Three-Dimensional Imaging
Cone-beam computed tomography can offer improved diagnosis capability in the dental office, but it must be used prudently.
This course was published in the June 2013 issue and expires June 2016. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define cone-beam computed tomography (CBCT) and how it works.
- Identify the advantages of using CBCT.
- List the limitations of CBCT imaging.
Over the past few years, radiographic imaging in dentistry has evolved from a conventional, two-dimensional technique into a three-dimensional modality. Cone-beam computed tomography (CBCT) was first introduced in Europe in 1998, later arriving in the United States in 2001.1 CBCT now serves as an influential clinical tool in the diagnosis of various oral health problems. As the technology has improved, CBCT has become an effective imaging device that produces three-dimensional imaging in any plane where visualization of the oral and maxillofacial structures is necessary. As the use of this technique continues to grow in the private practice setting, dental professionals should be educated about its uses and how the resultant images can be incorporated into treatment planning.
TECHNOLOGY
CBCT uses a cone-beam-shaped X-ray source and a two-dimensional flat panel detector. Once the subject is positioned in the machine, a single rotation is made around the patient and a complete scan is produced. A cone-beam scanner uses a cone-shaped beam and a reciprocating detector that rotates around the patient 360° and acquires between 150 and 1,599 projected images.2 The complete scanning time ranges from 5 seconds to 40 seconds, depending on the type of unit and settings.1
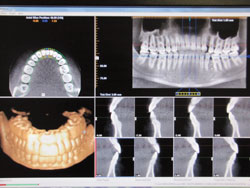
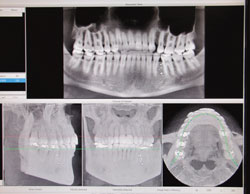
After scanning is complete, these incomplete images are processed by reconstruction to produce digital images in the form of units called voxels. The smallest subunits of digital images, voxels have equal parameters in all three dimensions and are stacked in rows and columns.1 They are then interpreted by software and organized to produce a three-dimensional image from different perspectives (Figure 1 and Figure 2). With these data, the qualified health care provider can then access and visualize the information as reconstructed images. All other parameters of digital imaging, such as brightness, contrast, and hue, can be adjusted for an optimal view of the processed image.3
ADVANTAGES
Less time is required to produce a CBCT scan than a routine CT scan. The CBCT image only requires a single rotation of the X-ray source during which all of the needed images are procured. The time needed to acquire an image is less than 1 minute, but the reconstruction of the image can take up to 20 minutes, although most do not need that much time.4
Because CBCT scans take less time to capture than CT scans, the radiation dose emitted in CBCT imaging is also decreased. A full-field view of a CBCT image requires a radiation dose of 29 ?Sv to 477 ?Sv.4 The use of CBCT imaging reduces radiation emission from 1.3% to 22.7% compared to a conventional CT scan.4
Another advantage of CBCT imaging is its accuracy. Through the voxel resolution, the technique is able to produce accuracy in all dimensions of the image. CBCT’s collimation enables the X-ray beam to be focused only on the areas of interest. Therefore, the optimal level of radiation frequency can be selected depending on what needs to be imaged.4 CBCT also produces images in all three planes of space, which is not possible in intraoral or panoramic radiographs or cephalograms. Measurement algorithms, such as scaling and zooming, allow the clinician to highlight anatomic areas required for diagnosis.4
LIMITATIONS
There are certain limitations to using CBCT, including a lack of clarity with some images. Also, many pathologies can still be detected through the use of conventional radiographs, thus reducing the need for CBCT imaging. Although radiation exposure is less than a conventional CT scan, CBCT imaging still exposes the patient to more radiation than a full-mouth series of radiographs. The clarity of CBCT images is affected by artifacts, which are radiographic factors from the CBCT unit that contribute to loss of detail and lead to a grainy appearance of the image, or noise, and poor soft tissue contrast.5
Artifacts are the distortions of images that are not present and are not related to the subject. They are categorized into patient-related artifacts, scanner-related artifacts, and cone-beam-related artifacts. They can be reduced by collimation, modified patient positioning, separation of dental objects, and introducing certain algorithms.5
The movement of a patient during scanning can lead to both decreased sharpness and increased distortion of images. These errors can be reduced by implementing a shorter scanning time and by using a head restraint. Also, metallic objects or dental restorations in the patient can cause the visualization of streak artifacts on the image. Poor calibration and scanner detection imperfection can lead to a circular or ring-shaped artifact being imposed on the image. Cone-beam related artifacts are due to improper image processing and image reconstruction errors using voxels that result in streaking artifacts, image distortions, and noise.5,6
APPLICATIONS
The initial use of CBCT was confined to surgical assessment of oral and maxillofacial pathologies and reconstruction. Later, the uses of CBCT were expanded to other specialties in dentistry including: orthodontics, endodontics, caries detection, implant diagnosis, temporomandibular joint (TMJ) assessment, preoperative and post-operative assessment of craniofacial fractures, salivary gland imaging, and periodontics. While CBCT can be used in these instances, it is not always the primary choice. The use of CBCT is not a replacement modality for routine two-dimensional radiographs, and should only be utilized when two-dimensional radiographs cannot provide an accurate diagnosis.
