 SCIEPRO / ISTOCK / GETTY IMAGES PLUS
SCIEPRO / ISTOCK / GETTY IMAGES PLUS
Improve the Ergonomics of Your Instrumentation
Incorporating small operator adjustments may help reduce the risk of musculoskeletal injuries and prolong your career in dental hygiene.
Dental hygienists must maintain prolonged static postures, often in awkward positions, and make repetitive small motor movements of the fingers and hands. The combination of these biomechanical risk factors can contribute to the onset of musculoskeletal disorders (MSDs).
Work-related MSDs among dental hygienists are strongly associated with prolonged static postures, the forceful continual repetition small motor movements, and non-neutral clinician posture necessary during therapeutic dental procedures.1
MSDs are a significant health concern for dental hygienists worldwide.2 The repetitive and precise movements of the hands, wrists and fingers, as well as prolonged static postures, place dental hygienists at a higher risk of developing MSDs than other occupations.2–4
The development of such MSDs causes absenteeism from work and/or early retirement from the profession.5 Multifactorial in nature, MSDs come in a variety of forms. The primary types affecting dental hygienists are pain in the neck, back, shoulder, wrist, and hand regions.2
Seating Positions
Textbooks have typically advised dental hygienists to complete periodontal instrumentation while seated next to the patient from the traditional “front” position.6 These seating types are often referred to as the “clock” positions.
For a right-handed clinician, the clock positions are typically between 12:00, where the clinician is seated directly behind the patient’s head, to 7:00, or the side position, where the clinician is facing the patient.
For left-handed clinicians the clock positions range from 12:00 to 4:00 (side position).7–10 In the 1950s, Daryl Beach, DMD, introduced the concept of “proprioceptive deviation.”11 In this context, proprioception means “having a sense or perception of the movements and position of one’s body and limbs, independent of vision, thus allowing the dental hygienist to use proprioceptive self-awareness to determine the most efficient, stress-free process of performing dental procedures.”11
In this type of operator positioning, dental hygienists establish their most comfortable and balanced working posture, then integrate their clinical procedures while maintaining the original posture. Once comfortably seated, the patient is positioned to support the dental hygienist’s posture and positioning; fine adjustments are made throughout the procedure to allow the clinician to maintain this position, decreasing undo stress on the musculoskeletal system.8 In addition, the clinician’s instruments are placed where neutral positions can be maintained when reaching for necessary equipment.11
Clinicians can work through their own postural needs while preventing or eliminating MSD risk factors through a combination of both the traditional clock positions and proprioceptive deviations. Small, fine adjustments to clinician and patient positioning, in addition to adjusting the hands and fulcrum, can help dental hygienists achieve and maintain neutral working positions.

Neutral Working Posture
A neutral working posture includes keeping the head upright, the shoulders relaxed, elbows flexed to 90º, forearm in a mid-position (thumbs up), wrists straight, back straight (maintaining the natural curves), knees bent at 90º, and feet flat on the floor (Table 1).11,12
Neck. Maintaining a neutral neck position while scaling can be difficult, as many areas of the mouth are hidden in shadows, exist outside of the direct line of sight, or are covered by soft tissues (tongue and buccal mucosa).
Neck flexion of 30° or more (Figure 1) creates a too-heavy load on the cervical muscles. Significant muscular fatigue will be felt within 4 hours to 5 hours of work in this position. This “head-forward/shoulder-protracted” posture can lead to the shortening of the pectoralis, serratus anterior, scalene, and sternocleidomastoid muscles over time, whereas the middle and lower trapezius muscles may become lengthened.
The imbalance of stabilizing muscles groups vs movement muscle groups leads to an overall decrease in how well the muscles contract while working, leading to muscular ischemia and pain in the overworked muscles. This imbalance also puts the cervical discs at risk of injury.13,14
To correct this, clinicians need to make sure they maintain a head tilt of only 0° to 20°, ensuring the line from the eyes to the treatment area is as near vertical as possible. To accomplish this, clinicians should adapt the chair and the patient while working each arch.
