Addressing Elder Abuse
Dental hygienists are well positioned to note the signs and symptoms of this increasingly common form of mistreatment among older adults.
This course was published in the May 2015 issue and expires May 31, 2018. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the types of elder abuse.
- List the risk factors for this type of mistreatment.
- Provide a profile of elder abuse perpetrators.
- Discuss the role of dental hygienists in reporting elder abuse.
Dental hygienists’ expertise is not limited to oral health, but rather includes a broad-based knowledge of overall risk assessment, detection of signs and symptoms of disease, and strategies to improve both oral and systemic health. They are often the most frequently visited health care professionals, as many Americans keep 3-month to 6-month recare appointments with their dental providers but don’t routinely visit their primary care physicians. As such, dental hygienists and other members of the oral health care team are well positioned to recognize the signs of abuse and, therefore, should be prepared to provide assistance to patients exhibiting these types of symptoms.
While abuse is present among all populations, the growing number of aging adults in the United States indicates that elder abuse is an important social problem that should be addressed. According to the US Census Bureau, the number of older adults has tripled since 1900.1 In the early 20th century, individuals age 65 and older constituted 4.1% of the American population; in 2010, they accounted for 13%.1 This upward trend highlights the fact that health issues related to aging, including elder abuse, need to be at the forefront of health care and social services planning moving forward.2
The fastest growing population among older adults is those age 85 and older.1 This trend is significant because this age group tends to be especially vulnerable and, therefore, may be at increased risk of abuse or neglect.1
DEFINITIONS OF ELDER ABUSE
There is no consistent definition of elder abuse in the US, as each state defines elder abuse according to its own laws and regulations. Therefore, the parameters for each category of abuse may differ from state to state.3 Gibbs and Mosqueda4 define elder abuse as the “actions or lack of actions that harm an older adult or put him or her at risk of harm, which may be physical, emotional, and/or financial.” The National Center on Elder Abuse (NCEA), which is part of the US Department of Health and Human Services’ Administration on Aging, describes elder abuse as “mistreatment that is committed by someone with whom the elder has a special relationship (spouse, sibling, child, friend, or caregiver).”3
Assessing the prevalence of elder abuse is challenging, partly due to the absence of a universally accepted definition.4 As more older adults continue to live in their homes and depend on others for assistance, the risk of elder abuse will likely increase. The New York State Elder Abuse Prevalence Study2 found that for every case of elder abuse reported, another 23 go unreported. Elder abuse can happen to anyone in any community regardless of race/ethnicity, gender, or socioeconomic status.5
According to the Administration on Aging, approximately 96% of older Americans live in the community, with many residing in their own homes, while less than 5% are institutionalized in long-term care facilities.5 Older adults’ level of independence depends on their ability to care for themselves. Some seniors may need help with activities of daily living, which may be provided by family members, friends, or home health care aides. Others may experience cognitive impairments that necessitate more involved assistance.6
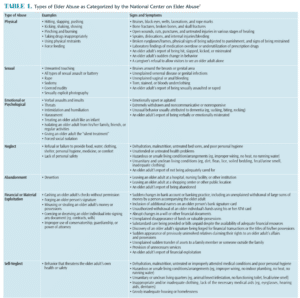
TYPES OF ELDER ABUSE
There are several types of elder abuse, including physical, sexual, emotional/psychological, neglect, abandonment, financial or material exploitation, and self-neglect. Table 1 provides examples of each type of abuse, as well as its signs and symptoms.7
Elder abuse often goes unreported due, in part, to the lack of proper screening methods within the health care continuum.8 Identifying abuse in older adults can be challenging due to the following factors:
- Older adults are frail and heal slowly, making it difficult to accurately assess suspected injuries caused by abuse9,10
- Most abusers are family members whom victims may be reluctant to turn in3
- Victims may feel embarrassed or ashamed
- Physical and/or cognitive barriers to reporting abuse
- Fear of abandonment by the abuser who may be the victim’s main caregiver
- Authority figures are not able to recognize the signs and symptoms11
The National Elder Mistreatment Study12 conducted in 2010 analyzed data from 5,777 individuals age 60 or older to determine the prevalence of emotional, physical, and sexual abuse, as well as financial mistreatment and potential neglect. The authors found that the prevalence rates for abuse experienced within the past year were 4.6% for emotional abuse, 1.6% for physical abuse, 0.6% for sexual abuse, 5.1% for potential neglect, and 5.2% for current financial abuse by a family member.12 The results equated to one in 10 study participants reporting emotional, physical, or sexual abuse or neglect within the past year.12 The authors concluded that little social support and previous exposure to trauma were the most common indicators that abuse would occur.
