Effective Use of the AMSA Nerve Block
These strategies will boost your confidence and improve success rates.
The relatively new anterior middle superior alveolar (AMSA) nerve block is an important addition to the dental hygienist’s pain control armamentarium. Providing adequate pain control allows a patient to comfortably receive necessary treatment, such as scaling and root planing, and it helps the dental hygienist perform procedures without hesitation due to the possible pain experienced by the patient.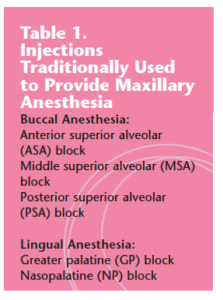
In the mandible, delivering widespread anesthesia is reasonably easy to accomplish with one or two injections. On the other hand, maxillary quadrant anesthesia can require up to five or more injections (see Table 1 for a list), including at least two that must be administered from the palatal aspects of the teeth.1 The AMSA block addresses this disparity by decreasing the number of injections and the overall volume of local anesthetic agent necessary to achieve anesthesia of a maxillary quadrant.1 Reducing the total number of injections can decrease the pain felt by the patient as well as the anxiety experienced by both the patient receiving the injections and the dental hygienist who administers them. 2,3

Unlike traditional local anesthetic injections, the AMSA block is too new to benefit from decades of clinical experience. However, much has been learned since its introduction and incorporating simple modifications to technique can improve its predictability and efficacy.1
History of the AMSA Block
Friedman and Hochman introduced the AMSA block along with a computer-controlled local anesthetic device (CCLAD) in 1998 (see Figure 1). 4,5 The use of the AMSA block has increased because of several advantages. In addition to its ability to provide widespread pulpal and periodontal anesthesia with fewer injections, the AMSA block does not typically anesthetize the labial tissues, which allows for the perioperative assessment of smile and lip lines during and after cosmetic procedures.
Past reports conflict over the efficacy of the use of the AMSA block. One of the few studies that assessed its clinical efficacy reported only modest success rates ranging from 35% to 58%.6 However, another study during the same period in cluded the following summary: “The results of the present study showed a statistically significant lower level of pain (p< 0.001) for local anesthesia with the AMSA-technique, compared to conven tional pala tal anesthesia.”7 Two additional studies in 2004 reported significant benefits when using the AMSA block for perio dontal therapy.8,9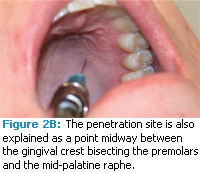
An unpublished reaction survey conducted at Eastern Washington University’s Department of Dental Hygiene during the same period (2003 to 2006) suggested that much higher success rates are possible. While slightly more than 80% of students reported success with the technique, 98% of the students who completed the survey indicated that they intended to use the AMSA block in the future.
AMSA Block Technique
While early literature may have reported conflicting information about overall success rates, increasing numbers of dental hygienists have already integrated the AMSA block into their maxillary anesthesia routines.1,7,8-10 Following are several strategies that can be used to increase the efficacy of the AMSA block:
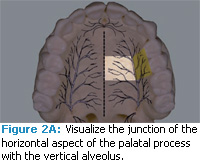
- Determine the penetration site by observing the intersection of the horizontal and vertical aspects of the palate opposite the apices of the premolars (the junction of the alveolus and palatine processes). In most cases, this site of penetration is just as accurate and easier to locate compared to calculating a point midway between the gingival crest bisecting the premolars and the median palatine raphe (see Figure 2A and 2B).
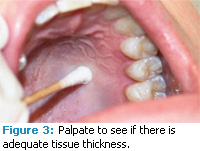
- Select a penetration site that can easily accommodate solution volumes (see Figure 3). Somewhat spongier sites may work better, and they can be located with a cotton swab. Occasionally, patients do not have enough spongy palatal tissue available to allow the administration of effective AMSA blocks.
