VAASEENAA/ISTOCK/GETTY IMAGES PLUS
VAASEENAA/ISTOCK/GETTY IMAGES PLUS
Effects of a Plant-Based Diet on Oral Health
As the association between periodontal health, systemic disease, and nutrition becomes more clear, dental hygienists need to expand their knowledge of the effects of diet on immune response.
This course was published in the November 2020 issue and expires November 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define the attributes of a whole food plant-based diet.
- Discuss the relationship between diet and oral health.
- Identify key nutrients’ impact on periodontal health.
Dental hygienists can play a role in reducing the morbidity and mortality associated with poor nutrition and other lifestyle habits. Increasing evidence of the relationship between physical and oral health emphasizes the urgency of increasing the public’s understanding of the effects of poor nutrition. Early data from the COVID-19 pandemic show that those with chronic diseases, such as diabetes, obesity, and cardiovascular disease (CVD), are more severely affected by the virus. The mechanisms behind this are not fully understood, but a new study posits that the health of the gut microbiome plays a crucial role.1 The microbiome is integral to immune function, and diet is important in cultivating healthy gut microbiomes. Eating a high-fiber, plant-rich diet with plenty of fruits, vegetables, whole grains, and legumes encourages the growth of a healthy microbiome, improving immunity and overall health.
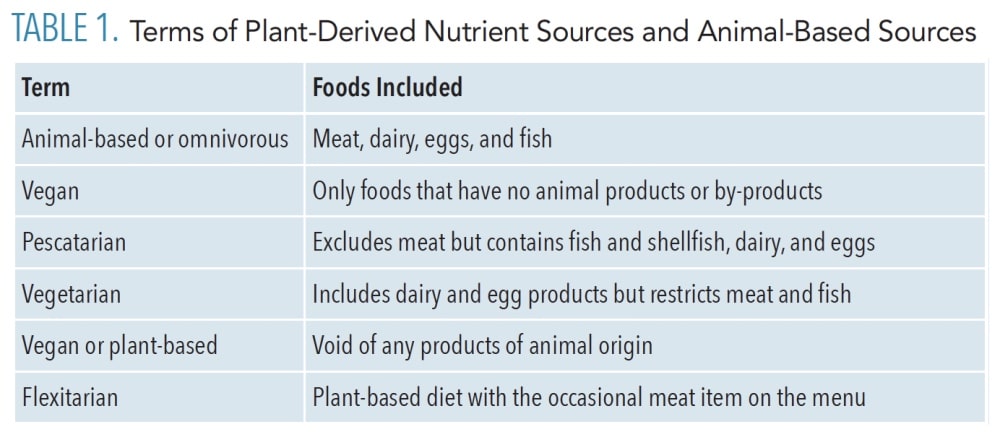
A whole food plant-based diet (WFPBD) requires that all or a majority of foods consumed are unaltered in their natural form rather than processed, extracted, and/or isolated parts of something else. A whole food diet is not to be confused with a raw diet because cooking is not considered when determining whether a product is processed. A plant-based, or vegan, diet and a WFPBD are similar in the sense that all components of both diets come from plant sources. However, a WFPBD does not include processed vegan products such as imitation meats and cheeses, refined grains, or isolated plant parts such as salt, oil, or sugar (Table 1). WFPBD sources all nutrients from fruits, vegetables, whole grains, legumes, nuts, and seeds.
This article looks at the benefits of a WFPBD on periodontal health in comparison to an animal-based diet. The foods and their nutrients are meant to be considered in whole form only, and do not include those that are processed. Further research is needed to determine the benefits of a vegan diet that encompasses processed plant-based foods on periodontal health when compared to animal-based diets.
Whole Food Plant-Based Diet and Oral Health
The United States Centers for Disease Control and Prevention reports that nearly 50% of adults between the ages of 30 and 65 experience periodontal diseases, and approximately 64% of those older than age 65 have moderate to severe periodontitis.2 Caries is also a widespread oral health problem, and the World Health Organization (WHO) project, Global Burden of Disease, names untreated dental caries in permanent teeth as the most common health condition worldwide.3
Dental caries and periodontal diseases are preventable diseases heavily influenced by the host’s resident oral microbiota.4 While mechanical removal of oral biofilm is necessary to prevent periodontal diseases, nonmechanical means of disease prevention are more important than originally speculated. In a 2011 systematic review, dietary modification was found to be more effective in preventing caries than flossing.5 Dietary habits greatly dictate the environmental conditions for microbial growth in the mouth.4 A plethora of scientific evidence has shown that a WFPBD is protective against several chronic diseases including cancers, CVD, obesity, and type 2 diabetes.6–8 The evidence is strongest for vegetable intake, with high levels of vegetable consumption reducing the risk of CVD and cancer by 23% and 50%, respectively.6 The bidirectional relationship between systemic disease and periodontal diseases is well known to dental hygienists. An understanding of the shared inflammatory response characteristics, and using inflammation reducing practices, such as a WFPBD, will benefit the treatment of both systemic and periodontal diseases alike.4,7
One commonly referenced clinical study, published in the European Journal of Clinical Nutrition, observed 100 vegetarians (89 lacto-ovo-vegetarians, 11 vegans) and 100 omnivores.9 Periodontal risk factors including age, gender, and smoking habits were matched, however body mass index was not. The results showed that vegetarians had significantly less periodontal disease indicators, including reduced probing depths, less bleeding on probing, decreased tooth mobility, fewer missing teeth, reduced inflammation, and decreased plaque biofilm.9 The study also demonstrated that vegetarians had higher levels of education; overall healthier lifestyle habits, such as less consumption of alcohol and increased physical activity; less obesity; and reduced prevalence of systemic diseases. All of these may have impacted the results.
