 IGOR BASTRAKOV / ISTOCK / GETTY IMAGES PLUS
IGOR BASTRAKOV / ISTOCK / GETTY IMAGES PLUS
The Keys to Caries Management
Plans to prevent and/or manage this common oral disease may include a variety of professionally applied or at-home products.
Dental caries, a multifactorial disease involving oral biofilm dysbiosis and several bacterial species,1 is the most prevalent chronic disease for all ages. Despite being preventable, 92% of adults ages 20 to 64 have had caries in their permanent dentition.2 Additionally, the prevalence of untreated caries is approximately 13% for those ages 5 to 19, 25% for ages 20 to 64, and 20% for those age 65 and older.3 Protective factors, risk factors, and disease indicators should be assessed for all patients to determine caries risk level. Furthermore, individualized evidence-based recommendations should be provided for caries prevention and intervention based on caries risk level; one preventive or therapeutic intervention is not effective for all patients.
Protective Factors, Risks Factors, and Disease Indicators
Caries can develop or be prevented based on the balance or imbalance of protective factors and pathological factors in the oral cavity.4,5 Factors that influence caries development are dietary practices associated with frequent fermentable carbohydrate consumption, along with socioeconomic status; special medical, developmental and or physical needs; orthodontics; chemotherapy; and medications that reduce saliva.6–11
Protective factors include adequate saliva, fluoride exposure, and use of antibacterial agents, such as chlorhexidine and xylitol. Pathological factors include presence of cariogenic acidogenic bacteria such as Streptococcus mutans and Lactobacillus; frequently consuming foods with fermentable carbohydrates; and hyposalivation or xerostomia.4,5
If the pathological factors predominate protective factors, demineralization causes a noncavitated lesion to develop. If the process is not stopped or reversed with protective factors, noncavitated lesions progress to cavitated lesions. The aim of caries management is for protective factors to outweigh pathological factors to reverse noncavitated lesions and prevent caries.4
The presence of adequate saliva is key to caries prevention and this should be included in the patient assessment. Table 1 includes questions for salivary hypofunction determination.11 “Yes” answers to all the questions in Table 1 indicate inadequate saliva.12
In addition to asking the patient questions to determine salivary hypofunction, dental hygienists can also assess salivary flow with a 5-minute objective diagnostic test. To assess unstimulated whole saliva, the patient should lean his or her head forward with the mouth open and allow saliva to collect in a sterile container. The patient should not swallow during the collection process. At the end of 5 minutes, the patient should spit any remaining saliva into the container.
Stimulated whole saliva is collected similarly; however, the patient chews on wax or gum during the collection process. Salivary hypofunction is whole unstimulated saliva of less than 0.1 millimeter per minute and/or whole stimulated saliva of less than or equal to 0.7 milliliter per minute.12
In addition to protective and pathological factors, disease indicators should be considered. Caries indicators include the presence or history of caries observed during the clinical exam. Some examples of disease indicators are cavitated lesions, approximal (surfaces which form points of contact between teeth) caries in the enamel only, white spot lesions on smooth surfaces, and any restoration placed within the past 3 years for new patients or placed in the past year for patients of record. Disease indicators are compelling indicators of future disease, but they are not risk factors themselves.4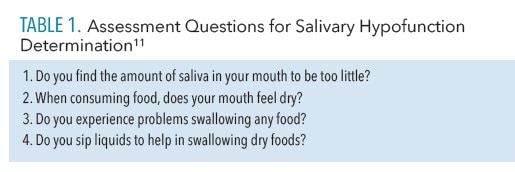
Caries Risk Assessment Tools
Caries risk assessment (CRA) tools can be used to predict future risk for developing caries. CRA tools consider caries risk factors, protective factors, and disease indicators.
A variety of validated CRA tools are available.1 For example, the American Dental Association (ADA) has two caries risk assessment forms available: one for patients ages 0 to 6 and one for patients older than 6.13
The California Dental Association’s caries management by risk assessment (CAMBRA) has tools for patients ages 0 to 5 years and ages 6 and older.14 The American Academy of Pediatric Dentistry has also developed an oral health risk assessment tool for infants, children, and adolescents.15 Caries risk can be categorized as low, moderate, high, and sometimes extreme depending on which CRA tool is used.
