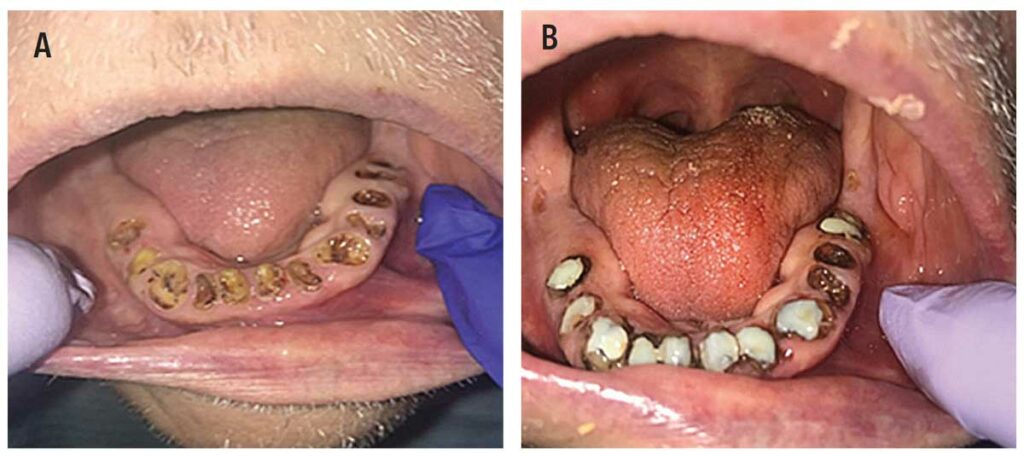
Another approach to minimize aerosol generation is using hand instruments instead of ultrasonics for restorative procedures. This delivery, known as ART, has long been employed in the public health sector and is another alternative for treating caries lesions (Figure 2A and Figure 2B). The ART approach includes preventive, minimally invasive care that prevents further development of caries, particularly in medically and socioeconomically vulnerable patients.22 In some cases, ART restorations are considered definitive restorations, while in other instances they are considered interim. The latter are often referred to as interim therapeutic restorations (ITR).
A 25-year comprehensive overview describes the ART restorative approach as precisely creating sufficient tooth or root surface access for the removal of only the soft, demineralized (decomposed) dentin with hand instrumentation.22 Caries removal is followed by restoration with an adhesive dental material;23 for example, glass ionomer is generally used in pediatric dentistry and for root caries in geriatric patients. When using SDF, cavity conditioner plays an important role.24 Simultaneously, the provider seals any remaining pits and fissures that remain at risk.25 If the lesion is excavated with rotating instruments, it is not considered ART or modified ART. This approach has spread globally; in many countries, in fact, ART is part of the dental curriculum due to conducive clinical outcomes in young children and older adults.26
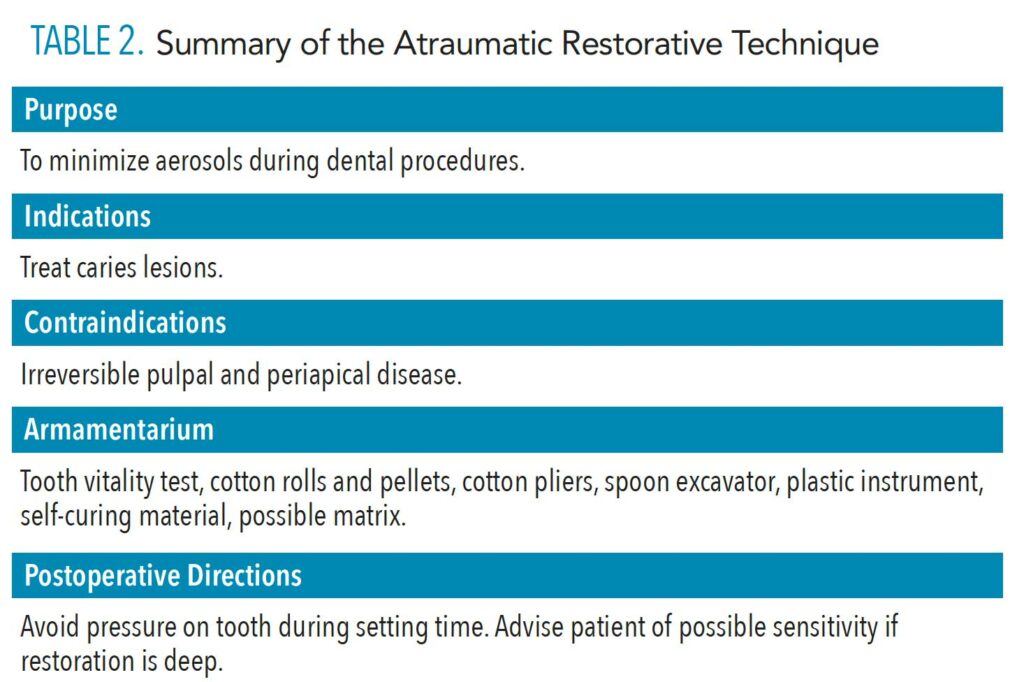
Research has found that partial caries removal was associated with a significant reduction in pulp exposure in asymptomatic teeth with deep caries.27 The intentional retention of caries within a restorative preparation is a significant paradigm in caries management, and the level and quality of evidence are compelling. Partial caries removal with ART minimizes trauma to the tooth. This technique typically does not involve local anesthetic or a handpiece, and there is minimal chance of unintended pulpal exposure.28 There are no medical contraindications to the ART approach or partial caries removal techniques, although patients with an allergy to the dental materials used for the restoration should be excluded (Table 2). Post-operatively, patients