
The Battle Against Biofilms
Keeping dental unit waterlines free from bacterial contamination is essential to ensuring patient and provider safety.
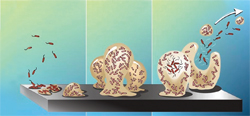
Biofilms are a collection of microorganisms firmly attached to a moist surface by a slimy matrix that can survive in a variety of environments. Biofilms are found in nature, industry, and health care settings—including dental unit waterlines (DUWLs). Two forms of bacteria are related to biofilm formation: planktonic (single free-floating) and attached communities (groups or clusters). Initially, planktonic bacterial cell walls adhere to surfaces using a polymer (glycocalyx). More and more bacteria begin to proliferate and colonize, giving the complex microbial colony a protective slimy layer (Figure 1).
DUWLs are ideal environments for biofilm formation because they are made of narrow tubing material, and there is a risk of stagnant water remaining in the lines.1 DUWLs include tubing to the air/water syringe and handpiece lines. Microorganisms thrive, colonize, and proliferate on the inner surface of waterline tubing—creating biofilms.2 Outgoing water from the dental unit may be contaminated if planktonic bacteria or pieces of biofilm break off and enter the water stream.1,3
CLINICAL IMPLICATIONS
Numerous waterborne microorganisms have been identified in DUWLs, but most are not pathogenic to patients with healthy immune systems.4,5 Unfortunately, some of these species, such as Pseudomonas, Legionella, and Mycobacterium, can be harmful or deadly to immunocompromised patients who are more susceptible to infections. In 2011, an otherwise healthy 82-year-old woman died from irreversible septic shock after acquiring Legionnaire’s disease (Legionella pneumophila) from dental unit water used during treatment.6 As more immunocompromised patients are treated in general dental practices, reducing exposure risk to harmful pathogens is important.3,7,8
GUIDELINES FOR DENTAL UNIT WATER QUALITY

In 1995, the American Dental Association (ADA)2 made a formal statement about the need for improvements in outgoing water quality levels in dental units and called for dental industry manufacturers to design equipment capable of delivering outgoing water levels of <200 colony-forming units (CFU/mL). The <200 CFU/mL threshold was based on safe levels previously established for fluids used in hemodialysis.5 The Environmental Protection Agency (EPA), the American Public Health Association, and the American Water Works Association set standards5 for safe drinking water at <500 CFU/mL. The 2003 Centers for Disease Control and Prevention (CDC) Guidelines for Infection Control in Dental Health-Care Settings5 state that bacterial counts in outgoing dental unit water (for nonsurgical procedures) should be “as low as reasonably achievable” and must minimally meet EPA drinking water standard of <500 CFU/mL.
Dental unit manufacturers rose to the challenge from the ADA (and subsequent CDC guidelines) and developed equipment that meets EPA safe water standards. Today, a wide variety of devices and cleaning/disinfectant treatment products are available to help dental practices meet these guidelines.
WATER QUALITY BASICS
Staff education, scheduled maintenance, and record keeping help to ensure that DUWLs meet EPA safe drinking water standards. 3,5 Without these measures, biofilms will continue to proliferate and may cause serious harm to patients. The CDC and the Healthcare Infection Control Practices Advisory Committee have categorized the recommendations provided by the CDC infection control guidelines. These categories range from strongly recommended for implementation based on research and strong theoretical rationale (IA and IB), required implementation mandated by federal or state standards (IC), to no recommendation at all (unresolved issue). When category IC (required) is used, a second rating can be added to provide the scientific basis for the recommendation. Category II means that the recommendation is supported by studies or theory.
The following recommendations from the Organization for Safety, Asepsis and Prevention (OSAP)3 and the CDC5 are designed to ensure DUWL safety.