Professionally Applied Nonrestorative Caries Management Tools
After a patient’s caries risk level is determined, individualized evidence-based recommendations should be provided. Fluoride is beneficial when applied in the right concentrations and at the appropriate time.
A panel of experts formed by the ADA Council on Scientific Affairs and ADA Center for Evidence-Based Dentistry provided clinical recommendations on professionally applied fluoride and prescription topical fluoride for home use.
For patients ages 6 and older at elevated risk for caries, the expert panel recommended 2.26% fluoride varnish, which contains 22,600 ppm fluoride, or 1.23% acidulated phosphate fluoride (APF) which contains 12,300 ppm fluoride.16
The only professionally applied fluoride recommended by the expert panel for patients younger than 6 is 2.26% fluoride varnish applied at least every 3 months to 6 months.16
The same experts published a systematic review on nonrestorative treatments for caries that included evidence-based practice guidelines. These include the recommendation of 38% silver diamine fluoride (SDF) to be used biannually to arrest advanced caries lesions on the coronal surfaces of primary and permanent teeth with an application of once per week for 3 weeks.17
SDF 38% is a mix of silver, fluoride, and ammonia that has been approved by the United States Food and Drug Administration to treat tooth hypersensitivity; however, it is used off-label to treat caries.18 SDF may be useful for uncooperative patients, where there are barriers to care, or when anesthesia is contraindicated.17 While SDF can be used to arrest caries, some lesions will still require restorative treatment.
The panel also provided recommendations for noncavitated caries. For noncavitated (also called incipient or initial) caries lesions on occlusal surfaces of primary and permanent teeth, sealants are recommended in addition to 5% fluoride varnish or sealants alone vs fluoride varnish only.17
For noncavitated lesions on the facial or lingual surfaces of primary or permanent teeth, 1.23% APF gel or 5% fluoride varnish applied every 3 months to 6 months is recommended.
For approximal noncavitated lesions, 5% fluoride varnish, resin infiltration alone, a combination of 5% fluoride varnish and resin infiltration, and/or sealants are recommended.17
Resin infiltration is a minimally invasive technique in which an etching agent, drying agent, and resin infiltrant are applied and then light cured.19
The expert panel does not recommend 10% casein phosphopeptide-amorphous calcium phosphate paste for noncavitated coronal caries if sealants, fluoride, or resin infiltration are options.17
At-Home Caries Management
All patients, regardless of caries risk, should maintain good oral hygiene and a healthy diet. Dental hygienists are charged with educating their patients on biofilm removal techniques.
Equally important is the evaluation of dietary factors that impact the oral pH. Monosaccharides, especially fructose and disaccharides such as sucrose or table sugar added to many foods and drinks, are major culprits in the caries process.20
Patients should be advised to reduce the intake of fermentable carbohydrate-rich foods and drinks in addition to decreasing consumption of those with naturally occurring sugars, such as honey and fruit juices.
As carbohydrates quickly removed from the mouth by saliva are less likely to cause demineralization than those slowly removed, both the consistency and method of consumption are important to evaluate. Sipping on sugary drinks throughout the day or consuming sticky, sugary foods lower the oral pH for longer periods, increasing the risk for demineralization.21
 To assess diet, clinicians may ask patients what they ate in the past 24 hours, what they normally eat in a day, or ask patients to document what they eat for several days. Patients who consume a high and/or frequent intake of carbohydrates, such as starches and added sugars, are at high caries risk and therefore may benefit from dietary counseling.22
To assess diet, clinicians may ask patients what they ate in the past 24 hours, what they normally eat in a day, or ask patients to document what they eat for several days. Patients who consume a high and/or frequent intake of carbohydrates, such as starches and added sugars, are at high caries risk and therefore may benefit from dietary counseling.22
Dietary counseling involves educating the patient on the correlation between cariogenic foods and oral health as well as the relationship between frequency of consumption and caries risk.
Helping the patient come up with a healthy food plan is also important. MyPlate Plan is a free, online resource that provides customized food group and calorie recommendations based on an individual’s height, weight, age, sex, and daily physical activity.23
Dental hygienists can print the MyPlate Plan for the patient to take home after the appointment is over.
