FATCAMERA/ISTOCK/GETTY IMAGES PLUS
FATCAMERA/ISTOCK/GETTY IMAGES PLUS
Promoting Dental Health For Pets
Excellent oral healthcare will help pets live longer, healthier lives.
This course was published in the November 2020 issue and expires November 2023. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the consequences of oral disease in pets.
- Recognize that pet owners can take an active role to improve the oral health of their pets.
- Describe evidence-based home-care products for cats and dogs to improve oral health.
Dental hygienists advocate and promote oral health for their patients and recognize the systemic effects of periodontal diseases. Dental hygienists can also assist their patients by promoting the oral health of their pets. Pet owners need to recognize that oral disease can have systemic effects on their pet’s overall health. Periodontal diseases are the most common illnesses among dogs and cats. By age 3, 75% of dogs and 60% of cats have some form of oral disease.1 Oral disease can cause pain and affect pets’ quality of life and longevity. Dental hygienists are well-positioned to educate their patients on the signs of dental pain in their pets, as dogs and cats often mask their discomfort. Untreated dental pain in animals can be demonstrated by teeth chattering, weight loss, change in eating habits, lethargy, and change in behavior.1
Periodontal Diseases in Pets
The progression of periodontal diseases in pets is similar to humans, with many modulating factors, such as the type of bacteria present, their ability to infect the host, and the host response. Additionally, other links have been found between periodontal diseases and changes in the kidney, myocardium, and liver in animals.2,3 A study conducted by Glickman et al4 showed a significant association of periodontal diseases in dogs with increased risk for endocarditis and cardiomyopathy. The endocarditis revealed a six-fold increase for dogs with moderate (Stage 3) periodontal disease and no risk in dogs with good periodontal health.4 Another study by Harvey et al5 demonstrated that calculus and periodontal diseases are more severe as dogs age and lose weight. Smaller dogs and toy breeds have smaller mouths and tend to have more severe periodontal diseases compared to larger breeds. Small breed dogs also tend to live longer and, therefore, have more time to develop advanced periodontal disease.5
Feline periodontal disease evolves in a pattern similar to dogs and humans. In one study, researchers found a high prevalence of periodontal inflammation among cats, with 81.6% exhibiting a severe form of tissue damage.6 Prevention should be of the upmost importance with dogs and cats.
Role of Pet Owners
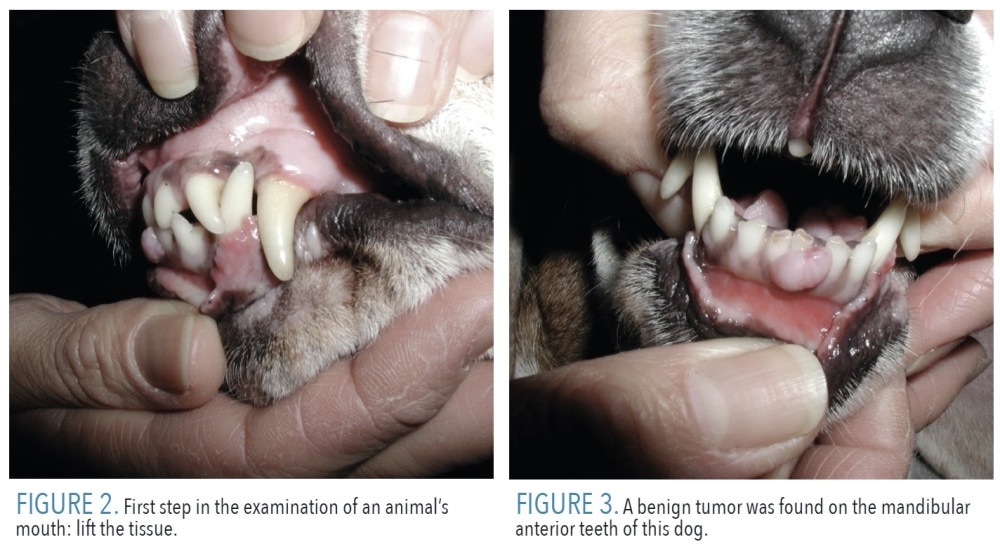
Quality of life is greater with optimal oral health. Pet owners can achieve this with a combination of oral examinations, home care, and professional cleanings. At home, pet owners can positively impact the health of their pets by performing routine oral exams and providing preventive dental care such as toothbrushing. Pet owners should begin by performing an oral exam on their pet at least once every 6 months, looking for inflammation, malocclusion, mobile teeth, eye swelling, tumors, and oral lesions. Figure 1 shows a full-bred Schnauzer that received extractions due to malocclusion (prognathism). The maxillary anterior teeth were occluding into the mandibular anterior teeth, which led to the teeth becoming mobile and eventual extraction of the incisor teeth.