ORTHODONTICS
CBCT provides a clear distinction between soft tissue of the pharynx and the airway space for a clear volumetric analysis. Airway analysis is an important factor while providing orthodontic treatment to analyze craniofacial growth patterns. Other uses of CBCT in orthodontics can include locating impacted teeth, determining cortical plate location with regards to root position and torque, and locating a temporary anchorage device after it’s been placed. CBCT imaging can also be used with computer software for enhanced analysis of a patient’s treatment and decreased orthodontic treatment time. An orthodontist can also relate the occlusal plane of view to the condyles with the TMJ fossa and can compare the dental arches with the other hard and soft tissues surrounding it.7
ENDODONTICS
CBCT has proved to be a plausible diagnostic tool in modern endodontic practice because of the three-dimensional information it provides. According to a study by Cheng et al, the evaluation of root canal obturation length by CBCT in comparison with periapical radiography showed that CBCT is the best method for the initial identification of maxillary first molar internal morphology.8 It can be used to observe the sagittal, coronal, and axial planes to determine if the root canal obturation is overextended or underextended. CBCT can be used to locate the apical foramen and therefore diagnose obturation lengths. This is a major advantage of CBCT when compared to periapical radiography.8
SURGICAL ASSESSMENT OF PATHOLOGIES
The assessment of complicated third molar impactions necessitates a three-dimensional view in order to interpret the adjoining structures involved. Sumomalainen et al found that CBCT is more effective than two-dimensional radiography in assessing the complicated root morphology, root structure variations, and their corresponding structures before surgical extraction of impacted teeth.9,10 CBCT has better sensitivity values, specificity values, and a greater prediction value. The three-dimensional reconstruction of the bony structures illustrates tumor invasion into the surrounding structures and helps to localize the tumors with exact boundaries—assisting in the surgical assessment of the pathology.11
DENTAL IMPLANTS
Three-dimensional imaging techniques have improved the accuracy of diagnosis and treatment planning for optimal implant placement. The CBCT scan improves visualization of the anatomy and the relationships of implants with adjacent structures. CBCT provides a detailed view of implant sites, allowing the dental practitioner to consider all relative parameters, including facio-lingual/mesio-distal widths, grafted bone, density of bone, and concavity of bone.12
CARIES DIAGNOSIS
When it relates to caries assessment, CBCT is best used to determine the depth of caries of interproximal and occlusal lesions. There is a chance for false positives due to an increase in sensitivity and decrease in specificity with the CBCT unit. CBCT cannot be used on restored teeth that contain metal or radiopaque material. When using CBCT for caries diagnosis, a bitewing radiograph is also needed for precise diagnosis.13 Although caries can sometimes be interpreted using a CBCT image, intraoral radiographs are still the ideal choice for caries diagnosis.
PERIODONTICS
Although many of the same items can be interpreted on both routine two-dimensional and CBCT images, CBCT provides increased detail. CBCT is superior in providing details of buccal and lingual defect measurements.14 It offers a better visual appearance of intrabony defects, as well as dehiscence and fenestration defects, periodontal cysts, and furcation-involved molars.15
TRENDS
The use of CBCT technology is increasing in both the private practice setting, as well as in dental schools, due to its enhanced diagnostic capabilities and the decreasing cost of CBCT machines. In the US, 50 dental schools (89%) have a CBCT machine.16 Overall, approximately 3,000 CBCT units have been sold in the US so far.17 The cost of CBCT machines range in price from $90,000 to more than $300,000.17 The average cost of a CBCT exposure is around $350 in a private practice setting.