For the maxillary arch, the back of the patient chair should be nearly parallel to the floor. Patients’ feet should be even or slightly higher than the tip of their nose and they should be in a chin-up position with their head even with the upper edge of the head rest.
Additionally, clinicians should direct patients to turn their head to the right or left when changing from working on direct vision to indirect vision locations as well as raise or tilt their chin to prevent bending of the neck and twisting of the torso.
Back. Back problems—both chronic and acute—have been reported in about 60% to 70% of dental hygienists.3 Upper back pain is less common among dental hygienists (37%) whereas low back pain occurs more frequently (52.1%). Both are the result of awkward and static posture and non-neutral positioning.1
This is especially true while using seated-posture dentistry. The repeated leaning toward a patient can cause overexertion and strain on the lower back extensor muscles, weakening the abdominal stability muscles.13,14 The thoracic spine should extend no more than 20° forward and maintain a –10° to 10° lateral flexion.15
Flexion and extension greater than 60° and lateral flexion at -20° to 20° will create unnecessary stress and strain on the muscles of the back and increase intrinsic disc pressure, causing an imbalance of muscle contractions.15 Figure 2 shows improper neck position.
Correct patient positioning. Dental hygienists must make sure the patient is seated at the correct height for the arch in which they are working in order to maintain a neutral spine on both flexion and extension forward, as well as a neutral shoulder and elbow position. This allows for relaxation of a variety of the upper back muscles.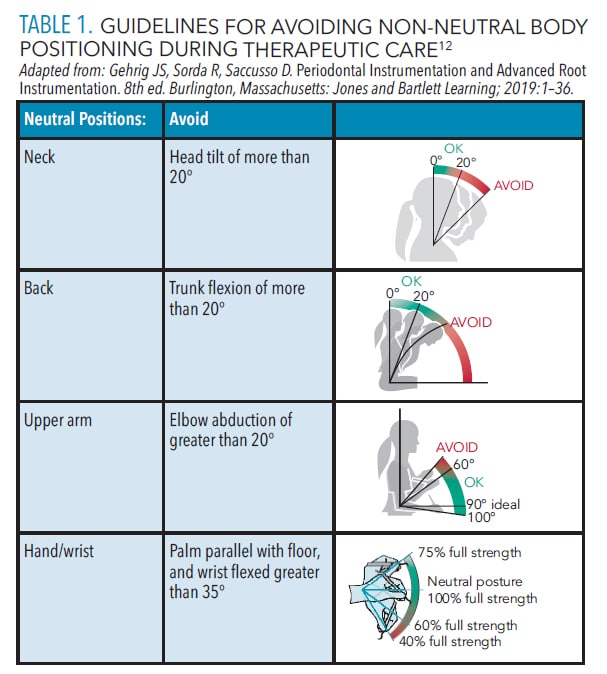
During routine dental hygiene clinical care, most of the work is done with the arms out in front of the body. This anterior arm positioning instantaneously increases the muscle activity of the shoulders and the neck (erector spinae cervicalis, upper trapezius, erector spinae thoracalis, levator scapulae, and sternocleidomastoid).
When working in a situation where the arms are too high or too abducted away from the body, upper thoracic and neck extensors occur (Figure 3A). This leads to increased fatigue and pain of the neck and shoulder muscles and, eventually, trapezius myalgia.13,14,16
Adjusting the patient chair height so that the tip of the patient’s nose is below the clinician’s waist, or the patient’s open mouth below the clinician’s elbow will help lower the arms and relax the upper back muscles (Figure 3B).9
Adjustments to clinician positioning. Primarily working from the 11:00 and side (front) positions while making slight adjustments to the seating positions can help create a neutral spine reducing the over flexion and extension of the upper and lower back muscles. For example, when instrumenting the mandibular right posterior away (lingual) surfaces (right-handed clinician), the clinician should sit between 10 o’clock to 11 o’clock. Often dental hygienists will find their optimal spot when beginning on the most posterior surfaces and remaining static as they move more anteriorly.
