
The Five Most Common Errors When Using Ultrasonic Inserts
The effective use of ultrasonic instrumentation depends on dental hygienists using sound technique and avoiding these familiar mistakes.
Initial periodontal debridement and prophylaxis or periodontal maintenance is frequently provided with an ultrasonic scaler in addition to hand instrumentation. Ultrasonic instrumentation offers significant benefits both to treatment outcomes and the dental hygienist. The ability of the ultrasonic scaler to provide lavage allows for the rinsing and removal of the smear layer that remains after hand instrumentation.1 Also, ultrasonic instrumentation is an ergonomic approach that is less likely to contribute to muscle strain, fatigue, and pain than hand instrumentation.2
There is a perception that treatment with an ultrasonic scaler is easier and less dependent on technique than comparable treatment with hand instruments. Most issues of angulation of the blade, application of lateral pressure, and the need to sharpen the instrument are eliminated by the use of ultrasonic instrumentation. However, using the proper technique with the correct ultrasonic insert is key to the effective use of the modality. As the use of ultrasonic instrumentation has grown in the practice of dental hygiene so has the level of user error.

Error Number 1: Worn Inserts
A common error is using an insert that is shortened through wear and, as a result, is less effective for patient treatment. Almost all manufacturers now provide wear guides for their inserts. Because tips gradually lose length through wear and also because the action in the hand continues to feel the same, it is not always apparent that a tip has lost its effectiveness. Most manufacturers of ultrasonic inserts note that the loss of little more than 1 mm of length results in a reduction of about 25% of the instrument’s effectiveness and the loss of the same amount again reduces its effectiveness by 50% (Figure 1).
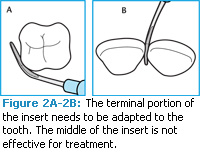
Error Number 2: Not Using the Tip’s Terminal Portion
Many dental hygienists make the mistake of not using the terminal portion of the tip. If the wear guides state that an ultrasonic insert is 50% less effective when it has lost 2 mm to 3 mm of the tip then it is logical to assume that this is the most important part of the tip. Thus, it should be used carefully to adapt to the tooth (Figure 2A-2B).
This is certainly a familiar concept but many dental hygienists have trouble implementing it. For example, in a patient with recession in the mandibular anteriors it is easy to let the tip extend through the interproximal area and adapt the middle of the tip instead of only the last few millimeters. This doesn’t harm the patient but it reduces the effectiveness of biofilm or calculus removal. Another example occurs at line angles and mid-proximally when the tip is not well adapted to the convexities and concavities found in these areas. Rotation of the tip either does not start soon enough or is not completed as the dental hygienist proceeds from the buccal or lingual surface toward the proximal surface. When working supragingivally, this is ineffective. When working subgingivally, this is both ineffective and potentially uncomfortable for the patient as the tip leaves the tooth surface and comes in contact with the soft tissue.
Proper adaptation is thus a limiting factor with ultrasonic instrumentation just as with hand instrumentation.
Error Number 3: Using Only the Point on the Root Surface
Another frequent mistake is using the most terminal portion of the tip on the root surface of the tooth (Figure 3A-3B). The point in both magnetostrictive inserts and piezoelectric inserts has the highest concentration of power. Use of this part of the insert can be very effective in fracturing and removing large calculus ledges. Using the point to tap on the top of a heavy calculus ring is a commonly recommended technique. Brief contact of the point to sound enamel is probably not harmful because the enamel surface is very hard. However, repeated contact of the point to the root can cause loss of tooth structure. This is a gradual and cumulative process. Because no visible change occurs in one appointment, dental hygienists may lose sight of the importance of adaptation even when they know the point can be dangerous.
