Treat Teething Pain Safely
The use of benzocaine in infants and children can raise the risk of methemoglobinemia—a dangerous and sometimes fatal condition.
Every mother of a newborn baby is deprived of one thing—sleep. When faced with an uncomfortable, teething infant, a good night’s rest is not always an option. For many years, over-the-counter topical anesthetics to soothe sore gums have been a mother’s best friend, but according to recent advisories from the federal Food and Drug Administration (FDA), these commonly used products could also be their worst enemy. Topical anesthetics for infants and children are now under scrutiny because of their association with methemoglobinemia—a rare but dangerous condition that can be induced by some types of anesthetics.
BENZOCAINE BASICS
Benzocaine is an ester local anesthetic found in numerous over-the-counter medications. Typically, oral numbing gels formulated for infants and children contain 7.5% benzocaine. 1–3 Topical anesthetics are used professionally and over-the-counter every day for minor oral irritations. They are easily applied directly on the tissues of the oral cavity and can penetrate 2 mm to 3 mm beneath the mucosal tissue surface, affecting free nerve endings. Benzocaine is the most commonly used agent in topical anesthetics because it is water insoluble and remains at the site of application, keeping the area numb for a significant amount of time.2 While topical anesthetics provide significant benefits, they do exert negative side effects that may be more pronounced in children. In 2006, the FDA published an alert warning the public that benzocaine can cause a potentially deadly condition called methemoglobinemia.1 Since this alert, 29 additional cases of benzocaine-induced methemoglobinemia have been reported. Of these adverse events, 19 affected children and 15 occurred in those younger than 2 years.1 The FDA issued an additional warning about the use of topical anesthetics in 2011.1
DESCRIPTION OF METHEMOGLOBINEMIA
Methemoglobinemia is a blood disorder in which too much methemoglobin is generated. While methemoglobin cannot release oxygen, it is a type of hemoglobin—the molecule in red blood cells that carries oxygen to the body. When methemoglobinemia occurs, the hemoglobin is prevented from releasing oxygen effectively to body tissues.
There are two different types of methemoglobinemia: acquired and hereditary.4 The majority of methemoglobinemia cases are acquired.5 The hereditary form results from a genetic defect in red blood cell metabolism or hemoglobin structure.6 Acquired methemoglobinemia is triggered by exposure to certain toxins or medications, such as benzocaine, which induce the formation of methemoglobin.7 It is impossible to predict who is susceptible to developing methemoglobinemia after the use of benzocaine and there is a fine line between administering enough to generate a therapeutic effect and giving too much, causing toxicity.8 Hemoglobin is a protein within the blood that transports oxygen throughout the bloodstream (Figure 1). When the body experiences a negative reaction to benzocaine, the ferrous iron that is contained in hemoglobin oxidizes to ferric iron. The iron in hemoglobin must be in the ferrous state in order for oxygen to bind to the protein.
This then changes the essential hemoglobin to methemoglobin. Once the methemoglobin is formed, the hemoglobin loses its vital ability to transport oxygen.9 Methemoglobin is always in the blood but consists of less than 1% of the total hemoglobin.7 As the methemoglobin levels in the body rise, the more serious the condition becomes. Although methemoglobinemia is rare, if left untreated it can lead to severe cardiopulmonary compromise or even death.10

Toxins are able to oxidize the hemoglobin to methemoglobin in several different ways including direct oxidation of hemoglobin, indirect oxidative pathways, and metabolic activation. Benzocaine is an oxidizer and reacts directly with hemoglobin to change its form.9 Infants are most susceptible to this complication because fetal hemoglobin is much easier to oxidize than adult hemoglobin.6 Fetal hemoglobin does not mature into adult hemoglobin until approximately 6 months of age.11 Infants start teething between 3 months and 7 months, just as immature hemoglobin is easily oxidized.6 Also, the primary protective mechanism against oxidization of hemoglobin, nicotinamide adenine dinucleotide (NADH), is not fully matured until infants pass the 4-month mark. NADH is the enzyme in the blood responsible for converting methemoglobin back to hemoglobin.5
