 ZLIKOVEC/ISTOCK/GETTY IMAGES PLUS
ZLIKOVEC/ISTOCK/GETTY IMAGES PLUS
Diabetes and Periodontal Diseases
Inflammation is the link that binds these two common maladies.
This course was published in the February 2017 issue and expires February 2020. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the diabetes epidemic.
- Identify the bidirectional link between diabetes and periodontal diseases.
- Explain the role that inflammation plays in diabetes and periodontal diseases.
INTRODUCTION
In April 2013, evidence-based information and recommendations for day-to-day patient management were disseminated in a joint publication of the American Academy of Periodontology (AAP) and the European Federation of Periodontology. The Colgate-Palmolive Company is committed to ensuring that practicing dental professionals have access to the latest educational resources. Hence, we are delighted to have provided an unrestricted educational grant to support the article “Diabetes and Periodontal Diseases”—the first in a series created in collaboration with the AAP. This article provides a useful review of the literature, highlighting the mechanisms behind the bidirectional relationships between diabetes mellitus and periodontal diseases. Dental professionals have a unique opportunity to improve patient outcomes with periodontal disease management and patient education. I hope you find this article to be a valuable resource to help manage the patients with diabetes in your practice.
—Matilde Hernandez,DDS, MS, MBA
Scientific Affairs Manager Professional Oral Care
Colgate Oral Pharmaceuticals
FROM THE AMERICAN ACADEMY OF PERIODONTOLOGY
The link between diabetes and periodontal diseases has been the subject of study for many years, prompting the dental and medical communities to work together in the care of both inflammatory conditions. In 2012, the American Academy of Periodontology (AAP)―in collaboration with the European Federation of Periodontology—released a consensus report on periodontitis and systemic diseases, finding that periodontal health can impact diabetes management and vice versa. The relationship between oral health and overall health grants dental professionals (particularly dental hygienists who perform preventive and nonsurgical care) a responsibility to educate all patients about the bidirectional relationship of diabetes and periodontal diseases and what it means for their risk and treatment. In this article, educator and AAP periodontist Marcelo Freire, DDS, PhD, DMSc, sheds light on the sweeping worldwide incidence of diabetes and its connection to periodontal disease, which affects one of every two United States adults older than 30.
The AAP is proud to work with Dimensions of Dental Hygiene and Colgate-Palmolive to bring you insights that will support your patients’ oral and overall health.
—Terrence J. Griffin, DMD
President, American Academy of Periodontology
Chronic inflammatory diseases, such as diabetes mellitus and periodontal diseases, significantly impact public health. Both conditions influence quality of life, lifespan, and health care costs across the globe. The prevalence of type 2 diabetes and periodontal diseases has increased worldwide.1 According to the International Diabetes Federation, about 415 million adults have diabetes.2 Unfortunately, the current incidence is estimated to increase to 640 million by 2040.2 The prevalence of periodontal diseases is also high, with nearly half of all Americans exhibiting periodontitis.3
In order to adequately treat diabetes and periodontal diseases, clinicians must remain up to date on advancements in basic biology and translational science that guide patient management. Chronic inflammation is the known mechanism that links periodontal diseases and diabetes. The long-term consequences of these associated pathologies include tissue damage, increased disease severity, and extensive treatment. The biological mechanisms behind disease initiation, establishment, and progression are regulated by immune and metabolic interactions. Understanding these complex molecular communications is important for the multidisciplinary team in order to provide optimal treatment options.
DIABETES—A GLOBAL EPIDEMIC
Diabetes is a chronic metabolic condition characterized by hyperglycemia, with defective production of insulin or defective insulin actions. As an essential hormone produced in the pancreas, insulin is required to conduct major biological functions including glucose transport and energy. There are three main types of diabetes: type 1, type 2, and gestational diabetes. Less common types of diabetes are monogenic diabetes, which arises from gene mutations, such as neonatal diabetes mellitus, and secondary diabetes, which is a comorbidity of other diseases, such as Cushing disease.4 Changes in diet and lifestyle and population growth have likely influenced the increase in the prevalence of diabetes worldwide.5
For the first time in history, it is estimated that more than half a million children age 14 and younger are living with type 1 diabetes.6Today, 415 million adults age 20 to 79 worldwide have diabetes, including 193 million individuals who remain undiagnosed.1 A further 318 million adults are estimated to have prediabetes, which puts them at high risk of developing the disease.1

Most patients diagnosed with type 2 diabetes do not require daily insulin treatment to survive. The cornerstone of type 2 diabetes treatment is the adoption of a healthy diet, increased physical activity, and maintenance of a normal body weight. Patients with both types of diabetes need to work closely with their health care team to receive diabetes education, regular checkups, and ongoing support to manage their health.7 Poorly managed diabetes leads to serious complications and early death.