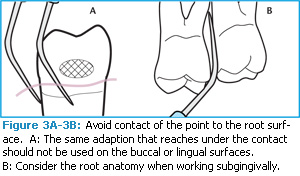 There are two common clinical situations where this problem occurs. One is when a curved or contra-angled tip adapted to a posterior tooth is positioned with the point curving in toward the tooth. The other is when an insert is adapted to and parallel with a proximal surface and then swept around to the buccal or lingual areas with no rotation, which results in the point now contacting these surfaces instead of the side of the insert. The second situation is when an insert is adapted with the toe toward the interproximal surface and then swept around the buccal or lingual surface allowing the point to make contact instead of rotating the tip to use the side of the insert. The Tips on Technique column by Anna M. Pattison, RDH, MS, in the February 2009 issue of Dimensions of Dental Hygiene provides graphic examples of the damage to a root caused by repeated treatment with the point of an ultrasonic insert.3
There are two common clinical situations where this problem occurs. One is when a curved or contra-angled tip adapted to a posterior tooth is positioned with the point curving in toward the tooth. The other is when an insert is adapted to and parallel with a proximal surface and then swept around to the buccal or lingual areas with no rotation, which results in the point now contacting these surfaces instead of the side of the insert. The second situation is when an insert is adapted with the toe toward the interproximal surface and then swept around the buccal or lingual surface allowing the point to make contact instead of rotating the tip to use the side of the insert. The Tips on Technique column by Anna M. Pattison, RDH, MS, in the February 2009 issue of Dimensions of Dental Hygiene provides graphic examples of the damage to a root caused by repeated treatment with the point of an ultrasonic insert.3
Error Number 4: Adaptation
There are two primary ways that the ultrasonic insert can be adapted to the tooth. Most of the time the tip should be positioned so that it is parallel to the root surface being treated. The tip will be positioned just like a periodontal probe to assess the periodontal sulcus or pocket around the entire perimeter of the tooth. This technique is the only approach that allows for adequate access to soft tissue attachment topography without limitation. It is the best strategy for achieving comprehensive coverage of the dentition’s most challenging areas: line angles, mid-proximal contours, and deeper periodontal pockets (Figure 4A-4B).
 The second adaptation is to position the tip so the terminal portion points to the interdental space, parallel to the occlusal plane. This puts the terminal portion of the insert tip perpendicular to the long axis of the tooth while the handle is more parallel. This adaptation approach is ideal for working around and immediately under the contact area where calculus often remains (Figure 4C). In healthy mouths where intact papillae fill the embrasure space of shallow sulci, proximal surface debridement with this adaptation can work. However, it is not effective in treating line angles or facial or lingual surfaces. Its use on these surfaces often positions the point on the tooth (see error number 3).
The second adaptation is to position the tip so the terminal portion points to the interdental space, parallel to the occlusal plane. This puts the terminal portion of the insert tip perpendicular to the long axis of the tooth while the handle is more parallel. This adaptation approach is ideal for working around and immediately under the contact area where calculus often remains (Figure 4C). In healthy mouths where intact papillae fill the embrasure space of shallow sulci, proximal surface debridement with this adaptation can work. However, it is not effective in treating line angles or facial or lingual surfaces. Its use on these surfaces often positions the point on the tooth (see error number 3).
Effective treatment of all tooth surfaces requires both adaptation approaches: vertical orientation (as in probing) with the tip parallel to roots for subgingival areas and root surfaces exposed by recession, and horizontal orientation with the tip perpendicular to the long axis to work around the contact. For a periodontally involved patient, most of the treatment time should be spent with the tip pointed into the pocket and adapted like a probe. To summarize error number 4, the problem can be:
- Failure to use both methods of adaptation for complete treatment.
- Use of perpendicular adaptation where it is not effective.
- Failure to use probe-like adaptation for the majority of the treatment.

Error Number 5: Not Using Enough Strokes
Another frequent error is failure to adequately cover root surfaces with the overlapping, multidirectional strokes necessary for thorough treatment (Figure 5). The narrow width of physical contact between an ultrasonic tip and the tooth surface makes the tip’s effective area of debridement small. Treatment is best accomplished with the goal of touching every square millimeter of subgingival root surface. The advantage of using ultrasonic intrumentation is that strokes are light pressured and performed more quickly and without concern for angulation than with a hand instrument. Effective ultrasonic treatment still takes many erasing motion strokes over any given surface and is not accomplished by sweeping from one contact area to the next. Treatment with an ultrasonic insert should not be confused with oral irrigation. It is the high frequency vibrations of the tip in a fluid environment that creates the turbulence and acoustic microstreaming needed to disrupt the biofilm—not a simple rinsing action as the tip moves by the surface.
ltrasonic instrumentation is an important part of dental hygiene treatment. It is most effective when there is careful and thoughtful attention to technique and especially to the adaptation of the tip of the insert and to complete treatment of the root surfaces.
References
- Drisko CH. Root instrumentation. Power-driven versus manual scalers, which one? Dent Clin North Am. 1998;42:229-244.
- Ryan DL, Darby M, Bauman D, Tolle SL, Naik D. Effects of ultrasonic scaling and hand-activated scaling on tactile sensitivity in dental hygiene students. J Dent Hyg. 2005;79:9.
- Pattison AM. The safe use of ultrasonics. Dimensions of Dental Hygiene. 2009;7(2):58
From Dimensions of Dental Hygiene. July 2010; 8(7): 46, 48, 50.


