The Dangers of Betel Quid Chewing
This addictive habit, popular in Southeast Asia and India, negatively impacts the oral cavity.
This course was published in the February 2014 issue and expires February 28, 2017. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define the betel nut and how it is prepared for chewing.
- Describe the effects of betel quid use on the oral cavity.
- Explain the possible mechanisms of the caries inhibiting effect of betel quid.
- Identify the signs and symptoms of oral submucous fibrosis.
- Discuss the dental professional’s role in the clinical management of the betel quid user.
Betel nut is the fruit of the areca palm tree. The nut, which is the seed found within the fruit, appears mottled brown with gray-white markings. Users describe it as having a slightly bitter taste and report that it is helpful for digestive and oral health, as well as for facilitating bowel movements, increasing stamina, and improving concentration.1

Betel nuts can be chewed alone, but many cultures mix it with a combination of ingredients. Once mixed together, the term most often used to describe this masticatory drug is betel quid.2 Betel nuts can be combined with catechu gum, which is produced from the sap of the catechu tree; menthol; sandal oil; spices, such as cloves, anise seed, cinnamon, and nutmeg; and finely pounded gold or silver metal.2 These ingredients are then mixed with a calcium hydroxide paste (traditionally referred to as slaked lime) and tobacco and wrapped in a betel leaf (Figure 1 and Figure 2).2 The leaf packet is then sucked on or chewed for 15 minutes to 20 minutes (Figure 3). When it has been chewed thoroughly, the user spits it out.3
The compound produces feelings of euphoria or relaxation, or creates a burst of energy.4 Arecoline, the active ingredient in betel nut, when mixed with calcium hydroxide paste, produces a substance that stimulates the central nervous system.3,5 The stimulated central nervous system induces the feeling of euphoria and may cause increased perspiration and tear production, pupillary constriction, and diarrhea.2
PREVALENCE
Paan, masala, gutka, supari, puwak, gua, mak, pinang, and daka are other names used to describe the betel nut, which is chewed throughout large parts of India, Bangladesh, the Federal Republic of Malanasia, East Africa, and the South Pacific.2,4 Approximately 200 million people chew quid regularly,2,3 making it likely that oral health professionals will encounter patients who engage in this habit. Its use is more common in rural areas,6 and has also gained popularity in parts of Thailand, Indonesia, and the Philippines.7

Through immigration, the habitual chewing of the betel nut has made its way to the United States. The second highest number of legal immigrants to the US comes from India.7 More immigrants from Asian Indian and South Asian subgroups, such as Pakistanis and Bangladeshis, are also coming to the US.7 These populations are mostly concentrated in Northeast metropolitan areas, such as New York, Northern New Jersey, Long Island, and Philadelphia, followed by Chicago and large cities in California.7 Betel nut and the compounds added to it for chewing are easily found in these areas. Two sachets of betel quid are sold for approximately $1. The betel quid’s low cost has lead to increased popularity, especially among young people.7,8
Global availability allows individuals to import part of their homeland, and continued use may be viewed as a way to keep in touch with their culture.8 Individuals who frequently visit their native countries often bring betel quid back to the US. Betel quid is not labeled a controlled substance in the US, but imported betel nuts can be confiscated by US Customs and Border Protection officers based on possible violations of food, agricultural, or medicinal regulations. However, this is rare. Strongly intertwined with social customs, cultural rituals, and religious practices, betel quid chewing is an ancient tradition2,4 that may be unfamiliar to Western health and dental professionals.
