 THANK YOU FOR YOUR ASSISTANT (SIC) / ISTOCK / GETTY IMAGES PLUS
THANK YOU FOR YOUR ASSISTANT (SIC) / ISTOCK / GETTY IMAGES PLUS
The Essential Role of Airflow Filtration, and Ventilation on Air Quality in the Dental Setting
A multidimensional approach is key to creating a safe indoor environment.
The risks posed by dental aerosols have become top-of-mind among oral health professionals with the emergence of SARS-CoV-2 over the past few years. However, dentistry has a long history of incorporating effective infection control measures to create a safe environment for patients and personnel. The low incidence of COVID-19 transmission in dental settings is a testament to an effective combination of educational programing, policies, procedures, and the dedication of oral health professionals incorporating stringent protocols in the dental office.
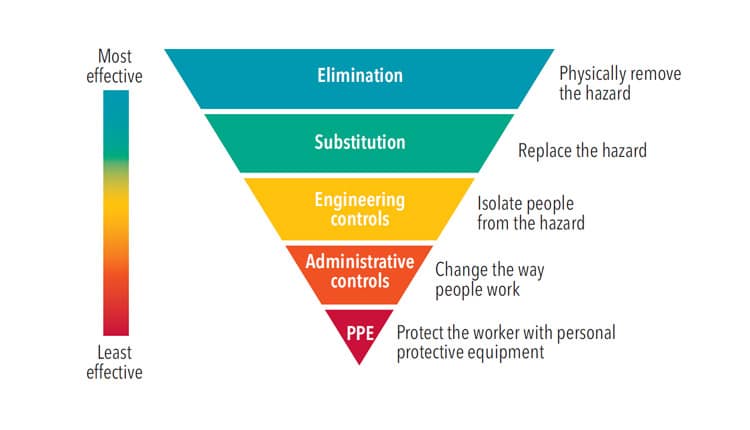
Multiple agencies—such as the United States Centers for Disease Control and Prevention (CDC), Occupational Safety and Health Administration, National Institute for Occupational Safety and Health (NIOSH), and Organization for Safety, Asepsis and Prevention (OSAP)—provide current scientific research and information to assist oral health professionals in promoting a healthy and safe work environment. The COVID-19 pandemic has forced dentistry to reevaluate infection control measures with a focus on the hierarchy of controls that include elimination, substitution, engineering, and administrative controls, as well as personal protective equipment (PPE).1
Hierarchy of Controls
The CDC and NIOSH established a “hierarchy of controls” to identify and mitigate exposure to hazards before a worker is exposed.1 Effective controls strive to eliminate or reduce risks to promote worker safety. The most effective controls are at the top of the list, which descends to those considered the least effective (Figure 1).1
Eliminating hazards is the most effective control but it is not always feasible. Attention to eliminating hazards in the design or early stages of any development makes this more attainable and less expensive.1
Substitution involves replacing a hazard with nonhazardous options. Elimination and substitution have not been an option during the COVID-19 pandemic because the virus and variants continue to circulate across the globe. Theoretically, the virus could be eliminated if a vaccine was effective against all variants and everyone worldwide developed immunity. An example of a substitution is the replacement of radiographic film requiring chemical processing with digital radiography.
Engineering controls do not eliminate hazards but isolate people from a hazard. Examples include installing physical barriers, use of high-volume evacuation (HVE) and rubber dams, instrument cassettes, needle recapping devices, and sharps containers. During the pandemic, the CDC published the following recommendations for dental facilities to prevent the spread of airborne pathogens:2
- Space dental chairs at least 6 feet apart.
- Place easy-to-clean physical barriers between patient chairs.
- Orient operatories parallel with the direction of airflow.
- The patient’s head should be positioned near return air vents, away from corridors, and toward a rear wall when feasible.