Patients at low caries risk should be advised to use over-the counter fluoride toothpaste and drink fluoridated water. Sodium fluoride, sodium monofluorophosphate, and stannous fluoride are used in anticaries toothpastes in the US.
All toothpastes with the ADA Seal of Acceptance must have fluoride.24 Fluoride toothpastes in the United States typically contain 1,000 ppm to 1,500 ppm fluoride.25 To help prevent fluorosis, children younger than age 3 should use an amount of toothpaste the size of a grain of rice and a pea-sized amount if between the ages of 3 and 6.24 Children younger than age 6 should not use fluoride mouthrinse due to the risk of fluorosis if ingested.
For patients at elevated caries risk, prescription products are available. Prescription strength, home-use fluoride includes 0.09% fluoride mouthrinse or 0.5% fluoride gel or paste.16 For cavitated or noncavitated root caries in permanent teeth, the use of 5,000 ppm toothpaste or gel such as one with 1.1% sodium fluoride, which is available by prescription only, is recommended.17
Some research suggests patients at high caries risk need antibacterial agents in addition to fluoride to reduce cariogenic bacteria and prevent future caries.5,26 Chlorhexidine gluconate, xylitol, and stannous fluoride are antibacterial agents that may aid in caries management.
Chlorhexidine gluconate (0.12%) is available as prescription mouthrinse that may be recommended to patients at high or extremely high caries risk. Patients should rinse for 1 minute daily for 1 week per month to target S. mutans and Lactobacillus.4 Fluoride supplemented with chlorhexidine significantly reduces the bacteria load.26,27
Xylitol is a natural sugar alcohol that is nonfermentable by cariogenic bacteria. Available as chewing gum, lozenges, candies, and mints, xylitol aids in caries management by reducing S. mutans, hindering bacteria from adhering to tooth structure, and inhibiting the transfer of bacteria from caregivers to children.4
Consuming enough xylitol is a factor in its efficacy. A 2017 systematic review by Marghalani et al28 found children who used more than 4 grams of xylitol daily had a caries reduction of 54%, compared to a 17% caries reduction when 3 grams of xylitol was used daily.
Conclusion
Dental hygienists are prevention specialists and play an integral role in caries management. Due to the multifactorial nature of caries, dental hygienists should perform a caries risk assessment and determine risk level. Then evidence-based guidelines can be tailored to each patient based on his or her individual risk assessment.
To support evidence-based decision making, clinicians should also consider their clinical expertise and patient preferences in their oral hygiene and dietary recommendations.
Caries management recommendations may include a variety of professionally applied products such as sealants, fluoride varnish, SDF or APF, or at-home products such as fluoride toothpaste, fluoride rinse, chlorhexidine gluconate rinse, or xylitol. Overall, the ultimate goal of caries management and prevention is to prevent future caries and reverse or stop noncavitated lesions, promoting optimal oral health throughout patients’ lifetimes.
References
- Featherstone, JDB, Crystal YO, Alston P et al. A comparison of four caries risk assessment methods. Front Oral Health. 2021;2:656558.
- National Institute of Dental and Craniofacial Research. Dental Caries (Tooth Decay). Available at: nidcr.nih.g/v/research/data-statistics/dental-caries. Accessed January 21, 2023.
- United States Centers for Disease Control and Prevention. Oral and Dental Health. Available at: cdc.gov/nchs/fastats/dental.htm. Accessed January 21, 2023.
- Rechmann P, Kinsel R, Featherstone JDB. Integrating caries management by risk assessment (CAMBRA) and prevention strategies into the contemporary dental practice. Compend Contin Educ Dent. 2018;39:226–233.
- Featherstone JDB, Chaffee BW. The evidence for caries management by risk assessment (CAMBRA®). Adv Dent Res. 2018;29:9–14.
- Naveed N, Kishorekumar S. Influence of socioeconomic and working status of the parents on the incidence of their children’s dental caries. Indian Journal of Forensic Medicine and Toxicology. 2020;14(4):1455–1458.
- Frank M, Keels MA, Quinonez R, Roberts M, Divaris K. Dental caries risk varies among subgroups of children with special health care needs. Pediatr Dent. 2019;41:378–384.