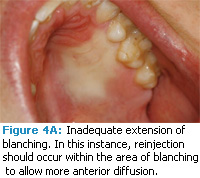
- Select additional penetration sites if the local anesthetic agent does not diffuse far enough in an anterior or posterior direction to cover all treatment areas in the palate. If the solution fails to diffuse far enough anteriorly or posteriorly (see Figure 4A), it may be helpful to withdraw and select another penetration site that is more anterior or more posterior depending on the pattern of diffusion. For comfortable injections, these new penetration sites should be located within existing areas of blanching.
![]()
-
- Reinject with another AMSA block when anesthesia is inadequate. Dental hygienists may be tempted to abandon the AMSA block when anesthesia is inadequate but many anesthetic procedures require the use of different techniques to achieve success. Reinjection with AMSA blocks after reconsidering the penetration and deposition sites can significantly improve success rates.
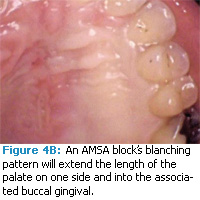
- Observe the progression of the slow diffusion of solution in the palate by following the blanching (see Figure 4B). A typical maximum rate of deposition that allows optimal diffusion without tissue trauma is 0.5 ml over 60 seconds, which is one cartridge over 3 minutes when using 2% and 3% drugs. A timer is helpful in accomplishing the correct rate of diffusion. In some instances, these slow rates can lead to hand fatigue. If patients are unwilling or unable to tolerate long administration times, this technique should be avoided.
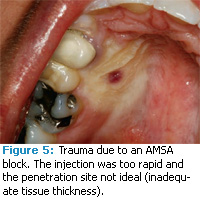
- Avoid tissue trauma. Tissue trauma, evidenced by excessive blanching and/or ballooning, suggests that deposition rates need to be reduced further (see Figure 5). Some patients have experienced significant burning sensations with the AMSA block despite negative aspiration and appropriate rates of deposition with all five available amide local anesthetics (see sidebar for a list of local anesthetic agents). The AMSA block may be contraindicated for these patients.1
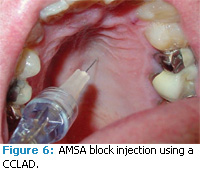
![]() Use the appropriate equipment. For dental hygienists with small hands, petite syringes can improve stability and reduce fatigue when lengthy palatal injections are administered. CCLADs are designed for the delivery of solution under controlled pressures compared to conventional syringes. They can also eliminate most hand fatigue and may reduce the pain felt by the patient. (see Figure 6).12 CCLADs take advantage of constant, pre-set delivery rates that are ideal for AMSA injections.
Use the appropriate equipment. For dental hygienists with small hands, petite syringes can improve stability and reduce fatigue when lengthy palatal injections are administered. CCLADs are designed for the delivery of solution under controlled pressures compared to conventional syringes. They can also eliminate most hand fatigue and may reduce the pain felt by the patient. (see Figure 6).12 CCLADs take advantage of constant, pre-set delivery rates that are ideal for AMSA injections.![]()
By incorporating specific strategies into the delivery of the AMSA nerve block, dental hygienists can experience greater success which, in turn, can lead to increased confidence. These suggestions are easy to incorporate into clinical routines and can allow for more efficient and productive appointments.