should be advised to avoid putting pressure on the restored tooth for the duration of the final setting time. If the restoration was deep and postoperative sensitivity is anticipated, advise the patient accordingly. This approach is not recommended for use on teeth with a diagnosis of irreversible pulpitis, necrotic pulp, or periapical disease. Also, patients with cognitive decline or management issues may not be suitable for this technique.
The CDT code used for billing will depend on the diagnosis and rationale for use of ART or ITR:
- D2941: Interim therapeutic restoration: primary dentition
- D2940: Protective restoration
- Codes for definitive resin restorations of primary or permanent teeth
CONCLUSION
The COVID-19 pandemic forced oral health professionals to pursue alternative methods to ensure patient and operator safety. Minimizing dental aerosols which may contain SARS-CoV-2 is a strategy that is easily implemented by using SDF and ART. The ART approach helps minimize aerosol production, while application of SDF minimizes the need to use a dental handpiece. Oral health professionals may offer a great service to patients at elevated risk of developing caries due to other conditions or medications by providing care utilizing alternative, aerosol-reducing clinical techniques.
REFERENCES
- United States. Food and Drug Administration. COVID-19 Vaccines. Available at: fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines. Accessed June 13, 2021.
- World Health Organization. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. Available at: who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed June 13, 2021.
- Santosh TS, Parmar R, Anand H, Srikanth K, Saritha M. A review of salivary diagnostics and its potential implication in detection of COVID-19. Cureus. 2020:12:e7708.
- United States Department of Labor Occupational Safety and Health Administration. Dentistry Workers and Employers. Available at: osha.gov/SLTC/covid-19/dentistry.html. Accessed June 13, 2021.
- Mandell LA, Niederman MS. Aspiration pneumonia. N Eng J Med. 2019;380:651–663.
- Möhler JS, Sim W, Blaskovich MA, Cooper MA, Ziora ZM. Silver bullets: a new lustre on an old antimicrobial agent. Biotechnol Adv. 2018;36:1391–1411.
- Horst JA. Silver fluoride as a treatment for dental caries. Adv Dent Res. 2018;29:135–140.