High-efficiency heating, ventilation, and air conditioning (HVAC) systems with high-efficiency particulate air (HEPA) filters enhance air quality. Well-designed engineering controls can effectively enhance productivity and worker comfort, as well as safety. Because it is not always possible to remove or reduce all hazards through elimination or substitution, engineering controls and administrative controls serve as the next level in the hierarchy.3
Administrative controls are thought to be less effective than other controls because they require additional effort by workers to adjust the way they work.1 They include preprocedural mouthrinsing, predispensing single-use items, avoiding aerosol-producing procedures, developing written policies and operating procedures, personnel training, immunization tracking, and adhering to a respiratory protection program (RPP).4
A primary example of RPP is fit testing N95 masks or a reusable elastometric half-mask respirator for each dental team member. Clinicians using N95 respirators should be fit tested annually. A fit test measures for any leakage to ensure a tight seal between the respirator and facial structure for each specific manufacturer, model, and size.5 When purchasing N95 masks/respirators, NIOSH certification indicates they have undergone rigorous testing and are a “legitimate particulate respirator.”5,6
Many oral health professionals are not aware that PPE is the last line of defense in the hierarchy of controls.1 PPE is used to protect the clinician when the other controls in the hierarchy cannot eliminate or mitigate hazards. Donning of gowns, masks, N95 respirators, eye protection (goggles, face shields), and gloves should be used appropriately for the specific procedure(s) performed.2
Air Flow and Ventilation Control
The quality of ambient air is not readily observable but is critical in preventing the spread of viruses and diseases. Increasing outside air flow and ventilation are important in minimizing exposure to aerosols and contaminants in a dental facility.
The American Institute of Architects established guidelines to address indoor air-quality standards.7 As new dental facilities are built and older ones renovated, engineering controls are needed to mitigate dental aerosols. A primary control is to regulate outside airflow and reduce aerosols through air filtration devices.7
The amount of time viruses remain airborne varies depending on their particle size, with smaller nano-sized particles staying airborne for up to 40 hours.8 Airborne particles are influenced by air currents created by fans, people walking and movement, humidity, and HVAC units.8 The primary types of air filtration are built-in HVAC systems and free-standing units that provide additional air filtration. The need for free-standing units is based on the efficacy of the HVAC system, room size, and occupancy.9
HVAC systems consist of the building’s central heating and cooling equipment. As air is circulated within the system, it runs through a filter to remove contaminants from the air before recirculating into the building. The HVAC system serves as the principal mover of air within a building.9 Installing a high-efficient filter within the HVAC system may provide a sufficient level of protection to negate the need for free-standing air filtration units. Airflow within buildings is affected by numerous factors including furniture and walls, people moving, and open windows and doors, creating areas of higher and lower pressure.9 Any air filtration system needs to be evaluated for the cubic feet of air the system can process, also referred to as the air exchange rate, and the rating of the specific air filter. Even if the HVAC system is able to provide quality environmental air, the addition of free-standing air purification systems can greatly reduce the time it takes to clear a room of potentially-infectious aerosols.2
In February 2022, the CDC released updated infection control recommendations for healthcare professionals that included using physical barriers and improving ventilation systems.10 Complementing these recommendations, the US Environmental Protection Agency has identified steps to control indoor pollutants.9 Most dental professionals are familiar with the concept of source control and reducing aerosols and the use of HVE systems. The other two recommendations may be less familiar: ventilation and air cleaning.
Two types of air filter ratings are used in HVAC and free-standing filtration systems: minimum efficency reporting value (MERV) and HEPA.10 A MERV rating is based on testing developed by the American Society of Heating, Refrigerating, and Air-Conditioning Engineers. MERVs describe the ability of a filter to collect particles between 10 microns down to 0.3 microns.9,10 In this rating system, a higher MERV rating correlates with improved air filtration. Particles of 0.3 microns are the most penetrating particle size.10
A common misconception is that particles smaller than 0.3 microns, such as the COVID-19 virus at 0.125, are not filtered as effectively. This is not necessarily true for a couple of reasons. First, particles of 0.3 microns are the most challenging to filter while particles both larger and smaller are filtered at much higher rates.10 The ability to trap particles is influenced by how the particles move in the air in addition to their size. Smaller particles bounce around in the air in a zigzag like motion known as Brownian motion.11 Second, for viruses to remain airborne, they must attach to a larger dust particle or water droplet, which can then be trapped in an air filter.