Financial or material exploitation is the fastest growing form of elder abuse. The 2011 MetLife Study of Elder Financial Abuse: Crimes of Occasion, Desperation, and Predation Against America’s Elders13 found that older adult victims of financial mistreatment experienced losses of more than $2 billion in 2010. This number was 12% higher than previous data gathered in 2008. Financial exploitation includes theft, fraud, and misuse of assets.14
RISK FACTORS![Elder Abuse Victim Profile]()
Clinicians who have a thorough understanding of the risk factors involved in elder abuse will be better prepared to help address elder abuse/mistreatment. Research shows that the characteristics of both victims and abusers can predict the occurrence of different types of elder abuse.15 The following risk factors are associated with victims of elder abuse: physical impairment, mental health problems, cognitive impairment, depression, and inadequate social support.16,17 Cognitively impaired older adults are at increased risk of abuse because they may not be able to recognize the signs of abuse or communicate them.16 Table 2 provides a profile of elder abuse victims.
ELDER ABUSE PERPETRATORS
Elder abuse perpetrators frequently lack social support and are likely to experience problems with interpersonal relationships.16 The House of Representatives Select Committee on Aging found that in more than two-thirds of substantiated cases, the perpetrator is a family member in a caregiving role—usually an adult child.16 The report also noted that men were more likely to become abusers than women. Family members with a history of substance abuse and/or mental/emotional illness, as well as those who felt overwhelmed by their caregiver role were most likely to become abusers.16 Table 3 provides the characteristics of elder abusers.
THE ROLE OF DENTAL HYGIENISTS![Elder Abuse Perpetrator Profile]()
As health care providers, it is important to notice red flags that may indicate the possibility of elder abuse among patients, such as unexplained injuries; changes in behavior (eg, becoming withdrawn, aggressive, or irritable); untreated health problems or malnutrition/dehydration; and patients noting they are no longer in control of their own finances.18 Identifying these symptoms are key to recognizing and reporting elder abuse.
When a clinician suspects elder abuse, he or she must decide whether to notify authorities immediately. This critical judgment should be made based on the patient’s physical and mental condition. A reasonable suspicion is all that is needed to make a report. Available in all 50 states, Adult Protective Services (APS) is a state government entity whose key responsibilities include receiving reports of alleged elder abuse, investigating allegations, determining whether the alleged abuse is substantiated, and, if needed, arranging for services to ensure victims’ well-being.19 Some of the services provided by APS include medical, social, legal, financial, housing, and other resources to ensure the health and safety of those in need.3 The APS process for addressing any allegation of elder abuse differs from state to state.20 Even if abuse is not substantiated, a call to APS can lead to the implementation of supportive measures to ensure the older adult can live safely at home.16 To find a state’s APS phone number, visit eldercare.gov or call (800) 677-1116.
Laws concerning who is legally required to report suspected elder abuse differ by state, as do the criteria for obtaining services.16 Clinicians should become familiar with the relevant laws in the state in which they practice.
CONCLUSION
Dental hygienists have a duty to protect their patients from harm. As the older adult population increases, more individuals will be at risk for elder abuse. As such, it is important to understand the complexities, signs, symptoms, and risk factors for this type of mistreatment. Dental hygiene services are often provided when patients are separated from their caregivers, which provide the opportunity to engage with patients and learn more about their lives. Dental hygienists are well positioned to ask nonthreatening questions if suspicions are aroused and to observe the dynamic between caregiver and patient. It is important to note that a suspicion of abuse is all that is necessary to make a report to APS. Elder abuse is a growing societal problem that should be addressed with education, awareness, and outreach so the cycle of abuse can be thwarted.