The consequences of high blood sugar levels (hyperglycemia) are immediate and can be lethal. Frequent urination, excessive thirst, weight loss, and blurred vision are common symptoms of both types of diabetes. In type 1, the onset of clinical manifestations is more sudden, while individuals with type 2 may remain in a prediabetic state for years. Many people with type 2 diabetes remain unaware of their condition because the symptoms are usually less noticeable than in type 1 diabetes.8 During this time, however, the body is being damaged by excess blood glucose. As a result, many people already have evidence of complications when they are diagnosed with type 2 diabetes.
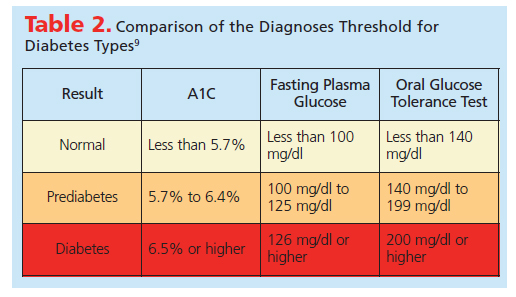
Diabetes diagnosis is mostly based on glucose and insulin levels. The glycated hemoglobin test (HbA1c) measures the blood glucose for 2 months to 3 months, whereas the fasting plasma glucose (FPG) requires 8 hours of fasting. The oral glucose tolerance test checks glucose before and 2 hours after ingestion of a glucose-enriched drink. Table 2 compares the diagnoses threshold for normal, prediabetes, and diabetes.9 Because many individuals stay in a prediabetes state for years before diagnosis, the interdisciplinary team—including oral health professionals—is charged with monitoring glucose values over the long term.
Hospitalization rates for heart attack were 1.8 times higher among adults with diabetes than among adults without diabetes.11Hyperglycemic crisis was the cause of 175,000 emergency department visits for people of all ages in 2011.12 Diabetes is the leading cause of retinopathy and kidney failure, in addition to increasing the chance of stroke by 1.5 times.13 Individuals with diabetes are more likely to experience nerve damage and poor circulation to the feet due to damaged blood vessels. These problems increase the risk of ulceration, infection, and amputation. People with diabetes face a risk of amputation that may be more than 25 times greater than in those without diabetes.14 In fact, cardiovascular diseases are the most common cause of death and disability among people with diabetes.15
BIDIRECTIONAL LINK
The inflammation triggered by diabetes directly impacts periodontal tissues and other organs. The increase of systemic inflammation leads to insulin resistance and reduced pancreatic B-cell function and apoptosis (programmed cell death).16 Periodontitis also contributes to systemic inflammation, and its severity and prognosis is influenced by diabetes-originated inflammation. A potential relationship between inflammatory pathways and metabolic diseases—such as type 2 diabetes and periodontal diseases—remains under scientific investigation.17,18
Recent evidence shows that 47% of adults older than 30 were found to have periodontitis.3 The prevalence of periodontitis was higher in men, Mexican-Americans, and individuals of low socioeconomic status.3 In a more detailed analysis of National Health and Nutrition Examination Survey (NHANES) data, 60% of those with diabetes were found to have moderate to severe periodontitis.19 A World Health Organization survey showed a positive association between periodontal diseases and diabetes, depending on the socioeconomic status of the country.20 It is now clear that the majority of patients with type 2 diabetes present with some form of periodontal diseases.21,22 Increased probing depths and attachment loss were observed in individuals with type 2 diabetes.23 The prevalence of periodontitis is also increased in patients with prediabetes.19
Periodontal diseases, including gingivitis and periodontitis, are inflammatory diseases initiated by microbial biofilms. The etiology of periodontitis is multifactorial, and a number of behavioral, environmental, microbial, systemic, and genetic risk factors influence the host-susceptibility and disease progression. The local acute periodontal inflammatory response is initiated by the challenge posed by microbial biofilm. The dysbiosis (microbial imbalance) of immunome and microbiome is characterized by increased inflammation and elevated expression of pathologic genes/microorganisms, which lead to chronic innate immune response, followed by an acquired immune response that results in tissue destruction or periodontitis.24
