 GOPIXA / ISTOCK / GETTY IMAGES PLUS
GOPIXA / ISTOCK / GETTY IMAGES PLUS
Precision Dentistry-The Future of Oral Healthcare Delivery
This new approach bodes well for improving healthcare outcomes while also lowering costs.
This course was published in the June 2022 issue and expires June 2025. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the prevalence of oral disease in the United States.
- Define precision medicine and precision dentistry.
- Note the progress in expanding precision dentistry in the US and explain the additional steps necessary to further its implementation.
In spite of significant scientific advancements in the fields of science and medicine, the rates of oral disease in the United States (dental caries, periodontal diseases, and head and neck cancer) are staggering: 47.2% of adults ages 30 and older have some form of periodontal disease, and more than 90% of adults ages 20 and older have had at least one carious lesion.1 Dental caries is rampant in the nation’s children: 57% of adolescents between the ages of 12 and 19 have had a carious lesion in their permanent teeth.1 Head and neck cancers, however, have been steadily declining for the past 20 years.2 Additionally, the US has an access-to-care problem, with persistent oral health disparities.3,4
A paradigm shift is necessary to improve oral health outcomes in the US. Precision medicine and precision dentistry may be able to potentially shift the burden of disease and improve the nation’s oral health, thus, improving overall health.
Terminology
Precision medicine, sometimes referred to as personalized medicine, is modernizing and improving the US healthcare system. Precision medicine refers to the use of personal data and biomarkers—particularly an individual’s own genetic biomarkers—to create protocols/treatments that improve health outcomes for all (Table 1).4–6 It is a departure from the current one-size-fits-all paradigm that focuses on treating disease instead of enhancing wellness. The National Institutes of Health (NIH) defines precision medicine as “an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, and lifestyle for each person.”5 Scientists and oral healthcare advocates suggest that health can be maintained and disease avoided by creating specific interventions that consider an individual’s specific genes and biomarkers, as well as environmental factors.7
Precision dentistry is a data-driven approach that classifies patients into groups to which treatments and interventions are tailored.8,9 Precision medicine’s success depends on its ability to be predictive, preventive, personalized, and participatory.
Overlapping similarities exist between precision medicine and personalized medicine. Much like precision medicine, personalized medicine involves tailoring medical treatment to the individual characteristics of each patient. Risk assessment, prevention, early detection, and accurate diagnosis, treatment, and management are hallmarks of both personalized and precision medicine. The term “personalized medicine” seems to insinuate that drugs or medical devices are created specifically for a patient. The term “precision medicine” more accurately captures the concept as “accurate” and “precise.” Since the introduction of the Precision Medicine Initiative in 2018, the term “personalized medicine” is used less in favor of the term “precision medicine.” The literature demonstrates, however, that these terms are often used interchangeably.
America’s Precision Medicine Initiative
Demonstrating the strength of this country’s commitment to precision medicine, President Obama launched the Precision Medicine Initiative in 2015. A foundational part of this initiative is the “All of Us” study, the largest longitudinal study ever conducted in the US. It seeks to enroll 1 million Americans and examine the effects of environment, lifestyle, and biology on human health.
The 10-year study, which began in 2018, is groundbreaking for several other reasons. First, its main focus is to enroll participants who are traditionally underrepresented in health research: ethnic minorities, those with cognitive impairments, and medically underserved populations.5 Second, in order to fulfill its mandates, new technologies and information technology infrastructure had to be created in order to gather and analyze the data collected. Precision medicine requires the use of advanced technology (hardware) and concepts, such as knowledge discovery, data mining (algorithms that find patterns in the information), and natural language processing (analyzing free-form text entered into electronic health records (EHRs) and discovering patterns in the data).4 Third, participants are required to play an active role in the study by contributing data freely (including DNA samples and other biologic specimens), agreeing to ongoing accessibility of their EHRs, sharing results of clinical and behavioral assessments, and participating in mobile health activities to collect geospatial and environmental data.5 Such participation requires researchers to gain patients’ trust and cooperation in order to meet the study’s goals.