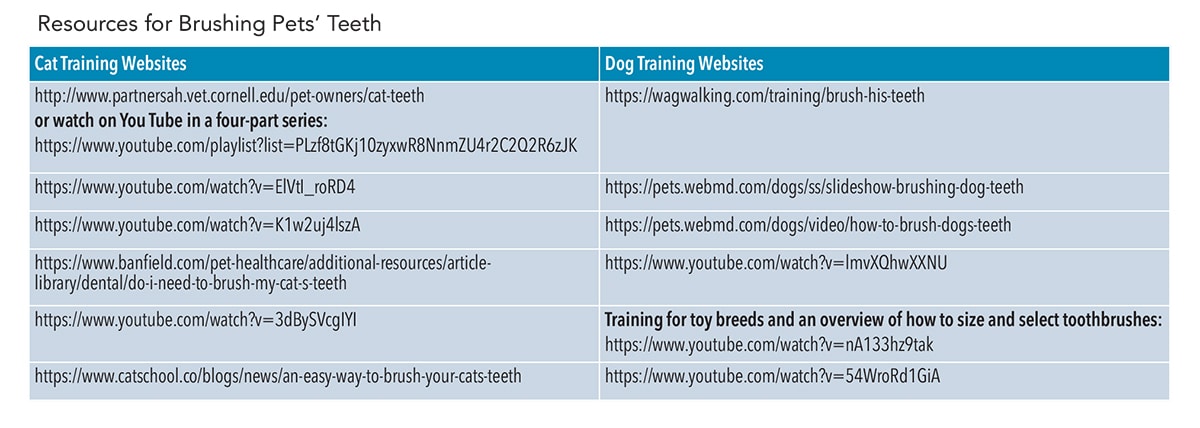
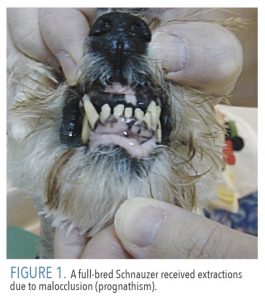
The examination should include the outside of the face and eyes and the inside of the mouth. Figure 2 (page 34) shows the most prudent approach to examining an animal’s mouth. The pet should be approached from the back side of the face and then the tissue should be lifted bilaterally with the index finger and thumb. If the pet is pawing at his or her mouth, not eating well, or licking obsessively, the pet should see a veterinarian. In Figure 3 (page 34), a benign tumor was found on the mandibular anterior teeth of this dog. Also, the apical roots of the canine teeth in cats and dogs are very long, often reaching close to the orbit of the eye. If discharge is noted coming from the eye, the pet’s mouth should be inspected to ensure that it is not caused by an infected tooth.
 Regular professional dental cleanings are also key to achieving optimal health in pets. The procedure involves sedating the pet, followed by hand and power scaling and polishing. Pet owners should be encouraged to discuss any concerns with the veterinarian and ask whether the teeth will be debrided and subgingival and supragingival calculus removed. The term prophylaxis is not used in veterinary tooth cleaning due to the complexity of services provided, but rather “procedure for oral health” is preferred.7
Regular professional dental cleanings are also key to achieving optimal health in pets. The procedure involves sedating the pet, followed by hand and power scaling and polishing. Pet owners should be encouraged to discuss any concerns with the veterinarian and ask whether the teeth will be debrided and subgingival and supragingival calculus removed. The term prophylaxis is not used in veterinary tooth cleaning due to the complexity of services provided, but rather “procedure for oral health” is preferred.7
The procedure for oral health should be done by a trained, credentialed veterinary technician or assistant who is supervised by a veterinarian. Veterinary technician specialist in dentistry is the highest level of certification, with participants completing a rigorous 2-year education process. There are also 4-year baccalaureate degree programs in veterinary technology.