- United States Food and Drug Administration. Breakthrough Therapy. Available at: fda.gov/patients/fast-track-breakthrough-therapy-accelerated-approval-priority-review/breakthrough-therapy. Accessed June 13, 2021.
- Crystal YO, Niederman R. Silver diamine fluoride treatment considerations in children’s caries management. Pediatr Dent. 2016;38:466–471.
- Gao SS, Zhang S, Mei ML, Lo EC, Chu CH. Caries remineralisation and arresting effect in children by professionally applied fluoride treatment—a systematic review. BMC Oral Health. 2016;16:12.
- Horst JA, Ellenikiotis H, UCSF Silver Caries Arrest Committee, Milgrom PL. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications and consent. J Calif Dent Assoc. 2016;44:16–28.
- Rosenblatt A, Stamford TC, Niederman R. Silver diamine fluoride: a caries “silver-fluoride bullet.” J Dent Res. 2019;88:116–125.
- Crystal YO, Kreider B, Raveis VH. Parental expressed concerns about silver diamine fluoride (SDF) treatment. J Clin Pediatr Dent. 2019;43:155–160.
- Patel J, Anthonappa RP, King NM. Evaluation of the staining potential of silver diamine fluoride: in vitro. Int J Paediatr Dent. July 4, 2018. Online ahead of print.
- Hosoya Y, Watanabe E, Tadokoro K, Inoue T, Miyazaki M, Tay FR. Effects of ammonium hexafluorosilicate application on demineralized enamel and dentin of primary teeth. J Oral Science. 2012;54:267–272.
- Gold J. Silver diamine fluoride arrests caries in primary teeth. J Evid Based Dent Pract. 2018;18:88–90.
- Chu CH, Lee AH, Zheng L, Mei ML, Chan GC. Arresting rampant dental caries with silver diamine fluoride in a young teenager suffering from chronic oral graft versus host disease post-bone marrow transplantation: a case report. BMC Res Notes. 2014;7:3.
- Hu S, Meyer B, Duggal M. A silver renaissance in dentistry. Eur Arch Paediatr Dent. 2018;19:221–227.
- Zhi QH, Lo EC, Lin HC. Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children. J Dent. 2012;40:962–967.
- Felemban OM, Dabroom WA, Alsharif MT, et al. The effect of silver diamine fluoride in preventing secondary caries in primary teeth: in-vitro study. EC Dental Science. 2018;17:1564–1569.
- Allred A, Moulding LR, Stewart PW. Dental patients’ perceptions and understandings towards the use of protective eyewear during dental procedures. Doctoral dissertation. Weber State University. 2016.
- Frencken JE, Leal SC, Navarro MF. Twenty-five-year atraumatic restorative treatment (ART) approach: a comprehensive overview. Clin Oral Investig. 2012;16:1337–1346.
- Perdigão J. Current perspectives on dental adhesion: (1) Dentin adhesion—not there yet. Jpn Dent Sci Rev. 2020;56:190–207.
- Mazaheri R, Pishevar L, Shichani AV, Geravandi S. Effect of different cavity conditioners on microleakage of glass ionomer cement with a high viscosity in primary teeth. Dent Res J (Isfahan). 2015;12:337–341.
- Borsatto MC, Thomaz MY, Contente MM, et al. Bonding agent underneath sealant: shear bond strength to oil-contaminated. Braz Dent J. 2010;21:50–54.
- da Mata C, Allen PF, Cronin M, O’Mahony D, McKenna G, Woods N. Cost-effectiveness of ART restorations in elderly adults: a randomized clinical trial. Community Dent Oral Epidemiol. 2014;42:79–87.
- Frencken JE. Atraumatic restorative treatment and minimal intervention dentistry. Br Dent J. 2017;223:183–189.
- Karim A, Mascarenhas AK, Dharamsi S. A global oral health course: isn’t it time? J Dent Ed. 2008;72:1238–1246.
From Dimensions of Dental Hygiene. July 2021;19(7):21-23.