Patients with diabetes are at two times to three times greater risk for developing chronic periodontitis than those without diabetes.25Those with chronically elevated HbA1c have a significantly higher prevalence of periodontitis and more tooth loss than those without elevated HbA1c levels.19 While high glucose levels affect periodontal status, acute and chronic infections can also influence glycemic control. Effective treatment of periodontitis can modify glycemic control, as suggested by recent evidence.22, 26–28 As such, nonsurgical periodontal therapy, including scaling and root planing, is important to the diabetes-periodontal disease treatment plan. Maintaining an effective self-care program, including twice-daily brushing with an antimicrobial toothpaste and rinsing with an antimicrobial mouthrinse, is key to controlling the pathogenic bacterial load common among patients with diabetes and periodontal diseases.29,30
As additional studies are published, the impact of periodontal therapy on diabetic control becomes more clear. Recent meta-analyses included studies with at least 3 months of follow-up after periodontal therapy measuring type 2 diabetes outcomes.31 Nine studies found a significant decrease of HbA1c (−0.36% HbA1c; 95% CI −0.66, −0.19) when periodontal maintenance is effective. Reductions of HbA1c have been the standard treatment outcome for diabetes and the development of new treatment modalities, because reducing HbA1c has been shown to delay the onset of diabetic complications. However, there is currently no evidence of a “threshold” for the benefit of reducing HbA1c. To reduce HbA1c levels, metformin is the preferred oral medication in the treatment of patients with type 2 diabetes.32
Approximately 50% of all patients with type 2 diabetes are treated with one or more drugs to achieve metabolic control.33 When considering the effects of periodontal actions on glycemic controls, the treatment or first drug of choice must be considered an additive. Thus the individualized actions of one treatment can be studied in combination with the other. In order, to weigh the clinical relevance of any HbA1c reduction due to periodontal treatment, its impact must be compared with a second drug for example, in addition to metformin. Several drugs have been used as add-on treatments to metformin. The additional reduction of HbA1c over metformin alone was 0.85%, 0.61%, and 0.42% for sulphonylureas, α-glucosidase inhibitors, and thiazolidinediones, respectively.34,35 Thus, if periodontal therapy can improve HbA1c levels by 0.4% to 0.5%, then its effect may be comparable to additional pharmacotherapies and it may find a place in the management protocols for patients with diabetes.
Future randomized clinical trials should include patients who are using different diabetic treatment approaches to determine whether periodontal treatment works equally well in all patients with diabetes, irrespective of drugs used.
CHRONIC INFLAMMATION
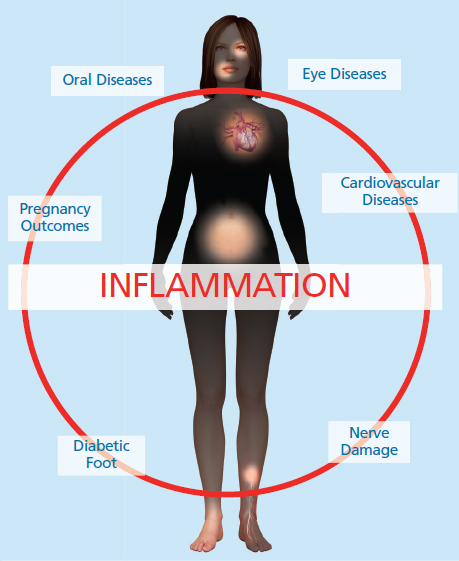
Inflammation is a protective biological response against disease (Figure 1). Patients with diabetes need to understand that part of their treatment goal is to resolve inflammation. Historically, tissue response to injury and infection was first recorded by the ancient Egyptian and Greek cultures. Cornelius Celsus’ studies documented inflammation signs in humans. Four cardinal signs of inflammation were identified: “rubor et tumor cum calore et dolore” (redness and swelling with heat and pain). Loss of tissue function (function laesa) was added as the fifth sign by Rudolph Virchow, a 19th century German pathologist. More recently, advanced cellular and molecular mechanisms governing the fate of inflammation (resolution vs chronicity) have been identified.17–20
Inflammation is an active biological response that aims to maintain health and tissue integrity. It turns on when the host tissue is challenged by pathogens, foreign bodies, or injury. The initial process is characterized by vascular dilation, enhanced permeability of capillaries, and increased blood flow in addition to leukocyte recruitment.36 Polymorphonuclear neutrophils (PMN) are the first cells to accumulate in the inflamed gingival tissue. These cells serve as the first line of defense of the innate immune system due to their phagocytosis and microbicidal functions. Next, mononuclear cells, monocytes, and macrophages enter the inflammatory site and clear cellular debris and apoptotic PMN by phagocytosis (consumption of bacteria by phagocytes and amoeboid protozoans).