Recommended by the CDC, HEPA filtration is another fairly simple yet effective environmental control.2 HEPA filters consist of a “mat of randomly aligned fibers, made from either glass or synthetic materials.”12 They are efficient and effective at removing 99.97% of most size particles, including viruses and bacteria but not gases such as nitrous or carbon dioxide.12 A HEPA filter’s MERV rating is 17 or higher.13 Both HVAC filtration and free-standing air purifiers reduce the volume of aerosolized pathogens in the air. Initially when turned on, air purifiers create substantial airflow disturbances and movement of nano-sized aggregates. However, continuous use can significantly reduce the overall concentration of respiratory droplets in the air.14 Running air purifiers and ventilation systems during working hours and up to 2 hours at the end of the business day is recommended.15
Carbon Dioxide Monitoring
Carbon dioxide (CO2) can build up in a room through simple respiration. Higher CO2 levels indicate poor ventilation and/or an overcrowded room. High CO2 levels can result in pathogen-laden aerosols that negatively impact health.16 Measuring adequate ventilation in dental operatories can be accomplished with a consumer grade CO2 monitor. Normal atmospheric CO2 levels are approximately 400 parts per million (ppm) whereas exhaled air might be as high as 40,000 ppm.16 A dental operatory with good ventilation should mirror outdoor CO2 levels. A recent study by Zemouri et al17 found …”CO2 levels were found to play the most important role in the risk of disease transmission.” Levels at or above 1,135 ppm potentially increase the risk of pathogen transmission.17 Therefore, monitoring CO2 levels in a dental office can help identify spaces that would benefit from increasing outdoor air flow or incorporating an adjunctive air treatment system.16,17
Inspired by the COVID-19 pandemic, OSAP’s 2020 infection control guidelines recommend proper ventilation and air filtration controls.15 The simplest way to enhance proper ventilation is to change the setting of the HVAC thermostat from “auto” to “on.”18 This step keeps the air circulating through the HVAC filtration system throughout the day.
Upper-Room Ultraviolet Germicidal Irradiation
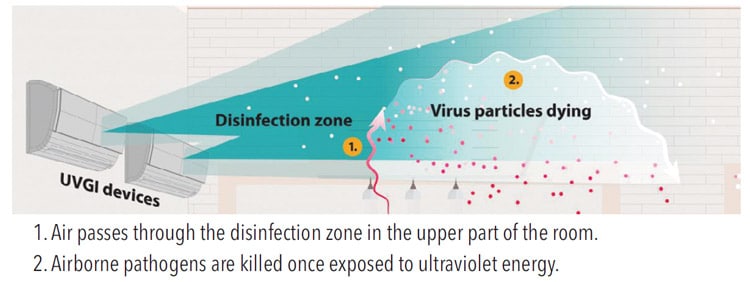
Upper-room ultraviolet germicidal irradiation (UR-UVGI) systems use ultraviolet energy to create a zone that kills airborne pathogens. UR-UVGI systems have a long history of substantial germicidal and tuberculocidal effects. UR-UVGI systems eliminate pathogens as they enter the irradiated area in the upper portion of dental operatories. Ultraviolet-C irradiation has a shorter wavelength that breaks the bonds that hold a microorganism’s DNA and RNA strands together, thus destroying viral and bacterial pathogens, including SARS-CoV-2. Because ultraviolet-C irradiation can be dangerous to humans, the UR-UVGI system is installed within HVAC ducts or along the upper wall or ceiling of a room (Figure 2). This directs the ultraviolet-C energy toward the upper part of a room, ensuring occupants in the room receive ultraviolet doses well below current safe exposure levels and preventing eye and skin damage.19,20
The COVID-19 pandemic has created an environment of innovation for multiple new air treatment options. Ideas such as ionization, dry hydrogen peroxide, and chemical fogging disinfection have emerged to combat the spread of the virus.15 OSAP guidelines recommend that oral health professionals use caution when using these new air treatment options as the evidence related to efficacy and safety is not yet fully understood.15 Consulting a knowledgeable professional is recommended when installing and maintaining these engineering controls.
Conclusion
Creating a safe indoor environment requires a multidimensional approach. While it is not realistic to eliminate all airborne contaminates and hazards in a dental setting, disease transmission can be minimized by incorporating as many aspects of the hierarchy of controls as possible.
References
- The National Institute for Occupational Safety and Health. Hierarchy of Controls. Available at: cdc.g/v/niosh/topics/hierarchy/default.html. Accessed July 20, 2022.