- Consult with the manufacturer of the dental unit to obtain directions on DUWL products and protocols that can be used with the unit to ensure proper maintenance scheduling (category II).5
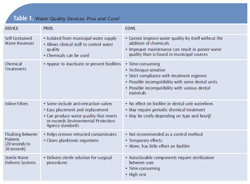
- Use commercially available devices, products, and procedures, including self-contained water reservoirs (Figure 2) with added cleaning agents designed to isolate water from municipal supplies (Figure 3); chemical or antimicrobial treatments designed to inactivate biofilms; slow release cartridges to prevent biofilm attachment; inline microfilters; or a combination of these (category IB, IC).5 Products that carry a disinfectant claim must be EPA-registered.9 Devices for waterline treatment that are attached to the dental unit must be registered with the federal Food and Drug Administration (FDA) as medical devices.9 Table 1 provides a discussion of the pros and cons of commonly used water quality devices.
- Use safe source water (<500 CFU/mL) which includes, tap, distilled, or sterile water (category IB, IC).5
- Maintain self-contained water reservoirs according to manufacturer’s instructions to prevent contamination. Self-contained water alone will not eradicate biofilm formation in the DUWL, so controlling the quality (either periodically or continuously) via devices, products, or procedures is necessary.5
- Flush all DUWLs for 20 seconds to 30 seconds between patients to remove any possible contamination from the previous patient. Most dental units are equipped with anti-retraction valves to prevent “suck-back” of contaminated fluid.5 Even with these valves, flushing is still recommended (category II).5 There is no longer a need to flush DUWLs for 1 minute to 2 minutes at the beginning of the day, because firmly adherent biofilms are not dislodged by flushing alone, therefore, flushing for 20 seconds to 30 seconds is adequate to clear stagnant lines.5 Flushing alone does not qualify as good quality control.5
- Retrofit dental units that are more than 20 years old with anti-retraction valves (category IB).5
- If municipal water is used, install a point-of-use filter between the DUWL tubing and the instrument, or retrofit the unit for a self-contained water system.5
MONITORING WATER QUALITY
To ensure safe water standards, all clinical staff members should be educated about dental unit water quality, biofilm, water treatment, and dental unit maintenance including monitoring of water quality.3,5 Monitoring water quality helps determine the safety of the outgoing dental unit water and staff compliance with monitoring schedules. Dental unit manufacturers should be consulted for proper instructions and recommended monitoring schedules to maintain safe water standards.3,5 Monitoring of dental unit water quality can be achieved by one of two methods: commercial water testing products/kits used in the office or a water testing laboratory service.5 Commercial testing laboratories use a gold standard test (Method 9215C with R2A agar) to determine exact bacterial CFU counts. In-office water testing kits are screening tools that may provide consistent results when compared to Method 9215C.10 Research findings on the efficacy of in-office testing products are mixed and more study is needed.10 They are easy to use, which can increase compliance, but they may not provide consistent results when compared to laboratory testing.
Compliance with monitoring protocols is important, no matter which testing method is used. The CDC guidelines do not outline specific (or standardized) procedures or maintenance schedules for monitoring dental unit water. Monitoring is dependent on the clinical staff as well as the dental unit and product manufacturer’s recommendations. OSAP3 recommends testing water before any chemical treatments are administered, when new products or protocols are used, and if a new employee is taking on the water testing responsibility.
Effective water monitoring is based on a variety of factors. Proper infection control standards should be adhered to in order to avoid contamination when collecting samples.3 All manufacturer instructions should be followed and records of monitoring results need to be kept for each unit in the practice.3
MAINTENANCE OF DENTAL UNIT WATERLINES
Once the quality of the dental unit water is determined, initial, periodic, or continuous chemical “shock” treatments are recommended to enhance the performance of waterline treatment products and to reduce or eliminate biofilm.9Some products are used initially or periodically to reduce or eliminate biofilm, while others provide continuous chemicals in the waterline to deter biofilm formation.
Periodic treatments require purging of the waterline, adding chemical additives to the water reservoir, filling the lines for the recommended time period, and then flushing. Continuous chemical treatments with automated metering devices release low levels of chemicals into the treatment water to control biofilm—lowering bacterial counts in the water.9 Some products require a combination of periodic and continuous shocking.
After shock treatments are administered, routine maintenance procedures and schedules should be followed according to manufacturer instructions. Depending on the product or unit, these guidelines typically include daily, weekly, quarterly, and/or annual protocols.