Some challenges to the “All of Us” study include ensuring participants’ privacy, and addressing concerns regarding exacerbation of health disparities due to availability of technology. Historically, individuals of low socioeconomic status have not benefitted from technological advances as much as those with higher socioeconomic status.4
One of the key challenges that researchers must successfully mitigate is the lack of data on minority populations. Unless data are gathered on these populations, the genetic technologies available will be implemented in ways that perpetuate and even widen health disparities. The effectiveness of genomic therapies relies on the availability of genetic data. As the diversity of the American population is so vast, data on all groups are necessary to create effective treatments. Currently, people of non-European ancestry are underrepresented in the genetic databases on which researchers base their studies. In 2021, “Oral Health in America: Advances and Challenges” was released by the NIH, providing updates on the findings of the 2000 report “Oral Health in America: A Report of the Surgeon General.” The report notes that oral health inequity remains 20 years later and key areas of research should be identified in order to improve the oral health of all Americans.10 Section 6 of the report, “Emerging Science and Promising Technologies to Transform Oral Health,” reviews the exciting findings made possible by technology, such as web-based human oral microbiome databases (Human Oral Microbiome Database, CORE database), ability to conduct clinically relevant studies by identifying new species, biomaterials, nanotechnology, and periodontal regenerative medicine. New approaches based on these advances, however, must be well planned, based on scientific evidence, and equitable.10 Active recruitment for the “All of Us” study is ongoing, and researchers are seeking to enroll minority populations. For more information and to participate, visit: joinallofus.org.
Precision dentistry in action
The ZOE 2.0 study is a large-scale, genetic epidemiologic study of early childhood caries conducted among a community-based sample of preschool-age children enrolled in Head Start centers in North Carolina. This NIH- funded study was conducted in phases with data collection occurring from August 2016 to February 2019. Recognizing the need for high fidelity, large-scale information to support precision medicine approaches, the researchers identified six major building blocks necessary to further precision dentistry:11
- Phenotype definition and measurements
- Accounting for and operationalization of proximal and distal influences
- Leveraging big data
- Development and utilization of health and disease biomarkers
- Training of precision health-minded oral health professionals
- Advocacy for investments in science, technology, education, and policy change
Administrative data (public health insurance claims, EHRs); caregiver reports (child oral health status, diet, dental attendance, medications, etc); clinical measures (caries experience as measured by International Caries Detection and Assessment System, occlusion, dental trauma, behavior/cooperation); genome (including microbiome); family history and demographics (age, race/ethnicity, education, caregiver health status, caregiver oral health status); imaging; environmental exposures (fluoride); and geography/community characteristics will all be collected.11
Fisher-Owens Framework
One of the challenges to applying precision medicine is the lack of large-scale, valid studies from which to create models. Several reasons account for this issue, including the lack of research methodologies that balance bias and variance. The University of California, San Francisco, has developed the Fisher-Owens framework to conceptualize child, family, and community influences on children’s oral health outcomes. Researchers sought to create a framework that would reduce confounding, a major concern when comparison groups are not randomized. Comparable dental patient groups were successfully created through the process of evaluating the need for and feasibility of matching, considering different matching methods, and evaluating matching quality.12 The Fisher-Owens framework illustrates the complexity of precision medicine and the necessity for valid, reliable data from which to build multifactorial, multilevel conceptual frameworks.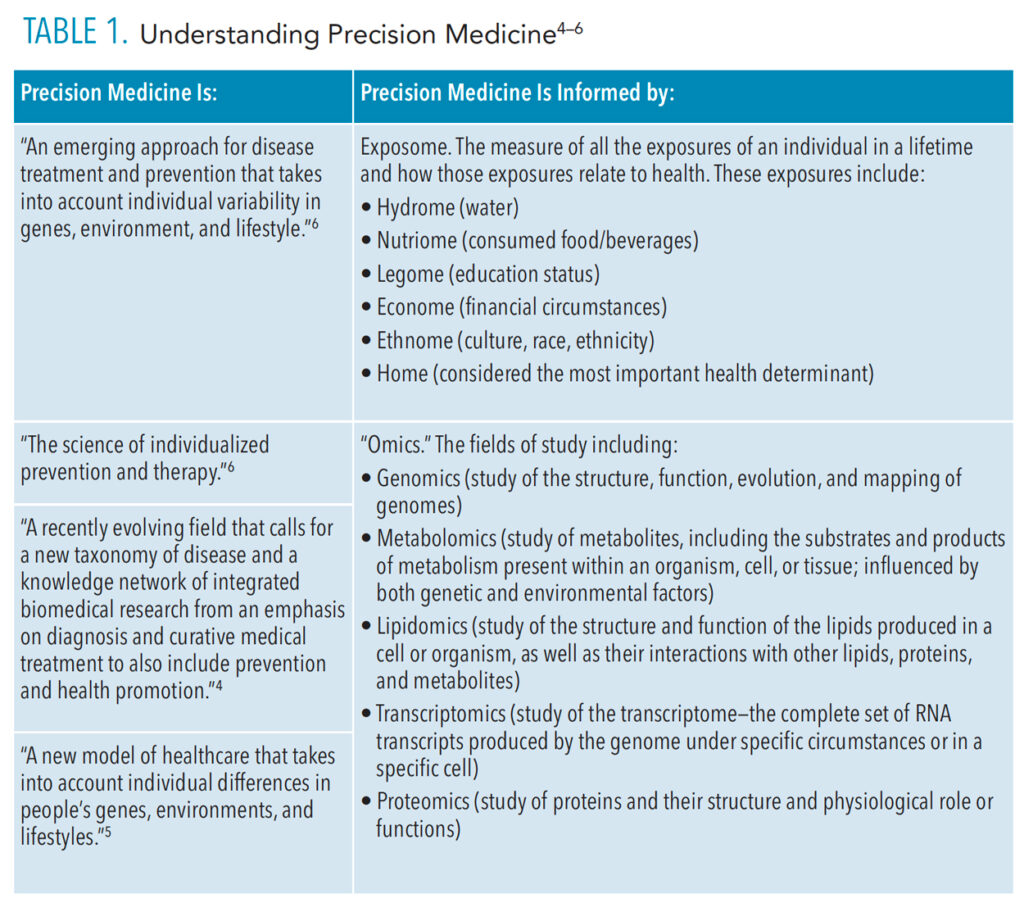