Pet owners should ask that X-rays be taken as well as a full-mouth periodontal probing (six readings per tooth). Normal sulcus depths for a mid-size dog is 2 mm to 3 mm, and 1 mm in cats. Any abnormal findings should be noted in the chart.7
Compliance and Training
If pet owners do not see the value of pet oral healthcare, then dental home care and professional cleanings may not be a priority.8 Besides the challenge of ensuring owners comply with oral health protocols, gaining compliance from the pet may also be difficult. Training pets to comply with oral health treatment takes time and patience. Pet owners should begin regular home care immediately after a professional cleaning, as a toothbrush will not remove calculus. The best way to train animals is to start when they are young. For older pets, training can occur with positive reinforcement and rewards. Pet owners should never put their hands in the mouth of an animal unless they are sure the pet will allow them to do or they are adequately trained. Visit the online version of this article for a table of free online resources for pet training.
During training, choosing a toothbrush that is the correct size for the pet is important. Consider the size of the animal—a bigger toothbrush is better for medium to large dogs while a smaller head, such as a child’s toothbrush, is best for toy breeds. Children’s toothbrushes can be used if they are small enough to get inside the mouth. On a cat or toy dog breeds, a small angled bristle brush is best, as the mouth is small. Dual-ended toothbrushes are ideal, as the handles are long enough to reach posterior teeth, yet the smaller part can clean small anterior incisors. Finger brushes with soft bristles work as well. Toothpaste designed for dogs or cats is best, and those that are flavored and appeal to pets can help in training.
Recommended Products
Veterinarians strongly discourage the use of human toothpaste for dogs and cats because it can cause illness. The fluoride content can upset the pet’s stomach. Instead, they recommend the use of various enzymatic formulas that are made specifically for pets.8 Enzymatic formulas come in a variety of flavors and can help with compliance. Once a pet is trained, the pet owner can begin brushing along the gumline on the facial surfaces by placing the toothbrush on the inside of the cheeks using the Bass technique in circular motion. As the animal becomes more compliant, lingual surfaces can be completed. Studies show that toothbrushing is the most effective home care regimen; however, owner compliance is only about 40% to 50%.7,8
For noncompliant pets, other products, such as dog foods, chews, and rinses, can be tried as adjuncts to home care. Pet dental products make various oral health claims, but they are not regulated by the United States Food and Drug Administration. Also, foods that make oral health benefit claims may not be optimally nutritious.
The Veterinary Oral Health Council (VOHC) was established in 1980—in collaboration with the American Dental Association, American Veterinary Medical Association, and American Veterinary Dental College—to set specific standards for product efficacy. The VOHC sets protocols for clinical studies and has created a system of standards for plaque and calculus removal. Once a product meets the standard, it receives the VOHC seal, meaning the dental product is proven effective. These standards are posted at: vohc.org.9
Evidence-Based Decision Making
Applying the standards of evidence-based decision making is also important in veterinary oral health. The grade I to grade IV system has been proposed for veterinary clinical nutrition, and is useful for recommendations regarding dental home care products.10 Grade I presents the highest quality of evidence with well-controlled randomly designed studies; grade II includes randomized well-controlled studies done in vivo or in vitro; grade III is evidence from controlled studies without randomization, such as cohort or case-control studies; and grade IV evidence presents the weakest evidence, such as studies on other species, descriptive studies, etc. Most of the data reviewed by the VOHC come from grade II studies.9
Using foods or treats with proven dental benefits is appropriate. For a food to provide the best mechanical cleansing, it must promote chewing and make contact for as long as possible with the tooth surface. Also, for safety reasons, all treats should be digestible.
With kibble, there are two mechanisms of action. One is that the kibble must be enlarged with a textural and surface characteristic that inhibits plaque and calculus. The second includes coating the outer surface of the kibble with a polyphosphate, such hexametaphosphate (HMP), so that it will bind salivary calcium and inhibit calculus formation. Some brands use physical and chemical methods in their products.11 One study found that coating dog food or biscuits with sodium HMP provided a 60% to 80% reduction in calculus formation depending on the dosage.12 Another study showed significant reduction of plaque (39%) and gingivitis (36%) when comparing a typical dry dog food to a specifically formulated dental food.13 In cats, dental foods were found to be more effective than toothbrushing for preventing calculus and gingivitis, which is important as research shows that only 40% of pet owners brush their cats’ teeth 6 months after a professional cleaning.14,15 Grade I and grade II evidence supports the use of food to improve oral health, and seven dog foods and five cat foods have earned the VOHC seal.