SYMPTOMS
The severity of methemoglobinemia symptoms is determined by the level of methemoglobin in the body.12 Central cyanosis, a distinct manifestation of methemoglobinemia, is a condition where the lips, skin, and nail beds turn a pale blue due to a decrease of oxygen in the blood. This occurs when methemoglobin levels reach 15%. Once methemoglobin levels grow to more than 30%, symptoms such as nausea, weakness, and vomiting occur. As levels reach 50%, seizure or coma may result. Finally, if methemoglobin levels surpass 70%,
death is likely.7 Blood taken from someone with methemoglobinemia has a chocolate brown color due to central cyanosis.10 Other symptoms include shortness of breath, fatigue, confusion, headache, and rapid heart rate. Symptoms are likely to occur anywhere from 20 minutes to 60 minutes after exposure to the causative agent.13 Methemoglobinemia is unpredictable and can occur after the very first exposure to benzocaine or following countless safe uses of the local anesthetic.1
WHAT TO DO IN A BENZOCAINE EMERGENCY
The most important step in preventing death due to methemoglobinemia is to recognize the symptoms early. The sooner the condition is treated, the better the outcome. Methemoglobinemia is a medical emergency and warrants a 911 call upon discovery of symptoms. When methemoglobinemia is confirmed by a medical professional, emergency treatment focuses on improving oxygen delivery. The oxidant—methylene blue—which converts the methemoglobin back to hemoglobin, is administered intravenously. Normal levels of methemoglobin should be reached within 1 hour after methylene blue is given. If normal levels are not achieved by this time, a second dose should be administered. Methylene blue treatment can be continued once every 4 hours until the appropriate levels are reached and the hemoglobin is back to normal.7 Most cases of methemoglobinemia are resolved completely within 24 hours to 72 hours after diagnosis.
ADDITIONAL CAUSES OF METHEMOGLOBINEMIA
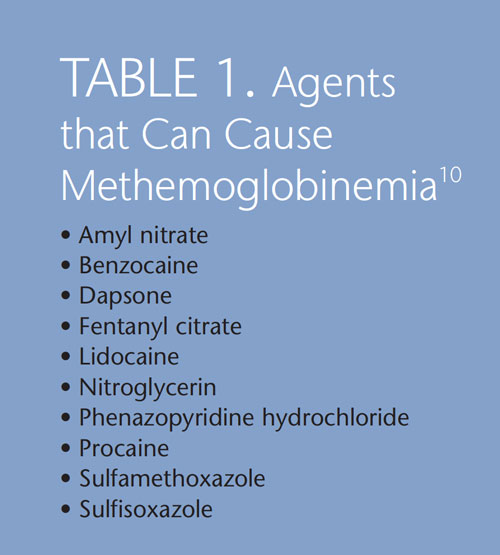
Benzocaine is not the only agent capable of oxidizing hemoglobin, but it is the topical anesthetic most commonly used in children. But any agent in the “caine” family can cause methemoglobinemia when given in excessive doses or mixed with another drug (Table 1).10 Therefore it is vital to record all medications or substances taken before any local anesthetics are administered.8 Additional products capable of inducing methemoglobinemia include acetanilide, aniline dyes, antimalarial agents, flutamine, and phenytoin. Several of these agents are thought to oxidize hemoglobin indirectly by forming oxygen-free radicals while hemoglobin is broken down rather than due to direct exposure to the chemical itself.10
ALTERNATIVES TO TOPICAL ANESTHETICS
Safe and effective alternative methods are available to ease teething discomfort. Gentle massage of the gums with a clean finger can ease teething pain. Chilled, but not frozen, food and teething rings may decrease discomfort. Even a cold washcloth for the baby to chew on can bring teething relief. The American Academy of Pediatrics recommends cold objects over benzocaine products as the safest method of treating teething pain because of the risk of methemoglobinemia.14 With a pediatrician’s approval, over-the-counter children’s pain relievers can be used, particularly at bed time. Natural alternatives containing plant derivatives, for instance eugenol from cloves (Baby Orajel Naturals) may also be helpful.15 If benzocaine anesthetics must be used for infants, they need to be applied in the smallest amount possible and not more than four times per day.16
PATIENT EDUCATION
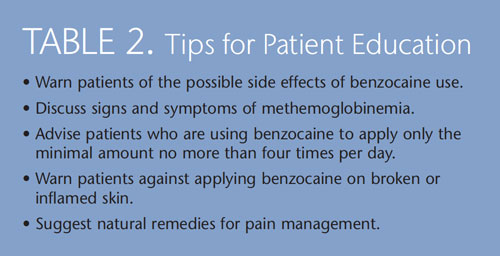
Educating the public about potentially harmful side effects of over-the-counter topical anesthetic products is important. Providing anticipatory guidance—informing patients about possible challenges particularly in regards to child development—is essential. 17 Dental hygienists should address the risk of methemoglobinemia with their patients, especially pregnant women, parents, and caregivers (Table 2). Because of the unpredictable effects that can arise at any time, prompt detection and treatment can be lifesaving.4
REFERENCES
- US Food and Drug Administration. Babies and benzocaine: not a good mix.Available at: www.fda.gov/ForConsumers/ConsumerUpdates/ucm306062.htm.Accessed January 14, 2013.