Periodontal Diseases
Precision dentistry is key to periodontics as periodontitis results from a highly individualized sequence of events derived from both genetic and environmental factors. The bacterial biofilm present in periodontitis induces an inflammatory host response, which is influenced by environmental, genetic, and epigenetic factors. Epigenetic and environmental factors alter gene expressions not encoded in the DNA sequence. These alterations cause a remodeling of the chromatin and activate or inactivate genes. Smoking, for example, is a powerful epigenetic factor (primarily via DNA methylation). Genome-wide association studies have identified variants in at least 65 genes involved in periodontal disease initiation/progression. Additionally, researchers have discovered four shared genetic loci between periodontal diseases and atherosclerotic cardiovascular diseases (CDKN2B‐AS1, VAMP3, VAMP8, PLG).13 This suggests that periodontitis and atherosclerotic diseases are not only causally linked, but also share a similar inflammatory track.13
In support of these scientific advancements, the American Academy of Periodontology and the European Federation of Periodontology introduced a new model of periodontal disease classification (the World Workshop Model) in 2017. Four stages indicate the severity of disease (previously classified as mild, moderate, or severe) and complexity of case management. The grading refers to the progression of disease and depends on biological factors such as predicted rate of progression, person-level risk factors, and potential health threats.9
The Periodontal Profile Class Model, also introduced in 2017, utilizes a latent class analysis classification model. The hallmark of this analysis is the use of data-driven multidimensional disease patterns as opposed to traditional disease classification (eg, mild, moderate, and severe, which only classify disease state and does nothing to prevent disease). The Periodontal Profile Class Model lists seven types of periodontal statuses and includes such factors as teeth that are healthy or have recession, presence of crowns, high gingival index, and a reduced periodontium.9,13,14
In a systematic review by Baima et al,15 more than 40 metabolites were found in periodontitis sites. These included malondialdehyde, generated by the peroxidation of membrane polyunsaturated fatty acid and a biomarker for oxidative stress, and 8-hydroxy-deoxyguanosine, a measurement of endogenous oxidative DNA damage and a risk factor for many diseases including cancer.
Big Data
The absence of evidence-based clinical practice guidelines, integration of massive data sets, and adoption of new knowledge as standard of care are three major challenges to the full implementation of precision dentistry.7 The Institute of Medicine has introduced the Learning Healthcare System, which aligns “science, informatics, incentives, and culture” in order to improve current health care delivery via the use of big data.7 The aggregation of that data is currently being done in the US by:
- Big Mouth: EHRs of eight dental schools, more than 1.2 million oral health records
- Consortium for Oral Health-Related Informatics: includes more than 20 dental schools
- National Practice-Based Research Network: sponsored by the National Institute of Dental and Craniofacial Research, it consists of practicing oral health professionals and academicians
The data from clinical trials are also adding to big data repositories. These massive amounts of data are analyzed in four domains: sociobehavioral, educational, clinical, and translational science. The end goal is to recognize clinical disease phenotypes and create guidelines to effectively treat them.