When compared to the usual two-dimensional images, such as panoramic radiographs and full-mouth series, CBCT produces a greater radiation exposure, so its use must be justified.2 As with routine dental radiographs, CBCT images should only be taken when needed and not overprescribed.
Adequate training of dental personnel is also key.16 A patient’s dental and health history should be evaluated thoroughly in conjunction with a clinical exam. Once this evaluation has been completed, both radiographs and CBCT imaging can be completed based on patient need. CBCT should only be used for specific cases where three-dimensional imaging is superior to conventional radiography, such as demonstrating the location and extent of pathology, the quantity and quality of bone, and the spatial relationship of an object relative to the adjacent critical anatomical structures.2 Clinicians should review the American Dental Association’s parameters for incorporating CBCT into daily practice.18
CONCLUSION
Although CBCT imaging provides a different perspective of the oral cavity, it is not needed for all patients. As when any radiographic exposure is being considered, the principle of ALARA (as low as reasonably achievable) should be followed at all times. Determining when to use this technology should be decided after reviewing the patient’s medical and dental history in conjunction with a thorough clinical exam. If after routine radiographs are taken, a different vantage point is needed for diagnosis or treatment, a CBCT image can provide enhanced viewing capabilities under certain parameters. Due to additional radiation exposure to the patient, the use of CBCT should be limited. All dental personnel using CBCT should receive proper training to ensure the safety of both clinicians and patients.
REFERENCES
- Hatcher, DC. Operational principles for cone beam computed tomography. J Am Dent Assoc. 2010;141:3S–6S.
- Adibi S, Zhang W, Servos T, O’Neill PN. Cone beam computed tomography in dentistry: what dental educators and learners should know. J Dent Educ. 2012;76:1437–1441.
- Sukovic, P. Cone Beam Computed Tomography in Dentomaxillofacial Imaging. Available at: www.aadmrt.com/currents/sukovic_winter_04_print.htm. Accessed May 20, 2013.
- Scarfe WC, Farman AG. Cone beam computed tomography: a paradigm shift for clinical dentistry. Australasian Dental Practice. 2007:102–110.
- Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008;52:707–730.
- Katsumata A, Hirukawa A, Noujeim M, et al. Image artifact in dental cone-beam CT. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.2006;101:652–657.
- Mah JK, Huang JC, Choo H. Practical applications of cone-beam computed tomography in orthodontics. J Am Dent Assoc. 2010;141:7S–13S.
- Cheng L, Zhang R, Yu X, et al. A comparativeanalysis of periapical radiography and cone beam computerized tomography for the evaluation of endodontic obturation length.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:383–389.
- Suomalainen A, Ventä I, Mattila M, Turtola L,Vehmas T, Peltola JS. Reliability of CBCT and other radiographic methods in preoperative evaluation of lower third molars. Oral SurgOral Med Oral Pathol Oral Radiol Endod. 2010;109:276–284.
- Pohlenz P, Blessmann M, Blake F, HeinrichS, Schmelzle R, Heiland M. Clinical indications and perspectives for intraoperative cone-beam computed tomography in oral andmaxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:412–417.
- Dreiseidler T, Alarabi N, Ritter L, et al. Acomparison of multislice computerized tomography, cone-beam computerized tomography, and single photon emission computerized tomography for the assessment of bone invasion by oral malignancies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:367–374.
- Worthington P, Rubenstein J, Hatcher DC.The role of cone-beam computed tomographyin the planning and placement of implants. J Am Dent Assoc. 2010;141:19S–24S.
- Tyndall DA, Rathore S. Cone-beam CT diagnostic applications: caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am. 2008;52:825–841.
- Mol A. Imaging methods in periodontology. Periodontol 2000. 2004;34:34–48.
- Kasaj A, Willershausen B. Digital volume tomography for diagnostics in periodontology.Int J Comput Dent. 2007;10:155–168.
- Scarfe WC, Levin MD, Gane D, Farman AG.Use of cone beam computed tomography in endodontics. Int J Dent. 2009;2009:634567.
- Parashar V, Whaites E, Monsour P,Chaudhry J, Geist JR. Cone beam computed tomography in dental education: a survey of US, UK, and Australian dental schools. J Dent Educ. 2012;76:1443–1447.
- The American Dental Association Council on Scientific Affairs. The use of cone-beam computed tomography in dentistry: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012;143:899–902.
From Dimensions of Dental Hygiene. June 2013; 11(6): 48–51.



