Fighting Caries One Patient at a Time
An individualized approach to decreasing the incidence of caries and reversing the breakdown of tooth structure.
Midway through the year 2010 seems an appropriate time to look back on the goals set by Healthy People 2010—a set of health objectives for the United States to meet by the end of 2010—to see if the targets for oral health have been achieved. There is some good news: the United States now has fewer adults with untreated decay and tooth loss is less common in people younger than 65 years.1 However, approximately 28% of adults age 20 years to 65 years still have untreated decay.1 Caries rates continue to rise in the older adult population due to significant increases in root and secondary caries.1 And with life spans increasing and medical treatments expanding, particularly in pharmacotherapeutics, more teeth will be at risk for decay. All of these factors lead to a greater role for the dental hygienist to play in helping patients prevent or stop decay.
DEMINERALIZATION AND REMINERALIZATION
The caries process is an active process of demineralization and remineralization. Demineralization is the process of losing calcium and phosphate in the tooth in an acidic environment. The demineralization process occurs when cariogenic bacteria metabolize fermentable carbohydrates. Frequency of consumption and the type of sugar and fermentable carbohydrates consumed are important factors in the caries process. Xerostomia also is a risk factor for demineralization since saliva contains protective factors and helps move fluoride, calcium, and phosphate through the mouth.2
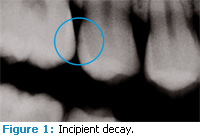
Demineralization occurs below an intact surface of a tooth in the presence of bacterial plaque—occurring simultaneously with remineralization. Remineral- ization is the process of depositing calcium and phosphate back into the tooth surface. If demineralization occurs at a greater rate than remineralization, eventually the sur- face will erode and frank cavitation occurs, requiring a restoration (Figure 1).
A tooth that has remineralized is more resistant to acid attack because of its higher organic content. Remineralization has to occur before a complete loss of minerals occurs and before the surface becomes involved. The optimal time for remineralization is while the surface remains intact, otherwise known as the white spot lesion phase. Remineralization is enhanced greatly in the presence of fluoride. Calcium increases binding sites for fluoride, which creates a synergistic relationship.2 An ideal clinical treatment for remineralization needs to have a quick application time and remain active for a prolonged period.
RISK ASSESSMENT
Treatment of caries has shifted emphasis from restorative procedures to prevention and treatment of the early signs of disease. Caries management by risk assessment (CAMBRA) is an evidence-based approach to caries prevention and caries management. Dental hygienists are traditionally the preventive specialists and can include CAMBRA in their protocol. CAMBRA helps dental hygienists determine if the patient needs prevention due to low caries risk or a more aggressive therapeutic approach because of a higher risk of caries or even existing demineralized areas. Caries risk is dependent on saliva level, presence of bacteria, diet, and the presence of biofilm. The use of CAMBRA assures an individualized treatment plan that can even be site specific.3
Nutritional counseling is part of CAMBRA. Determining the consumption of sugars and fermentable carbohydrates is effective in determining risk. One preventive effort often forgotten is the simple act of drinking water. If fluoride is present in the water supply, the benefits increase due to the ability of calcium to provide extra binding sites for fluoride.4
New forms of demineralization detection technology can help determine mineral loss before a restoration is required and should be included as a part of CAMBRA. However, caries detection technologies are supple- mental and should not be used as the only diagnostic tool. They need to be used in conjunction with radiographs and visual detection.
TREATMENT PLANNING FOR REMINERALIZATION
The dental hygienist should be part of the treatment planning process for remineralization. Individualized treatment is based not only on home care, compliance, and diet ary factors, but also on patient values and lifestyle. Dental hy gienists need to be knowledgeable about demineralization and remineralization technologies as they typically spend the most time with patients. Patients will be more compliant with new products or techniques if they do not require a major change in their routine.
FLUORIDE
Fluoride sources, both in-office topical and water, have been the traditional tools used for remineralization. Fluoride enhances re min eralization through two avenues. It decreases the pH in which the tooth begins to de min eralize and prevents bacteria from breaking down fermentable carbohydrates. The remineralized surface is stronger than the original tooth surface—creating a tooth surface more resistant to acid at tack. Fluoride works best in the presence of adequate saliva.3
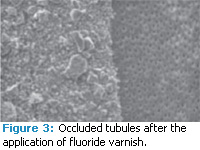
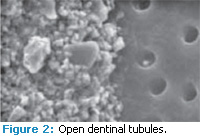
There are many fluoride choices for inoffice application and the best product to use should be determined by the risk levels and needs of the patient. Fluoride varnish (5% NaF) contains 22,600 ppm fluoride and has increased in popularity due to ease of use and the duration of action (figures 2 and 3). Fluoride varnish can be applied three to four times per year in high-risk patients. The need for more fluoride exposure at home can be addressed through pre- scription fluoride gels and pastes that contain 1.1% NaF. If the patient likes to rinse and has low caries risk, there are many over-the- counter fluoride mouthrinses that contain 0.05% NaF.