Personalized Medicine in Dental Education
Previous educational paradigms will not facilitate the expansion of precision dentistry. Successful implementation of precision medicine requires changes in practice patterns and management strategies for oral health professionals. Zheng et al6 studied the development of personalized medicine/personalized dentistry in the curricula of North American dental schools from 2014 to 2017 and discovered that while the majority of respondents felt that personalized medicine/personalized dentistry should be taught in the curriculum (as it would impact clinical practice in the future), most had yet to include medicine/personalized dentistry in their didactic curricula. Additionally, the researchers discovered that when medicine/personalized dentistry was included in the curricula, it was done as nongenetics-based diagnostics (eg, caries risk assessment) as opposed to genetics-based diagnostics (eg, salivary diagnostics). To date, no studies on the application of precision dentistry in dental hygiene programs have been published.
Conclusion
Precision medicine holds promise for improving health care while also lowering costs. It relies on EHRs, genetic and molecular data, big data analytics, supercomputing, and the social determinants of health in conjunction with the collaboration of clinicians, researchers, bioinformaticians, data scientists, and, most important, patients. Successful implementation of precision dentistry requires training of “precise-minded” practitioners.13 Precision medicine/precision dentistry concepts and frameworks must be added to the curricula of dental and allied dental schools. Currently, little scientific research is available to support the use of precision dentistry in clinical practice.13 Genomics in oral health is in its infancy and more genome-wide association studies must be conducted in order for precision dentistry to become the standard of care.
References
- United States Centers for Disease Control and Prevention. Oral Health: Cavities. Available at: cdc.gov/oralhealth/fast-facts/cavities/index.html. Accessed May 18, 2022.
- American Cancer Society. Key Statistics for Oral Cavity and Oropharyngeal Cancers. Available at: cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html. Accessed May 18, 2022.
- Slavkin HC. From high-definition precision healthcare to precision public oral health: opportunities and challenges. J Public Health Dent. 2020;80:S23–S30.
- Gansky SA, Shafik S. At the crossroads of oral health inequities and precision public health. J Public Health Dent. 2020;80:S14–S22.
- Sankar PL, Parker LS. The Precision Medicine Initiative’s All of Us Research Program: an agenda for research on its ethical, legal, and social issues. Genet Med. 2017;19:743–750.
- Zheng LY, Rifkin BR, Spielman AI, London L, London SD. The teaching of personalized dentistry in North American dental schools: changes from 2014 to 2017. J Dent Educ. 2019;83:1065–1075.
- Finkelstein J, Zhang F, Levitin SA, Cappelli D. Using big data to promote precision oral health in the context of a learning healthcare system. J Public Health Dent. 2020;80:S43–S58.
- Bartold PM. Personalized/precision dentistry–the future of dentistry? Aust Dent J. 2017;62:257.
- Beck JD, Philips K, Moss K, Divaris K, Morelli T, Offenbacher S. Advances in precision oral health. Periodontol 2000. 2020;82:268–285.
- Oral Health in America: Advances and Challenges. Bethesda, Maryland: United States Department of Health and Human Services, National Institutes of Health, National Institute of Dental and Craniofacial Research; December 2021.
- Divaris K, Joshi A. The building blocks of precision oral health in early childhood: the ZOE 2.0 study. J Public Health Dent. 2020;80:S31–S36.
- Fisher-Owens SA, Gansky SA, Platt LJ, et al. Influences on children’s oral health: a conceptual model. Pediatrics. 2007;120:e510–e520.
- Divaris K, Moss K, Beck JD. Biologically informed stratification of periodontal disease holds the key to achieving precision oral health. J Periodontol. 2020;91:S50–S55.
- Loos BG, Van Dyke TE. The role of inflammation and genetics in periodontal disease. Periodontol 2000. 2020;83:26–39.
- Baima G, Corana M, Iaderosa G, et al. Metabolomics of gingival crevicular fluid to identify biomarkers for periodontitis: a systematic review with meta‐analysis. J Periodontal Res. 2021;56:633–645.
From Dimensions of Dental Hygiene. June 2022; 20(6)34-37.



