Minimize the Risk of Infection
Minimize the risk of infection by adhering to evidence based infection control protocols, oral health professionals can reduce the risk of disease transmission in the dental office.
Both clinicians and patients may be exposed to potentially infectious pathogens in the dental operatory. Contact with blood and saliva, as well as contaminated surfaces, increases the risk of transmission of infectious diseases, including hepatitis B, hepatitis C, human immunodeficiency virus (HIV), tuberculosis (TB), methicillin-resistant Staphylococcus aureus, the common cold, influenza, and herpes viruses.1 Contact with a pathogen alone will not produce infection. Rather, several factors play a role in disease transmission, including host response, number and virulence of pathogens, and mode of transmission.2 Contaminated dental surfaces and contagious oral health professionals may be reservoirs for communicable diseases. To prevent transmission of potentially infectious pathogens, oral health professionals must adopt and adhere to stringent infection control protocol and use standard precautions during the treatment of all patients.
HEPATITIS
Oral health professionals are at increased risk of acquiring hepatitis B (Figure 1) and hepatitis C (Figure 2) through occupational exposure. According to 2010 data from the United States Centers for Disease Control and Prevention (CDC), the number of individuals in the US living with chronic hepatitis B and hepatitis C infections was between 800,000 and 1.4 million, and 2.7 million and 3.9 million, respectively.3 The actual number of these cases may be higher than documented, because most states do not report their hepatitis statistics to the CDC.4
Oral health professionals are at greater risk of becoming chronic hepatitis B carriers than the general population.5 due to the virus’ ability to survive at room temperature in dried blood for days.2 Transmission of hepatitis B occurs through contact with infectious blood, saliva, and all bodily fluids; sexual contact; perinatal transport; and sharing contaminated needles or other drug-injection objects. The hepatitis B vaccine is recommended for people of all ages. Hepatitis C is transmitted by contact with infectious blood, exposure to contaminated needles, and needle stick injuries. There is no vaccination for hepatitis C.4
TUBERCULOSIS
TB (Figure 3) is transmitted through the air in droplet nuclei when a person with an active infection coughs, talks, sings, or sneezes. The number of reported TB cases has declined over the past 20 years, with 9,951 new cases reported stateside in 2011. Cases were spread across the US, with California, Texas, New York, and Florida each reporting more than 500 cases.6
TB transmission is possible when rendering or receiving dental services. Following standard precautions is not sufficient in preventing the transmission of TB; therefore, dental offices should develop TB infection-control policy based on community risk assessments from the local health department.7 According to the CDC Guidelines for Infection Control in Dental Health-Care Settings—2003, dental offices that deliver care to patients with TB should inquire about a personal history of TB; refer patients with suspected TB for medical evaluation; provide dental services to individuals with TB in an isolated room; instruct patients with TB to wear a surgical mask between services; defer elective dental services until confirmation of cleared infection; and provide urgent dental care in a hospital setting with airborne infection isolation. Oral health professionals should have a baseline TB skin test upon hire, with subsequent testing performed according to the practice’s risk of TB infection. Staff should be evaluated if a persistent cough develops in presence of other active TB signs and symptoms—returning to work only when cleared of TB infection by a physician.7
The TB vaccination, Bacille Calmette-Guérin, is not commonly used in the US, but rather is administered to infants and young children in countries where TB is prevalent. Unfortunately, the vaccine is not 100% effective against TB.8
HUMAN IMMUNODEFICIENCY VIRUS
The life expectancy of people with HIV (Figure 4) is rising due to significant advances in medical management that have occurred over the past 25 years. Approximately 50,000 individuals become infected with HIV each year. In 2008, it was estimated that 679,590 adolescents and adults in the US were infected with the virus.9 Special procedures are not needed to prevent transmission of HIV, as every dental office must follow standard precautions with all patients, regardless of health status, to prevent the spread of infection.10