BEYOND FLUORIDE
Some patients may not want to use fluoride or may require a different strategy. The dental hygienist must then take on the role of investigator and find products that will fit into the current lifestyle of the patient. Fortunately, many options are available.
Xylitol is a sugar alcohol that cannot be metabolized by Streptococcus mutans (MS), one of the main bacteria implicated in the caries process. Xylitol also blocks the adherence of bacterial plaque to the tooth surface. It is sweet and can be used as a sugar substitute in many products such as gum and mints. It is low in calories and good for people who have diabetes because it does not stimulate the release of insulin. The ideal amount to be consumed per day is 6 mg to 10 mg. Too much xylitol can cause intestinal upset.3 Some examples of over-the-counter xylitol products include gum, mints, toothpastes, mouthrinses, and nasal sprays.
AMORPHOUS CALCIUM PHOSPHATE
A soluble calcium phosphate compound, amorphous calcium phosphate (ACP) delivers calcium and phosphate ions to aid in the re mineralization process.5 Tung et al6 found that at high paste-to-liquid ratios, ACP with the addition of fluoride was able to form tooth minerals. While studying the deep pits above the enamel prisms, Winston et al7 found that ACP was able to reduce the roughness of pits and the number of pits. The study also found that ACP remineralized tooth structure to a deeper level when used in conjunction with fluoride, than when fluoride was used alone.7 ACP is available in a variety of vehicles, such as toothpastes, prophy pastes, and sealant products. Gum containing ACP is currently under investigation. ACP prophy paste can start the remineralization process in the office without relying on patient compliance.
CPP-ACP
Casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) or Recaldent® is a protein derived from milk casein but is lactosefree. CPP-ACP is designed to supersaturate saliva with bioavailable calcium and phosphate, which have potential to deposit the calcium and phosphate into the tooth. More controlled studies need to be conducted regarding the re mineralization properties of CPP-ACP but early indications are positive with no side effects reported as long as the patient is not allergic to milk.3 Products that contain CPP-ACP include chewing gum and professionally-dispensed paste.
CALCIUM SODIUM PHOSPHOSILICATE
Calcium sodium phosphosilicate bioactive glass (NovaMin®) was initially used for repairing damaged bone. Since fluoride requires a source of calcium to be effective in remineralization—and salivary insufficiency is a common issue in people with root caries—Burwell et al studied the use of calcium sodium phosphosilicate as a remineralization agent for root caries. They found that when combined with fluoride, calcium sodium phosphosilicate promoted the remineralization of the root surface, even in the absence of saliva.8 Calcium sodium phosphosilicate is an ingredient in toothpastes, a prophy pastes, and an air pol- ishing powder.
THE ROLE OF THE DENTAL HYGIENIST
The dental hygienist is the key to individualized treatment for patients at risk for caries. Risk assessment should include CAMBRA, comprehensive health review, nutritional analysis, and the use of de mineralization detection technology. A comprehensive treatment plan includes prevention, caries reduction, and nutritional counseling, which must consider patient desire and motivation.
The dental hygienist’s focus is first on prevention, which can include fluoride and xylitol. If demineralization is already present, treatment can then move to the use of a calcium phosphate technology. Dental hygienists should consider a patient’s current self-care routine when determining which product will be easily adopted into the existing protocol. For patients who have xerostomia, gum, or mints may provide help in managing caries and possibly increase salivary flow. For patients who do not wish to change their routine, recommending a toothpaste may be the most beneficial strategy. Dental hygienists can significantly contribute to decreasing caries and reversing initial breakdown of tooth structure simply by finding the right product for each patient.
REFERENCES
- Healthy People 2010. Available at: www.healthypeople.gov. Accessed June 16, 2010.
- Zero DT, Fontana M, Martinez-Mier EA, et al. The biology, prevention, diagnosis and treatment of dental caries: scientific advances in the United States. J Am Dent Assoc. 2009;140:25S-34S.
- Young D, Kutsch VK, Whitehouse J. A clinician’s guide to CAMBRA: a simple approach. Compend Contin Educ Dent. 2009;30:92-94.
- Bruvo M, Ekstrand K, Arvin E, et al. Optimal drinking water composition for caries control in populations. J Dent Res. 2008;87:340-343.
- Chow LC, Takagi S, Vogel GL. Amorphous calcium phosphate: the contention of bone. J Dent Res. 1998; 77:6.
- Tung MS, Malerman SH, Mchale WA. Reactivity of prophylaxis pastes containing calcium, phosphate and fluoride salts. J Dent Res. 2005;84:Special Issue A.
- Winston AE, Charig A, Patel V, McHale WA. Effect of prophy pastes on surface of tooth enamel. J Dent Res. 2005;84:Special Isssue A.
- Burwell AK, Litkowski LJ, Greenspan DC. Calcium sodium phosphosilicate (NovaMin): remineralization potential. Adv Dent Res. 2009;21:35-39.
From Dimensions of Dental Hygiene. July 2010; 8(7): 38, 40, 42.