ADDICTION

Betel nut is considered the fourth most addictive substance in the world after tobacco, alcohol, and caffeine.9,10 Participants in a study that examined whether betel nut usage could lead to addiction reported repeated use despite knowledge of harm and multiple attempts at abstinence.10 Withdrawal symptoms are also experienced, such as craving, anxiety, fatigue, and sadness.10
In some regions, betel quid chewing begins as early as age 7 among both girls and boys.4,6 Habitual users engage in betel quid chewing during all waking hours.4 Some mothers report giving their infants premasticated quids.4
ORAL MANIFESTATIONS
Betel quid chewing stains the teeth, gingiva, and oral mucosa (Figure 4 and Figure 5). The color of the stain varies from deep red to black, depending on its preparation and the longevity of use.2 Chronic users also develop betel chewer’s mucosa, a condition characterized by deep red or brownish-red discoloration of the oral mucosa with wrinkled incrustations that can be scraped off.5,11 This localized lesion is associated with the site of the betel quid placement, usually the buccal mucosa.5 The oral mucosa tends to desquamate or peel with loose detached tags of tissue also evident.11 In some cultures and societies, this change in color is considered a sign of beauty.3 Though some chewers try to reduce the amount of discoloration with intense toothbrushing, the substances used in its preparation will still produce significant discoloration if regular professional dental care is not obtained.5 This stain naturally adheres to pits and fissures, calculus, rough filling surfaces, and naturally rough areas of the teeth.3,5

Consistent chewing of betel quid often produces severe wear on the incisal and occlusal tooth surfaces.5 The degree of attrition is dependent on the consistency of the betel quid and how often and for how long it is chewed.5 Chronic betel quid users may also experience root fractures due to constant mastication and the burden the habit places on the teeth.5 The ongoing flexion, compression, and tension that betel quid chewing places on the cervical area of the tooth can result in abfraction, and, eventually, loss of cervical tooth structure.12
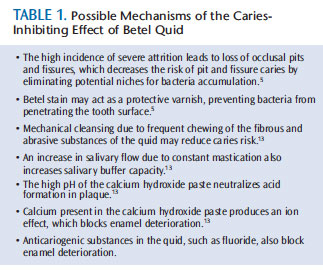
Despite the severe attrition that betel users experience, their risk of caries is reduced.5,13 Explanations for this inverse relationship range from an increase in salivary flow and anticariogenic substances in the betel quid to the high pH of the quid that neutralizes the acid in the oral cavity. Table 1 lists possible mechanisms of the caries-inhibiting effects of betel quid.
In vitro studies have shown that the active ingredient in betel nut—arecoline—inhibits the growth of attachment in human-cultured periodontal fibroblasts.5,14 Therefore, betel nut may be cytotoxic to periodontal fibroblasts and may exacerbate pre-existing periodontal diseases, as well as hinder periodontal reattachment.5,14 Studies have also shown that betel quid users experience more loss of periodontal attachment and increased calculus formation than nonusers.5
ORAL SUBMUCOUS FIBROSIS

Epidemiologic studies have discovered that long-term betel quid chewing increases the risk of oral submucous fibrosis (OSF).5,15 A chronic, progressive condition of the oral cavity,16 OSF?is characterized by fibrosis of the mucosal lining of the upper digestive tract, oral cavity, and lamina propria. OSF affects 2.5 million people.15 The exact mechanism and etiology are unclear; however, when buccal mucosal cells are exposed to the active ingredient in betel nut, there is an increased accumulation of collagen, along with a reduction of collagenase, which then results in an inability to break down the excess collagen.16 Histological findings of OSF show an increase in fibroblasts and a cross-linking of fibers.16 The retromolar areas, buccal mucosa, soft palate, tongue, and lips are frequently affected.15 The tongue stiffens and exhibits limited protrusion and papillary atrophy.15 Patients with OSF often present with a past history of pain and sensitivity to spicy foods.15 Other signs and symptoms include an increase in saliva, altered taste, vesicle formation on the palate, and a nasalized voice.15 A marble-like appearance of the oral mucosa that can either be localized or diffuse is also an early sign of OSF.15 This chronic disease results in a limited opening of the oral cavity, which is associated with stiffening of the oral mucosa by fibrous bands.5,15 Patients with OSF often experience difficulty in eating, swallowing, and speaking.3,15 Mucosal leukoplakia may accompany OSF, and is regarded as a precancerous condition with a 7.6% malignancy transformation rate.3,17 The calcium hydroxide component of the betel quid and arecoline—the active ingredient in betel nut—may be related to the development of OSF.2
ORAL CANCER
The tobacco content in betel quid places the user at risk for oral cancer. Oral cancer is the sixth most common malignancy in the world.18 More common than cancers of the liver, brain, and bone, oral cancer kills approximately one person per hour.18 Betel quid use coupled with tobacco is listed as a carcinogen by the International Agency for Research on Cancer.2 Betel quid chewing associated squamous cell carcinomas occur along surfaces where the betel quid is held, specifically the lateral borders of the tongue and the buccal mucosa.3 Oral squamous cell carcinomas may occur independently or in association with OSF.3 Studies show that the incidence of oral cancer is increased in regions where betel quid is chewed.19 India has the largest betel quid chewing population in the world, as well as an increased prevalence of OSF and oral squamous cell carcinomas.3,4 In Southeast Asia, 30% of oral cancers are caused by the habitual chewing of betel quid containing tobacco.2 Reports show that betel nut and tobacco act synergistically to produce oral cancer.2 The prognosis of oral cancers is dependent on its timeframe of identification; therefore, early detection and treatment are key.