MICROORGANISMS IN DENTAL UNIT WATERLINES
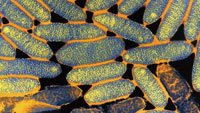
The dental unit waterline (DUWL) connects to the municipal water system through a long, narrow tube—making it the ideal habitat for biofilm growth.11 Bacteria, fungi, protozoa,.12 and living amoebae have been found in DUWLs.12 Opportunistic pathogens, such as Legionella pneumophila (Figure 5) and Pseudomona aeruginosa (Figure 6), have also been detected in DUWLs.11,13 The risk of microorganisms in DUWLs causing disease is low for healthy patients, but immunocompromised patients are at increased risk of infection transmission.11,13,14
In 2012, Dogruoz et al demonstrated the contamination of DUWLs with microorganisms.11 Water samples from 123 air-water syringes, high-speed drills, and water sources from 41 dental units were investigated for aerobic heterotrophic bacteria and sulphate-reducing bacteria. Out of the 123 samples taken, 113 failed to meet the American Dental Association standard of less than 500 colony-forming units per milliliter of water.11 Heterotrophic bacterial levels were found to be significantly higher in air-water syringes, high-speed drills, and water sources. Sulphate-reducing bacteria were detected in 102 of the samples, and in all air-water syringes and high-speed drills. Free-living amoebae were detected in 103 of the samples. The age of the dental unit did not affect the counts of heterotrophic bacteria and sulphate reducing bacteria. Biofilm accumulation and absence of DUWL disinfection systems were blamed for the presence of anaerobic bacteria, which hosts sulphate-reducing bacteria. The presence of sulphate reducing bacteria, particularly hydrogen sulfide, has been linked to increased risk of periodontitis.11
Oral evacuation systems may also pose an infection control risk because pathogens can be introduced into the mouth from dental tubing as a result of backflow.15 While few adverse health effects caused by contaminated saliva ejectors have been reported, oral evacuation systems should be regularly disinfected to eliminate the proliferation of harmful bacteria, and the use of specially designed saliva ejectors that prevent backflow may be considered.16
Regardless of whether the threat of infection from exposure to high microorganism counts in DUWLs is high or low, oral health professionals are ethically bound to evaluate and properly disinfect DUWLs in order to maintain a safe environment for clinicians and patients alike.17,18
AEROSOL-CONTAINING MICROBES
Aerosols are created from many day-to-day procedures in the dental operatory. The spread of aerosols, as well as their level of contamination, is a concern in dentistry. Measured through microbial quantitative analysis, research has sought to pinpoint aerosol contaminants and determine how far-reaching they spread onto surfaces.17 Microbial counts in the air are lower prior to dental procedures compared to during and post-clinic sessions. Aerosols are most commonly produced by handpieces, ultrasonic scalers, and air polishers.19,20 Longer dental procedures generate more aerosol bacteria. Gram-positive cocci and opportunistic pathogens, such as Micrococcus, Streptococcus, and Staphylococcus, are found in higher numbers when aerosol production is great. The use of DUWLs combined with microorganisms from the patient’s oral cavity generate aerosols, creating a potentially hazardous environment for immunocompromised patients.7,21 Therefore, it may be helpful to have all patients use an antimicrobial mouthrinse prior to beginning dental treatment in order to reduce the amount of bacteria present in resultant aerosols.7
MINIMIZE RISK

In order to reduce potential infection in the dental setting, dental offices should maintain written policy on infection control and exposure management; provide staff training on the Occupational Safety and Health Administration (OSHA) standards and CDC guidelines; and supply dental staff with required vaccinations. Employees should understand protocol for equipment maintenance, disinfection, and sterilization methods; contaminated waste disposal; occupational exposure plans; documentation and monitoring; and requirements for immunizations and personal health risks.