Dental treats and rawhide chews rely mainly on mechanical abrasion to reduce plaque. In a colony of dogs, a compressed dental chew has been shown to reduce plaque and calculus and improve gingival health.15 A study was conducted on 60 adult male and female dogs that received scaling under anesthesia. After the cleaning, the dogs were assessed for plaque and gingivitis beginning at day 0. None of the dogs had periodontitis. The dogs were then stratified into a test and control group. Results showed a significant reduction in gingivitis (p<0.0001) among the dogs offered the dental chew. Also, significant reductions in oral malodor (p<0.0001) and plaque scores (p=.0.0005) were reported. On day 28, the dogs that were offered the chew had lower calculus scores when compared to the control dogs (p<0.0001). The aim of the study was to emphasize the benefits of oral chews as an adjunct to toothbrushing.16
Rawhides are another form of chew aid that can be used as an adjunct for home care. A study done with soft rawhides on small dogs showed statistically significant reductions in calculus (28%), plaque (19%), and gingivitis (46%).17 Studies on cats have shown similar results. In one study, cats were given a dry diet and dental chews for 4 weeks. Results showed a significant reduction in gingivitis, plaque, and calculus.18 Grade I and grade II evidence exists for the use of specific rawhide chew products for home care. The VOHC website lists two rawhide treats for dogs and none for cats. Also approved, are more than 20 treats in dogs and four treats in cats. Dental chews or treats should be part of a regimen of toothbrushing every day.10
Biscuit treats make many dental claims such as to freshen breath, reduce tartar, or clean teeth. Plain baked treats provide little plaque and calculus reduction in dogs.19 However, the addition of HMP to the surface of a treat reduced calculus accumulation in a research setting.20 Grade I and grade II evidence exists for and against the addition of HMP to reduce calculus accumulation.
The use of chlorhexidine and zinc ascorbate in home-care products may help support pets’ oral health. Chlorhexidine is well studied in humans and is proven to reduce plaque accumulation and gingivitis. Some veterinary products contain chlorhexidine such as rawhide chews, dental gels, oral rinses, and tablets. In one study, dental chews with chlorhexidine inhibited plaque accumulation and significantly reduced gingivitis in dogs.21 Grade II evidence exists for the use of chlorhexidine in dogs. Evidence also shows that it is effective as a pre-operative rinse prior to an oral health procedure22 and for post-operative healing post-cleaning.23
Zinc ascorbate or soluble zinc salts are available in rinses, gels, and toothpaste. In a 6-week study of cats, a zinc ascorbate gel was applied orally to a treatment group while the control group received no oral health products. Results showed a significant decrease in plaque accumulation and gingivitis in anaerobic periodontal pathogens in the treatment group.24 Limited grade I evidence supports the use of zinc ascorbate gel for cats. Zinc salts have been used to control oral malodor in dogs. However, more evidence is needed to support this claim. Some products contain zinc salts and chlorhexidine; however, more evidence is needed to establish efficacy.25
Conclusion
Evidence demonstrates that food, chews, treats, and rinses can reduce plaque and calculus accumulation, thus preventing gingivitis. The regular inspection of pets’ mouths for oral pathology in addition to treatment by a veterinarian are also important. Annual professional cleanings are necessary to ensure good periodontal health. The most effective way to promote pet oral health is by frequently brushing pets’ teeth. Compliance is always an issue whether it be on the part of the pet or the owner. Many factors influence compliance, but the research is clear that owner and pet compliance is critical to effective oral health. All pet owners need to remember that excellent dental care will help pets live longer, healthier lives, and dental hygienists are well prepared to educate their patients on this important topic.
References
- Gorrel C. Veterinary Dentistry for the General Practitioner. Philadelphia: WB Saunders Ltd; 2004.
- DeBowes LJ, Mosier D, Logan E, Harvey C, Lowry S, Richardson D. Association of periodontal disease and histologic lesions in multiple organs from 45 dogs. J Vet Dent. 1996;13:57-60.