While inflammation is protective, chronic activation is detrimental to tissue function. Failure to remove noxious materials via phagocytosis and lymphatic drainage characterizes the initiation of pathological lesion and disease establishment. The incomplete elimination of leukocytes from a lesion is observed in susceptible individuals, such as those with periodontal abscesses and uncontrolled diabetes. A new class of resolution lipid mediators can activate endogenous cells to return to homeostasis (resolvins, lipoxins, protectins, and maresins).18 Accordingly, loss of resolution and failure to return tissue to homeostasis results in neutrophil-mediated destruction and chronic inflammation, which is a major cause of human inflammatory diseases.
CONCLUSION
In summary, unresolved inflammation is a hallmark of various human diseases, including diabetes and periodontitis. Diabetes directly affects periodontal health and disease. Continuous release of cell/bacterial debris and toxins results in local tissue damage, prolonged inflammatory response, and loss of resolution results in the chronic lesion. Emerging evidence suggests oral infections, especially periodontal diseases, are risk factors for initiation and progression of diabetes. There is evidence that periodontal treatment can reduce glycated hemoglobin when periodontal disease is present. A multidisciplinary health care team—including oral health professionals—can effectively address the biological mechanisms behind disease initiation and progression.
ACKNOWLEDGMENTS
The author is supported by National Institute of Dental and Craniofacial Research grant K99/R00DE 0235804. The author would like to thank Thomas E. Van Dyke, DDS, PhD; Corneliu Sima, DMD, DSc, MSc; Erin Breen, DDS; Alaa Ahmed, DMD; and Ana Metzger, MD, PhD.
REFERENCES
- International Diabetes Federation. IDF Diabetes Atlas. Available at: diabetesatlas.org. Accessed January 17, 2017.
- International Diabetes Federation. Facts & Figures. Available at: idf.org/WDD15-guide/facts-and-figures.html. Accessed January 17, 2017.
- Eke PI, Dye BA, Wei L, et al. Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009 to 2012. J Periodontol. 2015;86:611–622.
- National Institute of Diabetes and Digestive Kidney Diseases. Monogenic Forms of Diabetes. Available at: niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/monogenic-neonatal-mellitus-mody. Accessed January 17, 2017.
- Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34:1249–1257.
- Aanstoot HJ, Anderson BJ, Daneman D, et al. The global burden of youth diabetes: perspectives and potential. Pediatr Diabetes. 2007;8(Suppl 8):1–44.
- Centers for Disease Control and Prevention. At a Glance 2016: Diabetes, Working to Reverse the US Epidemic. Available at: cdc.gov/chronicdisease/resources/publications/aag/pdf/2016/diabetes-aag.pdf. Accessed January 17, 2017.
- Guariguata L, Whiting D, Weil C, Unwin N. The International Diabetes Federation diabetes atlas methodology for estimating global and national prevalence of diabetes in adults. Diabetes Res Clin Pract. 2011;94:322–332.
- American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care. 2015;38(Suppl):S8–S16.
- Franklin JE. Confronting the urgent challenge of diabetes: an overview. Health Affairs. 2012;31:12–19.
- American Diabetes Association. Statistics About Diabetes. Available at: diabetes.org/diabetes-basics/statistics. Accessed January 17, 2017.