Dental offices should have a clearly written office policy that defines or describes principles of infection control and occupational health, based on current scientific evidence and CDC recommendations. These should align with relevant federal, state, and local regulations and statutes. Staff should review office policies on an annual basis, with policies remaining accessible to all persons at risk of exposure to contaminated items or pathogens. A well-written policy explains risks encountered in the dental environment, and outlines infection control protocols to reduce accidents and exposures. It thoroughly discusses personal protective equipment, exposure control, post-exposure management, environmental infection control (barriers and surface disinfection, housekeeping, blood spills), sterilization, instrument processing, DUWL disinfection, and other relevant topics.2
Once established, policies need to be reviewed and updated. All new employees at risk of occupational exposure should be trained upon hire. The CDC recommends the policy be introduced at initial hire, anytime job roles change, and reviewed annually.2,7 All employees should understand and follow office policies. To assist in this task, it is prudent to assign the role of “infection control coordinator” to a designated staff member, who can help implement the policy and improve office personnel compliance. The coordinator takes ownership of the office policy document, overseeing office adherence to federal regulations, and certifying that all personnel are trained and maintaining documentation.7 A 2012 randomized survey of dentists practicing in the US found continuing education on infection control improves dentists’ attitude and compliance to CDC guidelines.21
Resources are available to assist in implementing an infection control policy for private practices, group practices, health organizations, hospitals, and educational settings involved in oral health care delivery.22 The office policy should include immunization protocols both required and recommended by the CDC Advisory Committee on Immunization Practices. Office personnel have a responsibility to advise their colleagues of any conditions, illnesses, or circumstances that put them at increased risk of infecting others. Employees should stay home when sick with a fever, vomiting, diarrhea, or any condition that may be transmissible. Similarly, patients should be encouraged to postpone any nonemergency treatment for the same reasons. The CDC recommends that health care professionals receive immunizations for hepatitis B, influenza, mumps, measles and rubella, tetanus, diphtheria, and varicella-zoster.7 OSHA requires employers to offer employees the hepatitis B virus immunization free of charge; employees have a right to decline, but must sign a declination waiver.

Following standard precautions and adhering to OSHA and CDC guidelines protects clinicians and their patients. Basic protocols for health care workers, called “standard precautions,” are employed for the sole purpose of protection. The rationale for the protocol is to treat all patients the same, because patients don’t always know if they possess an illness or infection, nor do they always accurately disclose the information to clinicians. By assuming all patients carry infectious pathogens, practitioners can use a blanketed set of standard precautions for protection against potential infection. Standard precautions are the foundation of infection control plans conceived by OSHA’s Revised Bloodborne Pathogens Standard and “universal precautions,” which state that all blood and body fluids contaminated with blood should be treated as infectious. This was expanded upon by the CDC to include all body fluids, secretion, and excretions (except sweat), whether or not they contain blood.23 In 2007, the CDC added safe injection practices, respiratory hygiene, and cough etiquette to protect health care workers.24
CONCLUSION
The risk from pathogenic microorganisms exists in the dental operatory from contaminated surfaces, DUWLs, and aerosols. Patients may not always know or reveal their infectious status. As such, clinicians must follow standard precautions, and, in some situations, transmission-based precautions to minimize the risk of infection. Dental offices should keep a written infection control policy, and provide staff with ongoing training on safety and infection control, based on current guidelines. The risk of transmission can further be reduced by following appropriate infection control and exposure control recommendations.
ACKNOWLEDGMENTS
- FIGURE 1. ALFRED PASIEKA / SCIENCE SOURCE
- FIGURE 2. JAMES CAVALLINI / SCIENCE SOURCE
- FIGURE 3. CNRI / SCIENCE SOURCE
- FIGURE 4. NIBSC / SCIENCE SOURCE
- FIGURE 5. BARRY DOWSETT / SCIENCE SOURCE
- FIGURE 6. JUERGEN BERGER / SCIENCE SOURCE
REFERENCES
- Petti S, Polimeni A. Risk of methicillin-resistant Staphylococcus aureustransmission in the dental healthcare setting: a narrative review. Infect
- Control Hosp Epidemiol. 2011;32:1109–1115.
- Thomas MV, Jarboe G, Frazer RQ. Infection control in the dental office.Dent Clin North Am. 2008;52:609?628.
- Centers for Disease Control and Prevention. Viral Hepatitis Statistics &Surveillance. Available at: www.cdc.gov/ hepatitis/ Statistics/index.htm.Accessed August 15, 2013.