- Karabekiroglu S, Ileri Z, Kahraman FB, Unlu N. The effects of fixed orthodontic treatment period on white spot lesion prevalence and dmft indexJ J Istanb Univ Fac Dent. 2014;48:27–35.
- Wang Y, Zeng X, Yang X, et al. Oral health, caries risk profiles, and oral microbiome of pediatric patients with leukemia submitted to chemotherapy. Biomed Res Int. 2021;2021:6637503.
- Olczak-Kowalczyk D, Krasuska-Sławińska E, Brożyna A, Turska-Szybka A, Dembowska-Bagiñska B, Dembowska-Bagińska B. Dental caries in children and adolescents during and after antineoplastic chemotherapy. J Clin Pediatr Dent. 2018;42:225–230.
- Jurasic MM, Gibson G, Wehler CJ, Orner MB, Jones JA, . Caries prevalence and associations with medications and medical comorbidities. J Public Health Dent. 2019;79:34–43.
- Navazesh M, Kumar SKS. Measuring salivary flow: challenges and opportunities. J Am Dent Assoc. 2008;139:35S–40S
- American Dental Association. Oral Health Topics: Caries Risk Assessment and Management. Available at: ada.org/en/member-center/oral-health-topics/caries-risk-assessment-and-management. Accessed January 21, 2023.
- Young DA, Featherstone JD, Roth JR, et al. Caries management by risk assessment: implementation guidelines. J Calif Dent Assoc. 2007;35:799–805.
- American Academy of Pediatric Dentistry. Caries-Risk Assessment and Management for Infants, Children, and Adolescents. Available at: aapd.org/media/Polici_s_Guidelines/BP_CariesRiskAssessment.pdf. Accessed January 21, 2023.
- Weyant RJ, Tracy SL, Anselmo T, et al. Topical fluoride for caries prevention. J Am Dent Assoc. 2013;144:1279–1291.
- Slayton RL, Urquhart O, Araujo MWB, et al. Evidence-based clinical practice guideline on nonrestorative treatments for carious lesions: a report from the American Dental Association. J Am Dent Assoc. 2018;149:837–849.
- American Dental Association. Oral Health Topics: Silver Diamine Fluoride. Available at: ada.org/en/member-center/oral-health-topics/silver-diamine-fluoride. Accessed January 21, 2023.
- Manoharan V, Arun Kumar S, Arumugam SB, Anand V, Krishnamoorthy S, Methippara JJ. Is resin infiltration a microinvasive approach to white lesions of calcified tooth structures?: a systemic review. Int J Clin Pediatr Dent. 2019;12:53–58.
- Sheiham A, James WP. A new understanding of the relationship between sugars, dental caries and fluoride use: implications for limits on sugars consumption. Public Health Nutr. 2014;17:2176––2184.
- Díaz-Garrido N, Lozano C, Giacaman RA. Frequency of sucrose exposure on the cariogenicity of a biofilm-caries model. Eur J Dent. 2016;10:345–350.
- Marshall T. Impact of diet and nutrition on oral health. Dimensions of Dental Hygiene. 2016;14(4):48–51.
- United States Department of Agriculture. MyPlate Plan. Available at: myplate.gov/myplate-plan. Accessed January 23, 2023.
- American Dental Association. Oral Health Topics: Toothpastes. Available at: ada.org/en/member-center/oral-health-topics/toothpastes. Accessed January 23, 2023.
- United States Centers for Disease Control and Prevention. Other Fluoride Products. Available at: cdc.gov/fluoridation/basics/fluoride-products.html. Accessed January 23, 2023.
- Featherstone JD, White JM, Hoover, CL, et al. A randomized clinical trial of anticaries therapies targeted according to risk management (caries management by risk assessment). Caries Res. 2012;46:118–129.
- Chaffee BW, Cheng J, Featherstone JDB. Non-operative anti-caries agents and dental caries increment among adults at high caries risk: a retrospective cohort study. BMC Oral Health. 2015;15:111.
- Marghalani AA, Guinto E, Phan M, Dhar V, Tinanoff N. Effectiveness of xylitol in reducing dental caries in children. Pediatr Dent. 2017;39:103–110.
From Dimensions of Dental Hygiene. February 2023; 21(2)18,21-23.