- Stanley FM. Handbook of Local Anesthesia. 5th ed. St. Louis: Elsevier Mosby;2004:75–76.
- Bong CL, Hilliard J, Seefelder C. Severe methemoglobinemia from topical benzocaine 7.5% (Baby Orajel) use for teething pain in a toddler. Clin Pediatr(Phila). 2009;48:209–211.
- Bittmann S, Krüger C. Benzocaine-induced methaemoglobinaemia: a casestudy. Br J Nurs. 2011;20:168–170.
- Lee DC, Ferguson KL, Kreplick LW, VanDeVoort JT, Burns MJ, Halamka JD. Methemoglobinemic in emergency medicine. Medscape Reference. 2011.Available at: emedicine.medscape.com/article/815613-overview. AccessedJanuary 14, 2013.
- Rehman HU. Methemoglobinemia. West J Med. 2001;175:193–196.
- Nguyen ST, Cabrales RE, Bashour CA, et al. Benzocaine-induced methemoglobinemia. Anesth Analg. 2000;90:369–371.
- Guay J. Methemoglobinemia related to local anesthetics: a summary of 242episodes. Anesth Analg. 2009;108:837–845.
- Haymond S, Cariappa R, Eby CS, Scott MG. Laboratory assessment of oxygenation of methemoglobinemia. Clin Chem. 2005;51:434–444.
- Birchem SK. Benzocaine-induced methemoglobinemia during transesophageal echocardiography. J Am Osteopath Assoc. 2005;105:381–384.
- Kumar S. What is the difference between adult and fetal haemogloin?Doctor NDTV. Available at: doctor.ndtv.com/faq/ndtv/fid/12035/What_is_the_difference_between_adult_and_fetal_haemoglobin.html. Accessed January 14,2013.
- Kwok S, Fischer JL, Rogers JD. Benzocaine and lidocaine induced methemoglobinemia after bronchoscopy: a case report. J Med Case Rep.2008;23:16.
- Sachdeva R, Pugeda JG, Casale LR, Meizlish JL, Zarich SW. Benzocaine induced methemoglobinemia: a potentially fatal complication of transesophageal echocardiography. Tex Heart Inst J. 2003;30:308–310.
- American Academy of Pediatrics. Teething care and anticipatory guidance.Available at: www2.aap.org/ORALHEALTH/pact/ch2_sect5.cfm. AccessedJanuary 14, 2013.
- Rosen MM. Safe baby teething remedies. Parenting. Available at:www.parenting.com/gallery/baby-teething-remedies?pnid=376566. AccessedJanuary 14, 2013.
- American Dental Association. FDA warns of benzocaine complications in teething gels. Available at: www.ada.org/news/5731.aspx. Accessed January14, 2013.
- Brazelton TB, Sparrow J. The touch points model of development.Available at: www.battlecreekenquirer.com/assets/pdf/A51821211122.pdf.Accessed January 14, 2013.
From Dimensions of Dental Hygiene. February 2013; 11(2): 30–32.