High serum cholesterol has been linked to systemic diseases such as CVD, diabetes, liver disease, and periodontal diseases.10 Cholesterol, one of the three types of lipids, is naturally produced by the liver and is important for various bodily functions. Elevated serum cholesterol, specifically low-density lipoprotein, is a direct result of over-consumption of cholesterol-rich foods, and all animal products contain cholesterol. Animal products also contain harmful saturated fats, and saturated fat-rich diets increase oxidative stress and prolong the intensity and duration of the inflammatory response.11 Dietary impact on systemic diseases has been highly studied but conclusive research on the impact of a specific diet pertaining to periodontal health is rare. The study of particular nutrients’ impact on periodontal health is more abundant and conclusive, better detailing the benefits of a WFPBD.
Key Nutrients
Lipids perform three primary biological functions within the body: serve as structural components of cell membranes, function as energy storehouses, and are important signaling molecules. Data show lipids play an important role in the modulation of the white blood cell response. Dietary fats can be both positive and negative to periodontal health, depending on the type of fatty acids present.11,12 Saturated fatty acids overload the Kreb’s cycle, which initiates oxidative stress and upregulates pro-inflammatory molecules, thus increasing the risk of periodontal diseases by direct cell damage.11 A WFPBD contains few calories from saturated fats. Nuts, seeds, and avocados contain small amounts of saturated fats but whole grains, fruit, and vegetables do not. For an animal-based diet, many calories come from saturated fats.
While a diet high in saturated fat dramatically minimizes the immune response, anti-inflammatory omega-3 fatty acids do quite the opposite by downregulating pro-inflammatory gene expression. In addition to preventing periodontal diseases through anti-inflammatory means, long chain omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid have shown to provide antibacterial properties and can inhibit periodontal pathogens, Porphyromonas gingivalis, Fusobacterium nucleatum, and Prevotella intermedia.12 Furthermore, some types of omega-6 fatty acids show the same highly negative effects on periodontal health as saturated fats.12 These particular omega-6 fatty acids compete against the positive effects of omega-3 fatty acids and, therefore, the ratio of omega-6 to omega-3 fatty acids must be closely monitored. For example, flaxseeds and walnuts have a very high omega-6 to a lower omega-3 ratio. At first glance, this may seem to be a negative aspect for plant sources of omega-3. This is not true, however, because all animal foods contain an omega-6 fatty acid called arachidonic acid. This fatty acid is a dangerous, pro-inflammatory acid. Poultry and eggs are substantially high in arachidonic acid. But in plant sources, the notable omega-6 fatty acid present is called gamma-linoleic fatty acid. This type of fatty acid is both highly anti-inflammatory and even decreases dietary arachidonic acid levels in plasma/serum phospholipids.12 For example, salmon, even with a high omega-3 to omega-6 ratio, increases overall levels of the dangerous arachidonic acid in the body which, in turn, eradicates the positive effects of the omega-3s from the fish. When one serving of walnuts is consumed, not only do levels of healthy, anti-inflammatory omega-3 and gamma-linoleic acids increase, the gamma-linoleic acids also decrease preexisting arachidonic acid levels in the system by about 7%.13
Omnivores consume high levels of cell-destroying saturated fats and must monitor animal sourced, pro-inflammatory arachidonic omega-6 fatty acid intake to ensure they are not overpowering their omega-3 intake. Those who follow a WFPBD have little saturated fats in their foods and can disregard omega-6 to omega-3 ratio because only healthy, highly anti-inflammatory and antibacterial fatty acids are present in plant foods.7,8
Nitric oxide, a reactive nitrate intermediate (RNI), acts as a vasodilator, increasing blood flow and decreasing blood pressure. This significantly impacts cardiovascular health, boosts athletic endurance, and even treats erectile dysfunction. RNIs affect periodontal health as well. In a double blind, placebo-controlled, randomized trial, the administration of dietary nitrates from lettuce showed a major reduction in gingival redness, inflammation, ulceration, bleeding on probing and/ or spontaneously, and a clear increase in salivary nitrate levels when compared to both baseline and control group in just 14 days.14 In addition, RNIs have strong antimicrobial properties that fight off bacterial, fungal, parasitic, and viral pathogens. Considering that nearly 25% of circulating nitrate is accumulated in salivary glands and converted to nitric oxide by anaerobic bacteria on the tongue, there’s no doubt nitrates play an enormously positive role in periodontal health.14