CLINICAL MANAGEMENT
Patients who present with deep-red stains on the teeth, gingiva, and oral mucosa should be educated about eliminating betel quid chewing and increasing oral self-care to prevent recurrence of stain.20 Effective toothbrushing twice a day, in addition to regular dental visits, are recommended to reduce the extrinsic stain accumulation caused by betel quid chewing.21,22 Dental hygienists should carefully examine the teeth to document the position and distribution of the stain, roughened enamel surfaces, enamel defects, and attrition, as well as plaque and calculus accumulation.22 Areas of severe attrition and abfraction should be evaluated for fractures and necessary treatment.12 Extrinsic staining caused by this habit should be treated with a thorough dental prophylaxis after scaling is complete.20 Both power scalers and hand scalers can remove betel nut staining.21 Due to the potential of pitting and damage to the enamel surface, stain removal should be completed systematically and carefully.20 Areas where cementum and dentin are exposed should not be treated with the rubber cup polisher because of the fragility of the enamel surface in betel quid chewers.20
For patients with OSF, there are few treatment options. Medical/surgical interventions and/or physical therapy may be helpful.9 Surgery focuses on relieving the stiffening of the oral cavity by incising the fibrosis bands, while physical therapy focuses on alleviating muscle tension.16 Nonsurgical methods of managing OSF include the use of corticosteroids to relieve early symptoms, proteolytic enzymes to decrease collagen formation, and vitamin therapy.16
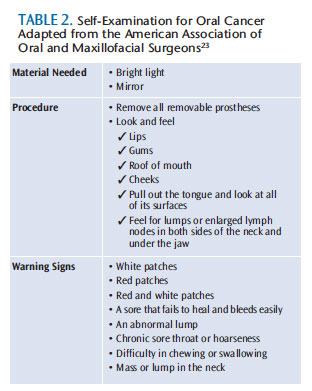
Due to the increased risk of oral cancer, as well as the risk of OSF becoming malignant, betel quid users must receive routine oral cancer screenings and extensive documentation of soft tissue lesions. Teaching patients how to perform a monthly oral cancer self-examination is important for early detection and favorable outcomes.23 Table 2 provides details on performing an oral cancer self-examination.
CESSATION STRATEGIES
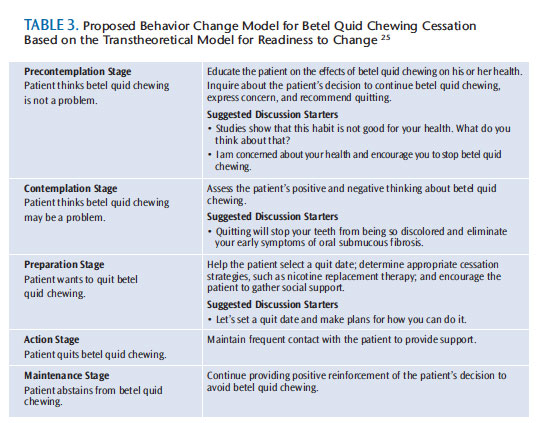
Cessation of betel quid chewing should be strongly encouraged, and patients should be assisted with quitting.2,3 No clear directive has been given on a cessation program for betel quid chewing; however, because of its addictive properties and the presence of tobacco, traditional tobacco cessation models are appropriate for this patient population. The use of nicotine gum can address nicotine dependency, as well as replace the associated masticatory habit.8 Use of the 5As (Ask, Advise, Assess, Assist, Arrange) is a common strategy in tobacco cessation—though this model of behavioral change is aimed at individuals who are ready to quit and it may not be helpful for those who are in the precontemplation or contemplation stage of changing the addictive behavior.24
The Transtheoretical Model for Readiness to Change may be more appropriate for use in eliciting behavior changes among betel quid users (Table 3). This model is a stage-based theory of how behavior change occurs.24 It encompasses five stages: precontemplation—patient does not believe that his or her habit is a problem or refuses to consider cessation; contemplation—patient recognizes that the habit is a problem and expresses a desire to quit the addictive behavior; preparation—the patient makes specific plans for cessation of the addictive habit; action—patient stops the addictive habit; and maintenance—the patient continues to employ methods and strategies to stay free of the addictive habit.25
CONCLUSION
In the US, education, prevention, and treatment efforts focus on conventional tobacco use. As such, expanded research addressing interventions for betel quid chewing cessation is needed.7 Dental hygienists’ active involvement in educating the community on the dangers of betel quid chewing, and encouraging policy changes that regulate the use and sale of purified preserved betel nut preparations to minors, is extremely important in decreasing the potential explosion of oral cancer in this growing population.7 US census reports from 2010 estimate that 40 million US residents, or 13% of the total population, are foreign-born.26 The possibility of treating a betel quid chewer is extremely likely. Once users are identified, their oral condition should be monitored and education and assistance in quitting betel quid use should be provided.
ACKNOWLEDGEMENTS
The author would like to thank dental hygiene student Syed Hossain at Eugenio María de Hostos Community College for inspiring her to write this article. Hossain also provided the accompanying photos.