- Centers for Disease Control and Prevention. Viral Hepatitis Statistics &Surveillance. Available at: www.cdc.gov/hepatitis/Statistics/2010Surveillance/Commentary.htm. Accessed August 15, 2013.
- Araujo MW, Andreana S. Risk and prevention of transmission of infectiousdiseases in dentistry. Quintessence Int. 2002;33:376?382.
- Centers for Disease Control and Prevention. Trends in tuberculosis—UnitedStates, 2012. MMWR Morb Mortal Wkly Rep. 2013;62:201–205.
- Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection control indental health-care settings—2003. MMWR Recomm Rep. 2003;52(RR- 17):1?61.
- Centers for Disease Control and Prevention. Vaccine and Immunizations.Available at: www.cdc.gov/ tb/ topic/vaccines. Accessed August 20, 2013.
- Centers for Disease Control and Prevention. HIV Surveillance Report.Diagnoses of HIV Infection and AIDS in the United States and DependentAreas, 2009. Available at: www.cdc.gov/hiv/pdf/ statistics_ 2009_ HIV_Surveillance_ Report_ vol_21.pdf. Accessed August 15, 2013.
- Centers for Disease Control and Prevention. Occupational HIV Transmissionand Prevention among Health Care Workers. Available at: www.cdc.gov/hiv/resources/factsheets/PDF/hcw.pdf. Accessed August 15, 2013.
- Dogruoz N, Illhan-Sungur E, Goksay D, Turetgen I. Evaluation of microbialcontamination and distribution of sulphate-reducing bacteria in dental units.Environ Monit Assess. 2012;184:133?139.
- Mill SE. Waterborne pathogens and dental waterlines. Dent Clin North Am.2009;47:545–557.
- Marciano-Cabral F, Cabral G. Acanthamoeba spp. as agents of disease inhumans. Clin Microbiol Rev. 2003;16:273?307.
- Ricci ML, Fontana S, Pinci F, et al. Pneumonia associated with a dental unitwaterline. Lancet. 2012;379:684.
- Barbeau J, ten Bokum L, Gauthier C, Prévost AP. Cross-contaminationpotential of saliva ejectors used in dentistry. J Hosp Infect. 1998;40:303–311.
- Centers for Disease Control and Prevention. Frequently Asked Questions—Saliva Ejector. Available at: www.cdc.gov/oralhealth/infectioncontrol/faq/saliva.htm. Accessed August 20, 2013.
- Rautemaa R, Nordberg A, Wuolijoki-Saaristo K, Meurman JH. Bacterialaerosols in dental practice—a potential hospital infection problem. J HospInfect. 2006;64:76?81.
- Pankhurst CL, Coulter WA. Do contaminated dental unit waterlines pose arisk of infection? J Dent. 2007;35:712?720.
- Manarte-Monteiro P, Carvalho A, Pina C, Oliveira H, Manso MC. Air qualityassessment during dental practice: aerosols bacterial counts in an universityclinic. Revista Portuguesa de Estomatologia, Medicina Dent‡ria e CirurgiaMaxilofacial. 2013;54(1):2–7.
- Harrel S K, Molinari J. Aerosols and splatter in dentistry: a brief review ofthe literature and infection control implications. J Am Dent Assoc. 2004;135:429–437.
- Hennessy B, Joyce A. A survey of preprocedurasl antiseptic mouth rinse usein army dental clinics. Mil Med. 2004;169:600–603.
- Cleveland JL, Foster M, Barker L, et al. Advancing infection control indental care settings: factors associated with dentists’ implementation ofguidelines from the Centers for Disease Control and Prevention. J Am DentAssoc. 2012;143:1127–1138.
- Harte JA. Standard and transmission-based precautions: an update fordentistry. J Am Dent Assoc. 2010;141:572–581.
- Siegel JD, Rhinehart E, Jackson M, Chiarello L. 2007 Guideline for isolationprecautions: preventing transmission of infectious agents in health caresettings. Am J Infect Control. 2007;35(10 Suppl 2):S65–S164.
From Dimensions of Dental Hygiene. September 2013; 11(9): 23–24, 26, 28–30