Allowing small chair adjustments from 11:00 toward 10:00 as they move from the most posterior (distal) surfaces to the more anterior (mesial) surfaces and encouraging patients to turn their head toward the clinician in a chin-down position will allow the dental hygienist to maintain a less static position and reduce the overflexion and extension of the back muscles. Similar adjustments with both the clinician and the patient should be made with all sextants and surfaces of the mouth to reduce the risk for MSDs.
Standing vs sitting. An intrinsic pressure of about 0.7kg/cm2 exists within the intervertebral disk of a resting spine.17 The resting pressure rises when the disc is subjected to an increased load, such as varying body positions due to the force from muscle contraction.

Seated and bending postures apply more muscular and disc loads than standing positions.17–19 While performing dental work, different muscles are used while standing vs sitting. Sitting puts much more pressure on the muscles of the back, shoulders, and neck.18
When seated on a flat surface, the spine’s degree of flexion is increased as is the intrinsic pressure. In fact, the act of leaning forward by even 20°, increases intrinsic pressure by 40 kg to 60 kg.20
If working while seated is necessary, tilt the clinician chair forward 5° to 15° to maintain the natural lower back curve. This will place the hips slightly higher than the knees and increase the hip angle to greater than 90,° which will allow the clinician to be closer to the patient during treatment.13,14 Additionally, alternating from a seated to standing position during clinical care will allow the muscles used to stabilize sitting to rest while engaging the muscles that stabilize standing.
Wrists/hands. About 25% of working dental hygienists report pain in the wrists;1 6.4% to 11% of all dental hygienist are diagnosed with carpal tunnel syndrome.21,22 In proper technique, the fingers will remain firm on the dental instrument while the forearm and the wrist provide the main source of power and direction for each therapeutic stroke. For optional wrist movement, the wrist should move from 5° of flexion to about 35° of extension where the forearm will rotate from supination to pronation.23
In order to maintain the proper neutral forearm and wrist positioning, the clinician should consider using the palm-up approach on the maxilla and a palm-down approach when working on the mandible. Both of these, however, can lead to a non-neutral wrist/forearm position if the clinician’s or the patient’s positioning is incorrect.

The use of proprioceptive deviation can help clinicians become more aware of improper body positions that can lead to MSDs. For example, when working in the maxillary right posterior buccal surfaces while seated in the front (side) position, the palm should be positioned so that it is close to the occlusal surfaces of the teeth. This helps the clinician to maintain a neutral wrist and reduce the risk of injury.
While instrumenting the upper right posterior buccal surfaces, the operator should sit at 10 o’clock to 11 o’clock and make small adjustments, such as having the patient turn slightly away or lowering the patient chair so that the patient’s nose is level with the operator’s elbow. This adjustment will straighten out the wrist allowing for optimal force on the fulcrum.
Additionally, while working in the mandibular posterior lingual surfaces, a small adjustment can be made to the patient, chair, and operator positioning to promote a neutral wrist. For this to occur, the clinician will need to adjust the clock positions from the 11 o’clock on the distal to 10:00 while on the mesial.
Conclusion
Applying thoughtful ergonomics into practice can help the dental hygienist in several ways. It can significantly reduce the chance of developing MSDs, decrease work time lost to injury, and increase career longevity. Using proprioceptive deviations during the workday as well as alternating sitting vs standing working positions may reduce overall stress on the spine and body.
References
- Gandolfi MG, Zamparini F, Spinelli A, Risi A, Prati C. Musculoskeletal disorders among Italian dentists and dental hygienists. Int J Environ Res Public Health. 2021;18:2705.