Considering the source of nitrates is integral to reaping their benefits. Nitrates occur naturally in soil, air, and water so they play a vital role in the life cycle of all plants. Vegetables have an enormous number of nitrates and so do fruits, nuts/seeds, and legumes in varying amounts. Animal-based foods, such as meat and dairy, also contain nitrates because animals eat plants. Nitrates are even added to processed meats as a preservative (hence their antimicrobial effects). Nitrates in meat are accompanied by high amounts of amino acids from an abundance of protein. The pair binds together to form nitrosamines before the meat is ingested.14 This binding reaction is accelerated under high temperatures during cooking. These nitrosamines are considered potent, mutagenic carcinogens.15 The WHO indicates that processed meats, such as ham, bacon, and lunch meats, are classified as carcinogenic to humans, along with smoking tobacco and asbestos, because of their high levels of nitrosamines.17 Regulatory establishments like the US Food and Drug Administration, have placed limitations of added nitrates in meat to prevent nitrosamines from reaching hazardous levels.15 Nitrosamines cause inflammation, atherosclerosis, oxidative stress, and damage cells, decreasing immune response, which leads to the progression of periodontal diseases.16 These inflammatory processes are not seen with vegetable consumption because they contain much less protein and are not typically cooked at high enough temperatures for such bonds to occur. When nitrates in plants are ingested, they are broken down by enzymes in saliva to nitrites, and then further reduced to healthy RNIs like nitric oxide.14
When discussing dietary impact on periodontal diseases, fermentable carbohydrates top the list as the most problematic.5 Foods and beverages containing refined sugars increase inflammation and cause salivary pH to drop, wreaking havoc on oral health. When considering a WFPBD, one might assume that the multitude of calories from fruit would cause damage to periodontal health. In a randomized controlled study, researchers compared periodontal health at baseline to a 2-month supplementation of either fruit or nuts. There was no significant change in the nut group. For the fruit group, periodontal health significantly improved, even with the added levels of acidity and sugar from fruit.18 Researchers hypothesized that the results are due to the antioxidants present in fruit and their anti-inflammatory qualities. In another study, researchers found that the phenolic acids, polyphenols, and flavonoids found in fruits and vegetables not only inhibit oxidative mechanisms, such as inflammation, but have profound antimicrobial properties.19 When exposed to the antioxidants in strawberries, pathogens Streptococcus aureus, S. pneumoniae, Klebsiella pneumoniae, and Escherichia coli levels were all decreased.19 This shows that the researchers in the fruit and nut study were correct about their anti-inflammatory hypothesis, but fruits also kill pathogens that can cause disease in the mouth. The antioxidants in fruit are so powerful that in randomized, double-blind, placebo-controlled study, blueberries were shown to not only decrease inflammation, but also improve the body’s overall insulin sensitivity.20 This means supplementing a diet with blueberries reduces the body’s susceptibility to systemic inflammation even after consuming separate forms of sugar, including refined. While no specific serving of blueberries is right for everyone (digestion and absorption of nutrients is a complex process that varies from person to person), consumption of blueberry and blueberry products confer immunomodulatory, antioxidant, and anti-inflammatory health benefits.20,21
People following a WFPBD avoid refined/extracted sugars so their main source of sugar comes from whole fruits, packed with these protective antioxidants. The typical omnivorous American diet does not place such restrictions, so they are susceptible to the harmful effects of fermentable carbohydrates including sugars in beverages and desserts. Aside from refined sugars, naturally occurring sugars from animal sources include lactose found in dairy. Despite the calcium present in whole milk, the WHO estimates that 530 million children experience “milk teeth,” or eroded enamel.5 Oral biofilm formation, driven by S. mutans, increases when exposed to lactose, as opposed to sucrose and glucose.21
Conclusion
As research continues to support the strong association between periodontal health, systemic disease, and nutrition, dental hygienists must expand their knowledge of the effects of diet on immune response. Oral health professionals must continuously promote dietary advice and use evidence-based nutrition adjustments, alongside other forms of patient education, in treatment plans. The conversation must go beyond the topic of fermentable carbohydrates and address the negative influences of poor nutrition, eg, diets high in unrefined sugar and processed foods. Becoming more knowledgeable about good nutrition will allow dental hygienists to provide holistic, evidence-based care. Dental hygienists are encouraged to refer patients to nutritionists to learn more about how a plant-based diet can improve their health but can also continue learning about the WFPBD.