- Pavlica Z, Petelin M, Juntes P, DamJan E, Crossley D, Skaleric U. Periodontal disease burden and pathological changes in organs of dogs. J Vet Den. 2008;25:97–105.
- Glickman LT, Glickman NW, Moore GE, Goldstein GS, Lewis HB. Evaluation of the risk of endocarditis and other cardiovascular events on the basis of the severity of periodontal disease in dogs. J Am Vet Med Assoc. 2009;234:486–494.
- Harvey CE, Shofer FS, Laster L. Association of age and body weight with periodontal disease in North American dogs. J Vent Dent. 1994;11:94–105.
- Servet NG, Biourge V, Hennet P. Periodontal health status in a colony of 109 cats. J Vet Dent. 2009;26:147–155.
- Bellows J, Berg M, Dennis S, et al. 2019 AAHA Dental Care Guidelines for Dogs and Cats. J Am Anim Hosp Assoc. 2019;55:1–21.
- Miller BR, Harvey CE. Compliance with oral hygiene recommendations following periodontal treatment in client owned dogs. J Vet Dent. 1994;11:18–19.
- Veterinary Oral Health Council. The VOHC Seal of Acceptance. Available at: vohc.org. Accessed October 28, 2020.
- Roudebush P, Allen TA, Dodd CE, Novotny B. Application of evidence-based medicine to veterinary clinical nutrition. J Am Vet Med Assoc. 2004;224:1765–1771.
- Roudebush P, Logan E, Hale FA. Evidence based veterinary dentistry: a systematic review of homecare for prevention of periodontal disease in dogs and cats. J Vet Dent. 2005;22:6–15.
- Stookey GK, Warrick JM, Miller LL. Effect of sodium hexametaphosphate on dental calculus formation in dogs. Am J Vet Res. 1995;56:913–918.
- Logan E, Finney O, Hefferren JJ. Effects of a dental food on plaque accumulation and gingival health in dogs. J Vet Dent. 2002;19:15–18.
- Miller BR, Harvey CE. Compliance with oral hygiene recommendation following periodontal treatment in client owned dogs. J Vet Dent. 1994;11:18–19.
- Theyse LFH, Vrieling TL, Dijkshoorn NA. A comparative study of 4 dental homecare regimens in client owned cats. Proceedings of the Hills European Symposium on Oral Care. 2003:60–63.
- Bradley W. Oral health benefits of a daily dental chew in dogs. J Vet Dent. 2013;30:84–87
- Stookey G. Soft rawhide reduces calculus formation in dogs. J Vet Dent. 2009;26:82–85.
- Ingham KE, Gorrel C, Bier TL. Effect of a dental chew on dental substrates and gingivitis in cats. J Vet Dent. 2002;19:201–204.
- Logan E, Wiggs R, Zetner K. Dental disease. ln: Hand MS, Thatcher CD, Bemillard RL, Roudebush P. Small Animal Clinical Nutrition. 4th ed. Topeka, Kansas: Mark Morris Institute; 2000:475-492.
- Stookey GK, Warick JM, Miller L, Katz,B. Hexametaphosphate-coated snack biscuits significantly reduce calculus formation in dogs. J Vet Dent. 1996;13:27-30.
- Rawlings JM, Gorrel C, Markwell PJ. Effect on canine oral health of adding chlorhexidine to a dental chew. J Vet Dent. 1998;15:129–134.
- Bowersock TL, Wu CC, Inskeep GA, Chester, TS. Prevention of bacteremia in dogs undergoing dental scaling by prior administration of oral clindamycin or chlorhexidine oral rinse. J Vet Dent. 2000;17:1–16.
- Hennet P. Effectiveness of a dental gel to reduce plaque in beagles. J Vet Dent. 2002;19:11–14.
- Clarke DE. Clinical and microbiological effects of oral zinc ascorbate gel in cats. J Vet Dent. 2001;18:177–183.
- Richard T, Taylor JB, Karwowski J. Pet foods with water-soluble zinc compound coating for controlling malodorous breath. Available at: patents.justia.com/patent/5405836. Accessed October 28, 2020.
From Dimensions of Dental Hygiene. November 2020;18(10):32-35.