- Hayes MJ, Smith DR, Cockrell D. An international review of musculoskeletal disorders in the dental hygiene profession. Int Dent J. 2010;60:343–352.
- Lalumandier JA, McPhee SD, Parrott CB, Vendemia M. Musculoskeletal pain: prevalence, prevention, and differences among dental office personnel. Gen Dent. 2001;49:160–166.
- Crawford L, Gutierrez G, Harber P. Work environment and occupational health of dental hygienists: a qualitative assessment. J Occup Environ Med. 2005;47:623–632.
- Gupta A, Bhat M, Mohammed T, Bansal N, Gupta G. Int J Clin Pediatr Dent. 2014;7:30–34.
- Cooper MD, Wiechmann L. Essentials of Dental Hygiene Preclinical Skills. Upper Saddle River, New Jersey: Pearson/Prentice Hall; 2005:321.
- Boyd LD, Mallonee LF, Wyche CJ, Halaris JF. Wilkins’ Clinical Practice of the Dental Hygienist. Burlington, Massachusetts: Jones & Bartlett Learning; 2020.
- Barry RM, Spolarich AE, Weber M, Krause D, Woodall WD, Bailey JH. Impact of operator positioning on musculoskeletal disorders and work habits among Mississippi dental hygienists. J Dent Hyg. 2017;91:6–14.
- Nield JS. Fundamentals of Periodontal Instrumentation and Advanced Root Instrumentation. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2004.
- Gehrig J, Sroda R, Saccuzzo D. Fundamentals of Periodontal Instrumentation and Advanced Root Instrumentation. Philadelphia: Lippincott Williams & Wilkins; 2018.
- Chaikumarn M. Working conditions and dentists’ attitude towards proprioceptive derivation. Int J Occup Saf Ergon. 2004;10:137–146.
- Sanders MJ, Turcotte CA. Ergonomic strategies for dental professionals. Work. 1997;8:55–72.
- Valachi B, Valachi K. Preventing musculoskeletal disorders in clinical dentistry: strategies to address the mechanisms leading to musculoskeletal disorders. J Am Dent Assoc. 2003;134:1604–1612.
- Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc. 2003;134:1344–1350.
- Ohlendorf D, Erbe C, Hauck I, et al. Restricted posture in dentistry—a kinematic analysis of orthodontists. BMC Musculoskelet Disord. 2017;18:275.
- Schüldt K, Ekholm J, Harms-Ringdahl K, Németh G, Arborelius UP. Effects of changes in sitting work posture on static neck and shoulder muscle activity. Ergonomics. 1986;29:1525–1537.
- Nachemson A. The load on lumbar disks in different positions of the body. Clin Orthop Relat Res. 1966;45:107–122.
- Nachemson AL, Morris JM. In vivo measurements of intradiscal pressure: discometry, a method for the determination of pressure in the lower lumbar discs. JBJS. 1964;46(5):1077–1092.
- Pejčić N, Đurić-Jovičić M, Miljković N, Popović DB, Petrović V. Posture in dentists: Sitting vs. standing positions during dentistry work: an EMG study. Srpski Arhiv Za Celokupno Lekarstvo. 2016;144:181–187.
- Nachemson AL. The lumbar spine an orthopaedic challenge. Spine. 1976;1:59–71.
- Osborn JB, Newell KJ, Rudney JD, Stoltenberg JL. Carpal tunnel syndrome among Minnesota dental hygienists. J Dent Hyg. 1990;64:79–85.
- Macdonald G, Robertson MM, Erickson JA. Carpal tunnel syndrome among California dental hygienists. Dent Hyg (Chic). 1988;62:322–327.
- Sanders MJ, Michalak-Turcotte C. Preventing work-related MSDs in dental hygienists. In: Ergonomics and the Management of Musculoskeletal Disorders. Oxford, United Kingdom: Butterworth-Heinemann; 2004:448–473.
From Dimensions of Dental Hygiene. February 2023; 21(2)24-27.