- Wang J, Geiss LS, Williams DE, Gregg EW. Trends in emergency department visit rates for hypoglycemia and hyperglycemic crisis among adults with diabetes, United States, 2006-2011. PLoS One. 2015;10:e0134917.
- American Diabetes Association. Stroke. Available at: diabetes.org/living-with-diabetes/complications/heart-disease/stroke.html. Accessed January 17, 2017.
- International Diabetes Federation. Complications of Diabetes. Available at: idf.org/complications-diabetes. Accessed January 17, 2017.
- Kreatsoulas C, Anand SS. The impact of social determinants on cardiovascular disease. Can J Cardiol. 2010;26(Suppl C):8C–13C.
- Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–867.
- Van Dyke TE, Kornman KS. Inflammation and factors that may regulate inflammatory response. J Periodontol.2008;79:1503–1507.
- Freire MO, Dalli J, Serhan CN, Van Dyke TE. Neutrophil resolvin E1 receptor expression and function in type 2 diabetes. J Immunol. 2017;198:718–728.
- Preshaw PM, Alba AL, Herrera D, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55:21–31.
- Petersen PE, Ogawa H. Strengthening the prevention of periodontal disease: the WHO approach. J Periodontol.2005;76:2187–2193.
- Pranckeviciene A, Siudikiene J, Ostrauskas R, Machiulskiene V. Long-term effect of periodontal surgery on oral health and metabolic control of diabetics. Clin Oral Investig. April 11, 2016. Epub ahead of print.
- Faggion CM Jr, Cullinan MP, Atieh M. An overview of systematic reviews on the effectiveness of periodontal treatment to improve glycaemic control.J Periodontal Res. 2016;51:716–725.
- Spangler L, Reid RJ, Inge R, et al. Cross-sectional study of periodontal care and Glycosylated Hemoglobin in an insured population. Diabetes Care. 2010;33:1753–1758.
- Herrera BS, Hasturk H, Kantarci A, et al. Impact of resolvin E1 on murine neutrophil phagocytosis in type 2 diabetes. Infect Immun. 2015;83;792–801.
- Negrato CA, Tarzia O, Jovanovič L, Chinellato LE. Periodontal disease and diabetes mellitus. J Appl Oral Sci. 2013;21:1–12.
- Teeuw WJ, Gerdes VEA, Loos BG. Effect of periodontal treatment on glycemic control of diabetic patients: A systematic review and meta-analysis. Diabetes Care. 2010;33:421–427.
- Singh S, Kumar V, Kumar S, Subbappa A. The effect of periodontal therapy on the improvement of glycemic control in patients with type 2 diabetes mellitus: A randomized controlled clinical trial. Int J Diabetes Dev Ctries. 2008;28:38–44.
- Janket SJ, Wightman A, Baird AE, Van Dyke TE, Jones JA. Does periodontal treatment improve glycemic control in diabetic patients? a meta-analysis of intervention studies. J Dent Res. 2005;84:1154–1159.
- Prasanth M. Antimicrobial efficacy of different toothpastes and mouthrinses: an in vitro study. Dent Res J (Isfahan).2011;8:85–94.
- Riley P, Lamont T. Triclosan/copolymer containing toothpastes for oral health. Cochrane Database Syst Rev. 2013;12:CD010514.
- Engebretson S, Kocher T. Evidence that periodontal treatment improves diabetes outcomes: a systematic review and meta-analysis. J Periodontol. 2013;84:S153–S169.
- Glick M. The Oral-Systemic Health Connection. Hanover Park, Illinois: Quintessence; 2014:301.
- García-Pérez L-E, Álvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013;4:175–194.
- Lam KS, Tiu SC, Tsang MW, Ip TP, Tam SC. Acarbose in NIDDM patients with poor control on conventional oral agents. Diabetes Care. 1998;21:1154–1158.
- Lin BJ, Wu HP, Huang HS, et al. Efficacy and tolerability of acarbose in Asian patients with type 2 diabetes inadequately controlled with diet and sulfonylureas. J Diabetes Complications. 2003;17:179–185.
- Spranger J, Kroke A, Mohlig M, et al. Inflammatory cytokines and the risk to develop type 2 diabetes: results of the prospective population-based European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Diabetes. 2003;52:812–817.
From Dimensions of Dental Hygiene. February 2017;15(2):37-42.