REFERENCES
- United States Census Bureau. The Older Population: 2010. Available at: census.gov/prod/ cen2010/briefs/c2010br-09.pdf. Accessed April 15, 2015.
- Lifespan of Greater Rochester Inc. Under the Radar: New York State Elder Abuse Prevalence Study. Available at: ocfs.ny.gov/main/reports/Under%20 the%20Radar%2005%2012%2011%20final%20report.pdf. Accessed April 15, 2015.
- National Center on Elder Abuse. Frequently Asked Questions. Available at: ncea.aoa.gov/faq/index.aspx. Accessed April 15, 2015.
- Gibbs L, Mosqueda L. Elder abuse: a medical perspective. Aging Health. 2010;6(6):739–747.
- US Department of Health, Administration on Aging. A Profile of Older Americans: 2012. Available at: aoa.gov/Aging_Statistics/Profile/2012/docs/ 2012profile.pdf. Accessed April, 15, 2015.
- The President’s Council on Bioethics. Taking Care: Ethical Caregiving in our Aging Society. Available at: bioethicsarchive.georgetown.edu/pcbe/reports/taking_care/chapter1.html. Accessed April 15, 2015.
- National Center on Elder Abuse. Types of Abuse. Available at: ncea.aoa.gov/FAQ/Type_Abuse/ index.aspx. Accessed April 15, 2015.
- Bonnie RJ, Wallace RB, eds. Elder Mistreatment: Abuse, Neglect, and Exploitation in an Aging America. Washington, DC: National Academies Press; 2003.
- McAndrew M, Marin MZ. Role of the dental professional in the identification and referral of victims of domestic violence. NY State Dent J. 2012;78:16–20.
- Love C, Gerbert B, Caspers N, Bronstone A, Perry D, Bird W. Dentists’ attitudes and behaviors regarding domestic violence. The need for an effective response. J Am Dent Assoc. 2001;132:85–93.
- New York State Elder Abuse Training Manual. New York: Lifespan of Greater Rochester Inc; 2011.
- Acierno R, Hernandez MA, Amstadter AB, et al. Prevalence and correlates of emotional, physical, sexual, financial abuse and potential neglect in the United States. Am J Public Health. 2010;100:292–297.
- MetLife. The MetLife Study of Elder Financial Abuse: Crimes of Occasion, Desperation, and Predation Against America’s Elders. Available at: metlife.com/assets/cao/mmi/publications/studies/2011/mmi-elder-financial-abuse.pdf. Accessed April 15, 2015.
- Jackson SL, Hafemeister TL. Elder financial exploitation vs. hybrid financial exploitation co-occurring with physical abuse and/or neglect. Psychol Violence. 2012;2:285–296.
- Jackson SL, Hafemeister TL. Risk factors associated with elder abuse: the importance of differentiating by type of elder maltreatment. Violence Vict. 2011;26:738–757.
- US Government Accounting Office. Elder Justice: Stronger Federal Leadership Could Enhance National Response to Elder Abuse [Reissued on March 22, 2011]. Available at: gao.gov/products/GAO-11-208. Accessed April 15, 2015.
- Beach SR, Schulz R, Castle NG, Rosen J. Financial exploitation and psychological mistreatment among older adults: differences between African Americans and non-African Americans in a population-based survey. Gerontologist. 2010;50:744–757.
- Boland B, Burnage J, Chowhan H. Safeguarding adults at risk of harm. BMJ. 2013;346:2716.
- National Center on Elder Abuse. Adult Protective Services. Available at: ncea.aoa.gov/Stop_Abuse/ Partners/APS/index.aspx. Accessed April 15, 2015.
- O’Neill L, Vermeal R. Elder Care: A Resource for Interprofessional Providers. The Portal of Geriatrics Online Portal; 2014.
From Dimensions of Dental Hygiene. May 2015;13(5):61–64.