- United States Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic. Available at: cdc.gov/coronavirus/떓-ncov/hcp/infection-control-recommendations.html. Accessed July 20, 2022.
- The National Institute for Occupational Safety and Health. Indoor Environmental Quality. Available at: cdc.gov/niosh/topics/indoorenv/buildingventilation.html. Accessed July 20, 2022.
- Occupational Safety and Health Administration. Respiratory Protection. Available at: osha.gov/respiratory-protection. Accessed Juy 20, 2022
- United States Centers for Disease Control and Prevention. The Respiratory Protection Information Trusted Source. Available at: cdc.gov/niosh/npptl/topics/respirators/di_p_part/respsource3fittest.html Accessed July 20, 2022.
- OSHA Review. OSHA Requirements for Occupational Use of N95 Respirators in Healthcare. Available at: oshareview.com/떔/葐/osha-requirements-for-occupational-use-of-n95-respirators-in-healthcare. Accessed July 20, 2022.
- United States Centers for Disease Control and Prevention. Guidelines for Environmental Infection Control in Health-Care Facilities, 2003. Available at: cdc.gov/infectioncontrol/guidelines/environmental/index.html. Accessed July 20, 2022.
- Kumar PS, Subramanian K. Demystifying the mist: Sources of microbial bioload in dental aerosolsJ J Periodontol. 2020;91:1113–1122.
- United States Environmental Protection Agency. Building Air Quality Guide: a Guide for Building Owners and Facility Managers. Available at: epa.gov/indoor-air-quality-iaq/building-air-quality-guide-guide-building-owners-and-facility-managers. Accessed Juy 22, 2022.
- United States Environmental Protection Agency. What is a MERV rating? Available at: epa.gov/indoor-air-quality-iaq/what-merv-rating-1. Accessed July 20, 2022.
- Gustafsson O, Gustafsson S, Manukyan L, Mihranyan A. Significance of Brownian motion for nanoparticle and virus capture in nanocellulose-based filter paper. Membranes (Basel). 2018;8:90.
- Robertson P. What are HEPA filters and how do they work? Available at: smartairfilters.com/en/blog/what-is-hepa-filter-how-hepa-air-filter-work. Accessed July 20, 2022.
- Henry Schein Dental. Air Management and Infection Control in the Dental Office Post COVID-19. Available at: henryscheinequipmentcatalog.com/content-library/air-management-infection-control. Accessed July 20, 2022.
- Heo KJ, Park I, Lee G, et al. Effects of air purifiers on the spread of simulated respiratory droplet nuclei and virus aggregates. Int J Environ Res Public Health. 2021;18:8426.
- OSAP. OSAP/CareQuest Institute Best Practices for Infection Control in Dental Clinics During the COVID-19 Pandemic. Available at: osap.org/best-practices-for-infection-control-in-dental-clinics-during-the-covid-19-pandemic. Accessed July 20, 2022.
- Huang Q, Marzouk T, Cirligeanu R, Malmstrom H, Eliav E, Ren YF. Ventilation assessment by carbon dioxide levels in dental treatment rooms. J Dent Res. 2021;100:810–816.
- Zemouri C, Awad SF, Volgenant CMC, Crielaard W, LaheiJ AMGA, de Soet JJ. Modeling of the transmission of coronaviruses, measles virus, influenza virus, Mycobacterium tuberculosis, and Legionella pneumophila in dental clinics. J Dent Res. 2020;99:1192–1198.
- United States Centers for Disease Control and Prevention. Ventilation in Buildings Summary of Recent Changes. Available at: cdc.gov/coronavirus/떓-ncov/community/ventilation.html. Accessed July 20, 2022.
- United States Centers for Disease Control and Prevention. Upper-Room Ultraviolet Germicidal Irradiation (UVGI). Available at: cdc.gov/coronavirus/떓-ncov/community/ventilation/UVGI.html. Accessed July 20, 2022.
- Nunayon SS, Zhang HH, Lai ACK. Comparison of disinfection performance of UVC-LED and conventional upper-room UVGI systems. Indoor Air. 2020;30:180–191.
From Dimensions of Dental Hygiene. August 2022; 20(8)14-17.