References
- Guo W, Yuanqing F, Liang Y, et al. Gut microbiota may underlie the predisposition of healthy individuals to COVID-19. Available at: medrxiv.org/content/10.1101/2020.04.22.20076091v1.full.pdf+html. Accessed October 29, 2020.
- Eke PI, Dye B, Wei L, Thornton-Evans G, Genco R. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91:914‐920.
- United Nations General Assembly. Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Noncommunicable Diseases. Available at: un.org/en/ga/ncdmeeting2011/. Accessed October 29, 2020.
- Marsh PD, Devine DA. How is the development of dental biofilms influenced by the host? J Clin Periodontol. 2011;38:28–35.
- Gurenlian JR. Interproximal biofilm management: lessons learned from the 11th European Workshop in Periodontology. Int J Dent Hyg. 2015;13:237–238.
- Fardet A, Boirie Y. Associations between food and beverage groups and major diet-related chronic diseases: an exhaustive review of pooled/meta-analyses and systematic review. Nutr Rev. 2014;72:741–762.
- Wright N, Wilson L, Smith M, Duncan B, McHugh P. The BROAD study: A randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Nutr Diabetes. 2017;7:e256.
- Norat T, Scoccianti C, Boutron-Ruault MC, et al. European code against cancer 4th edition: diet and cancer. Cancer Epidemiol. 2015;39:S56–S66.
- Staufenbiel, I., Weinspach, K., Förster, G. et al. Periodontal conditions in vegetarians: a clinical study. Eur J Clin Nutr. 2013;67:836–840.
- Thapa S, Wei F. Association between high serum total cholesterol and periodontitis: National Health and Nutrition Examination Survey 2011 to 2012 Study of American Adults. J Periodontol. 2016;87):1286–1294.
- Varela-López A, Giampieri F, Bullón P, Battino M, Quiles J. Role of lipids in the onset, progression and treatment of periodontal disease. a systematic review of studies in humans. Int J Mol Sci. 2016;17:1202.
- Rett BS, Whelan J. Increasing dietary linoleic acid does not increase tissue arachidonic acid content in adults consuming Western-type diets: a systematic review. Nutr Metab (Lond). 2011;8:36.
- Chiang Y-L, Haddad E, Rajaram S, Shavlik D, Sabaté J. The effect of dietary walnuts compared to fatty fish on eicosanoids, cytokines, soluble endothelial adhesion molecules and lymphocyte subsets: a randomized, controlled crossover trial. Prostaglandins Leukot Essent Fatty Acids. 2012;87:111–117.
- Jockel‐Schneider Y, Goßner S, Petersen N, et al. Stimulation of the nitrate‐nitrite‐NO‐metabolism by repeated lettuce juice consumption. J Clin Periodontol. 2016;43:603–608.
- Sen NP. Formation and Occurrence of Nitrosamines in Food. Diet, Nutrition, and Cancer: A Critical Evaluation. Cleveland, Ohio: CRC Press; 2018:135–160.
- Scanlan RA. Nitrosamines. In: The Encyclopedia of Food Sciences and Nutrition. 2nd ed. Cambridge, Massachusetts: Academic Press; 2003:4142–4147.
- World Health Organization. Q&A on the Carcinogenicity of the Consumption of Red Meat and Processed Meat. Available at: who.int/news-room/q-a-detail/q-a-on-the-carcinogenicity-of-the-consumption-of-red-meat-and-processed-meat. Accessed October 28, 2020.
- Fridell S, Ström E, Agebratt C, et al. A randomised study in young subjects of the effects of eating extra fruit or nuts on periodontal inflammation. BDJ Open. 2018;4:1–5.
- Seleshe S, Lee JS, Lee S, et al. Evaluation of antioxidant and antimicrobial activities of ethanol extracts of three kinds of strawberries. Prev Nutr Food Sci. 2017;22:203.
- Stull AJ, Cash KC, Johnson WD, Champagne CM, Cefalu WT. Bioactives in blueberries improve insulin sensitivity in obese, insulin-resistant men and women. J Nutr. 2010:140:1764–1768.
- Silva S, Costa EM, Veiga M, Morais RM, Calhau C, Pintado M. Health promoting properties of blueberries: a review. Crit Rev Food Sci Nutr. 2020;60:181–200.
From Dimensions of Dental Hygiene. November 2020;18(10):36-39.