| Special Considerations for Drug Selection with AMSA Nerve Blocks1,10
When selecting a local anesthetic agent for an AMSA nerve block, drug concentration and total volume delivered are key considerations. Solutions of 4% drugs may increase the risk of paresthesia, therefore, the total volume delivered should be no more than 0.9 ml (~1/2 cartridge) for these agents. The total time taken to administer 4% drugs remains the same, approximately 3 minutes for 0.9 ml It is important to monitor palatal tissues for excessive blanching during deposition. Solutions with higher concentrations of vasoconstrictors (such as 1:50,000) should be avoided to reduce the risk of post-operative pain and possible necrosis. Summary of Local Anesthetic Agents Used In Dentistry1,10,11 LIDOCAINE Concentration: 2% Lidocaine is available without a vasoconstrictor or with a vasoconstrictor (1:50,000 epinephrine or 1:100,000 epinephrine). Without a vaso con strictor, lidocaine’s duration is 5 minutes to 10 minutes for pulpal anesthesia and approxi mately 1 hour to 2 hours for soft-tissue anes thesia. Adding the vasoconstrictor epine phrine increases its duration to 60 minutes to 90 minutes for pulpal tissue and approxi mately 3 hours to 5 hours for soft tissue. MEPIVACAINE Concentrations: 2% and 3% Mepivacaine is available with or without a vasoconstrictor. Three percent mepivacaine without a vasoconstrictor provides 20 minutes to 40 minutes of pulpal anesthesia and 2 hours to 3 hours of soft-tissue anesthesia. Adding the vasoconstrictor levonordefrin increases pulpal anesthesia to 60 minutes to 90 minutes and soft-tissue anesthesia to 3 hours to 5 hours. Prilocaine comes with or without a vasoconstrictor and the duration of anesthesia provided depends on whether a vasoconstrictor is included and the type of injection used. Without a vasoconstrictor, pulpal anesthesia lasts approximately 5 minutes to 10 minutes and soft-tissue anesthesia lasts 1 hour to 2 hours. During a nerve block without a vaso constrictor, 40 minutes to 60 minutes of pulpal anesthesia and 2 hours to 4 hours of soft-tissue anesthesia are provided. Adding a vaso constrictor lengthens pulpal anesthesia to 60 minutes to 90 minutes and 3 hours to 8 hours of soft-tissue anesthesia and is not dependent on the type of injection administered. ARTICAINE Concentration: 4% Articaine is used only with a vasoconstrictor and is available with 1:100,000 epinephrine or 1:200,000 epinephrine. It provides 45 minutes to 75 minutes of pulpal anesthesia and 3 hours to 6 hours of soft-tissue anesthesia. BUPIVACAINE Concentration: 0.5% Bupivacaine is also available only with a vasoconstrictor—1:200,000 epinephrine. Bupivacaine creates 1.5 hours to 5 hours of pulpal anesthesia and 4 hours to 9 hours of soft-tissue anesthesia. |
REFERENCES
- Bassett KB, DiMarco AC, Naughton DK. Local Anesthesia for Dental Professionals. Upper Saddle River, NJ; Pearson Education: 2010.
- Simon JF, Peltier B, Chambers D, Dower J. Dentists troubled by the administration of anesthetic injections: long-term stresses and effects. Quintessence Int. 1994;25(9):641-646.
- Matthews DC, Rocchi A, Gafni A. Factors affecting patients’ and potential patients’ choices among anaesthetics for periodontal recall visits. J Dent. 2001;29:173-179.
- Friedman MJ, Hochman MN. The AMSA injection: a new concept for local anesthesia of maxillary teeth using a computer-controlled injection system. Quintessence Int. 1998;29:297-303.
- Friedman MJ, Hochman MN. A 21st century computerized injection system for local pain control. Compendium. 1997;18:995-1003.
- Lee S, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of the anterior middle superior alveolar nerve block (AMSA) injection. Anesth Prog. 2004;51:80-89.
- Sculean A, Kasaj A, Berakdr M, Willershausen B. A comparison of the traditional injection and a new anesthesia technique (The Wand®) for non-surgical periodontal therapy. Periodontal Practices Today. 2004;1(4):363-368.
- Loomer PM, Perry DA. Computer-controlled delivery versus syringe delivery of local anesthetic injections for therapeutic scaling and root planing. J Am Dent Assoc. 2004;135:358-365.
- Al Amoudi N, Feda M, Sharaf A, Hanno A, Farsi N. Assessment of the anesthetic effectiveness of anterior and middle superior injection using computerized device versus traditional technique in children. J Clin Pediatr Dent. 2008;33:97-102.
- Malamed SF. Handbook of Local Anesthesia. 5th ed. St. Louis: Elsevier; 2004.
- Paarmann C. Decision making and local anesthesia. Dimensions of Dental Hygiene. 2008;6(10):24.
- Loomer PM, Perry DA. Pain perception when using computer-controlled anesthetic device compared to conventional aspirating syringe. J Dent Res. 2002;80:81.
From Dimensions of Dental Hygiene. July 2010; 8(7): 30-32, 34.