SURGICAL PROCEDURES
Oral surgical procedures put patients at increased infection risk because of the invasive nature of these procedures, so sterile solutions must be used for irrigation and cooling. Traditional dental units cannot always deliver sterile water due to biofilm formation in DUWLs, so sterile irrigation solutions are recommended for oral surgical procedures.5 The CDC recommends that surgical hand antisepsis be performed by using an antimicrobial product (eg, antimicrobial soap and water, or soap and water followed by alcohol-based hand scrub with persistent activity) before donning gloves (category IB). Sterile surgeon’s gloves must be worn (category IB). Sterile saline or sterile water should be used as a coolant/irrigant when performing oral surgical procedures. Only devices specifically designed for delivering sterile irrigating fluids (eg, bulb syringe, single-use disposable products, and sterilizable tubing) should be implemented (category IB).5
BOIL-WATER ADVISORIES
Drinking water is monitored by city municipalities according to EPA standards and is generally safe. Contamination, however, sometimes occurs for a variety of reasons, such as failures in water treatment processes, harmful pathogens identified in the water supply, violations of coliform rules, water main breakages, and natural disasters.5 When these events occur, boil-water advisories are issued as a public health announcement indicating that tap water is not safe to drink unless it is first boiled. OSAP has an excellent Boil-Water Advisory Toolkit9 available at www.osap.org.
During a boil-water advisory, the CDC recommends against using water from the public water system in any manner where patients would be exposed, including dental treatment, patient rinsing, or handwashing (category IB, IC). Hand hygiene should be conducted with antimicrobial-containing products that do not require water for use (eg, alcohol-based hand rubs). If hands are visibly contaminated, bottled water and soap should be used or an antiseptic towelette (category IB, IC).5
After a boil-water advisory is cancelled, clinicians should follow the guidelines provided by the local water utility regarding adequate flushing of waterlines. If no guidance is provided, flush dental waterlines and faucets for 1 minute to 5 minutes before using for patient care (category IC).5 Dental waterlines should be disinfected as recommended by the dental unit manufacturer (category II).5
THE BOTTOM LINE
Prudent infection control policies and practices are vital in providing safe patient care. Monitoring and maintenance of dental unit water quality is an essential part of routine infection control practices. All dental staff should be trained and calibrated to ensure that dental equipment is maintained properly to produce acceptable water quality standards of <500 CFU/mL set forth by the EPA and recommended by the ADA and the CDC.
REFERENCES
- Liaqat I, Sabri AN. Biofilm, dental unit water line and its control. Afr J Clin Exper Microbiol. 2011;12:15–21.
- American Dental Association. Statement on Dental Unit Waterlines. Available at: www.ada.org/1856.aspx. Accessed August 22, 2012.
- From Policies to Practice: OSAP’s Guide to the Guidelines: Workbook. Annapolis, Md:Organization for Safety, Asepsis and Prevention;2004.
- Miller CH, Palenik CJ. Infection Control and Management of Hazardous Materials for the Dental Team.4th ed. St. Louis: Mosby Elsevier;2010.
- Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection control in dental healthcare settings—2003. MMWR Recomm Rep.2003;52:1–66.
- Ricci ML, Fontana S, Pinci F, et al. Pneumonia associated with a dental unit waterline. Lancet. 2012;379:684.
- Mann PC. Training future dental clinicians an integrated approach to health care.NY State Dent J. 2009;75:32–35.
- Radfar L, Lakshmanan S. Medical profile of a dental school patient population. J Dent Educ.2007;71:682–686.
- Organization for Safety Asepsis and Prevention.Dental Unit Waterlines. Available at: www.osap.org/?page=Issues_ DUWL_ 1&hh Search Terms=dental+ and+unit+and+ waterlines. Accessed August 22, 2012.
- Cohen ME, Harte JA, Stone ME, O’Connor KH, Coen ML, Cullum ME. Statistical modeling of dental-unit water bacterial test kit performance.J Clin Dent. 2007;18:39–44.
From Dimensions of Dental Hygiene. September 2012; 10(9): 28; 30-33.