- Lingappa A, Nappalli D, Sujatha G, Prasad S. Areca nut: To chew or not to chew? Available at: ejournalofdentistry.com/articles/e-JOD3 BC4F9E2-1D5E-4659-A0C3-DAD2ABA83528.pdf. Accessed January 21, 2014.
- Nelson BS, Heischober B. Betel nut: a common drug used by naturalized citizens from India, Far East Asia, and the South Pacific islands. Ann Emerg Med. 1999;34:238–243.
- Norton SA. Betel: consumption and consequences. J Am Acad Dermatol. 1998;38:81–88.
- Gupta PC, S. Global epidemiology of areca nut usage. Addict Biol. 2002;7:77–83.
- Trivedy CR, Craig G, Warnakulasuriya S. The oral health consequences of chewing areca nut. Addict Biol. 2002;7:115–125.
- Wang S, Tsai C, Huang S, Hong Y. Betel nut chewing and related factors in adolescent students in Taiwan. Public Health. 2003;117:339–345.
- Changrani J, Gany FM. Paan and gutka in the United States: an emerging threat. Journal of Immigrant Health. 2005;7(2):103–108.
- Winstock A. Areca nut-abuse liability, dependence and public health. Addict Biol. 2002;7:133–138.
- Kerr A, Warnakulasuriya S, Mighell A, et al. A systematic review of medical interventions for oral submucous fibrosis and future research opportunities. Oral Dis. 2011;17:4–57.
- Benegal V, Rajkumar RP, Muralidharan K. Does areca nut use lead to dependence? Drug Alcohol Depend. 2008;97:114–121.
- Zain RB, Ikeda N, Gupta PC, et al. Oral mucosal lesions associated with betel quid, areca nut and tobacco chewing habits: consensus from a workshop held in Kuala Lumpur, Malaysia, November 25-27, 1996. J Oral Pathol Med. 1999;28:1–4.
- Kim JJ, Karastathis D. Dentinal hypersensitivity management. In: Darby ML, Walsh MM, eds. Dental Hygiene Theory and Practice. 3rd ed. St. Louis: Saunders; 2010:726.
- Möller IJ, Pindborg JJ, Effendi I. The relation between betel chewing and dental caries. Eur J Oral Sci. 1977;85:64–70.
- Chang MC, Kuo MY, Hahn LJ, Hsieh CC, Lin SK, Jeng JH. Areca nut extract inhibits the growth, attachment, and matrix protein synthesis of cultured human gingival fibroblasts. J Periodontol. 1998;69:1092–1097.
- Cox SC, Walker DM. Oral submucous fibrosis. a review. Aust Dent J. 1996;41:294–299.
- Anusushanth A, Sitra G, Dineshshankar J, Sindhuja P, Maheswaran T, Yoithapprabhunath T.Pathogenesis and therapeutic intervention of oral submucous fibrosis. J Pharm Bioall Sci. 2013;5:85–88.
- Sinor PN, Gupta PC, Murti PR, et al. A case-control study of oral submucous fibrosis with special reference to the etiologic role of areca nut. J Oral Pathol Med. 1990;19:94–98.
- Gurenlian JR. Screening for oral cancer. Available at: cdeworld.com/courses/20000-Screening_for_Oral_Cancer#. Accessed January 21, 2014.
- Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century—the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol.2003;31:3–23.
- Dolan JJ. Management of extrinsic and intrinsic stains. In: Darby LM, Walsh MM, eds. Dental Hygiene Theory and Practice. 3rd ed. St. Louis: Saunders; 2010:511.
- Prathap S, Rajesh H, Boloor VA, Rao AS. Extrinsic stains and management: a new insight. Journal of Academia and Industrial Research. 2013;1(8):435.
- Hattab FN, Qudeimat MA, al-Rimawi HS. Dental discoloration: an overview. J Esthet Dent. 1999;11:291–310.
- Oral and Maxillofacial Surgeons Head, Neck and Oral Cancer. Available at: myoms.org/procedures/head-neck-and-oral-cancer. Accessed January 21, 2014.
- Aveyard P, Massey L, Parsons A, Manaseki S, Griffin C. The effect of transtheoretical model based interventions on smoking cessation. Soc Sci Med. 2009;68:397–403.
- Mallin R. Smoking cessation: integration of behavioral and drug therapies. Am Fam Physician. 2002;65:1107–1122.
- Grieco EM, Acosta YD, de la Cruz P, et al. The Foreign-Born Population in the United States: 2010. Available at: census.gov/prod/ 2012pubs/acs-19.pdf. Accessed January 21, 2014.
From Dimensions of Dental Hygiene. February 2014;12(2):65–69.



