 EDWARDOLIVE/ISTOCK/GETTY IMAGES PLUS
EDWARDOLIVE/ISTOCK/GETTY IMAGES PLUS
Supporting the Longevity of Dental Implants
Dental hygienists play a critical role in the success of implant therapy.
This course was published in the January 2022 issue and expires January 2025. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify current implant market trends.
- List the materials used for implant parts.
- Discuss the factors contributing to implant failures.
- Recognize the importance of dental hygienists in the success of dental implants.
Modern-day implants offer creative solutions for restoring edentulous areas.1 Implants provide support for the orofacial structures; however, they also present many challenges for dental practitioners and patients alike. Thus, proper treatment planning, placement, and oral care pre- and post-treatment are critical for the longevity of dental implants and optimal patient health.
Dental hygienists are well versed in helping patients preserve their natural dentition. However, tooth loss affects a large number of Americans. Data from the American College of Prosthodontists suggest that more than 36 million Americans are edentulous and 120 million have at least one missing tooth.2 The National Institute of Dental and Craniofacial Research reports that nearly a third of those older than age 65 are edentulous.3 Those at greatest risk for edentulism are older adults, active smokers, and individuals with less education or low socioeconomic status.
An average implant treatment takes a year to complete and costs approximately $4,000 per fixture.4 Advanced technologies, such as three-dimensional digital imaging and surgical planning software, help make implant treatments more predictable, safe, fast, and affordable.1 With these changes, the implant market is projected to nearly double from $3.9 billion in 2018 to $7.4 billion in 2027.5 As such, dental hygienists will experience a significant influx of patients with dental implants and should be prepared to support their longevity.
Materials Used for Implant Parts
In order to support the long-term care of implants, dental hygienists should be familiar with the materials used to fabricate implant components, including a post, abutment, and prostheses (fixed or removable). Implant-supported fixed prostheses include crowns or bridges, and they can be cemented or screw-retained. Table 1 lists the materials used for fixed prostheses. Implant-supported removable restorations— used as part of overdenture, hybrid, and telescopic structures—can be made of acrylic, composites, polymethyl methacrylate, or high-performance polymers.6
The implant abutment, or the portion of the implant to which a dental restoration is attached by a screw or cementation, is typically made of titanium or zirconia. The implant post, which makes up the body of the implant and is surgically placed in the jawbone, is also prefabricated in titanium or zirconia. Both titanium and zirconia exhibit excellent mechanical strength, fracture toughness, biocompatibility, tissue integration, and low plaque affinity. Titanium is preferred for its durability, low level of toxicity, and high corrosion resistance. On the other hand, zirconia improves esthetics and helps to avoid or reduce the occurrence of soft-tissue complications. Because allergic reactions to titanium, while rare, have been reported, zirconia also provides an alternative for patients sensitive to titanium.7–11
One of the most significant drawbacks of titanium is its dark gray color, which is especially visible in areas with thin tissue or gingival recession. Yet, this thin oxide layer, called titanium dioxide (TiO2), which is formed by exposure of titanium to air or water, allows implant biocompatibility with surrounding structures. TiO2 also decreases the release of metallic ion from implant to neighboring tissue, minimizes adverse body reactions, and greatly aids in osseointegration.12 To mask the grayness, the anodization process can be utilized to change the hue of the titanium surface.13 It uses an electric current to speed up the oxidization process, creating a thicker oxide layer (less than 1 µm) while increasing surface roughness and hardness without modifying the material’s properties. The higher the voltage, the thicker the oxide layer. When the titanium part is placed in an electrolytic bath, and the exact voltage is applied, light reflections from titanium and oxide layer result in different surface colors. For example, 65 volts generate a gold hue used on substructures for fixed restorations, while 75 volts produce a pink surface finish utilized in substructures made for dentures. Anodized titanium is very durable in the oral environment, but friction or scratches can damage the surface.14
Zirconia exhibits tooth-like color and minimal ion release.11 Disadvantages include microcracks and stress breaks attributed to many factors, including incorrect design or fabrication where dull burs used in the milling process create minor fractures that grow under pressure and cause breakage over time.15 Also, modifying the surfaces of zirconia is challenging. Yet, studies show that osseointegration, surface roughness, and stress distribution of zirconia are comparable to those of titanium implants.11
Various implant designs and surface treatments influence osseointegration by generating better biological and mechanical connections between the implant and the alveolar bone. Tapered implant designs create better bone osseointegration, add stability, and reduce the risk of micro gaps and micro-movements.16 Mechanical, chemical, and physical surface modifications of implant posts achieve a long-lasting bond between the bone and the implant.
Mechanical treatments create rougher or smoother implant surfaces and incorporate grinding, machining, and blasting. Blasting removes parts of the implant material, creating slight irregularities and roughened surfaces. Machining leaves grooves and ridges on the implant surface, and grinding produces coarseness contributing to better bone-implant connection.10
Chemical modifications alter surface topography and composition while enhancing surface energy. They include acids, alkali, sol gel, or anodization processes.10 When strong acids are applied to implant surfaces, they increase surface roughness and surface area. Alkali-etching creates a porous, hydrated, and reactive titanium oxide surface.17 On the other hand, the sol-gel process deposits biocompatible hydroxyapatite to the implant’s surface to improve osseointegration and provide antibacterial and anticorrosive properties.18 Anodization is an electromechanical process that thickens and roughens the oxide layer.10,16
Physical modifications influencing connections between the implant and the alveolar bone include plasma spraying and ion deposition. Plasma spraying involves tiny particles of metal or ceramic sprayed with a plasma torch creating a thick coating with a high level of adhesion. The ion deposition creates a specific pattern on the surface of an implant for better adhesion.10,16,19
Some surface modification techniques have fallen out of favor, while others are growing in popularity such as sandblasting and acid etching. However, studies of implant surface treatments show either variable results or suggest that most implants are comparable to each other regardless of their morphological characteristics, surface structures, or types.10,20 With current techniques of producing surface irregularities, the processes creating the most predictable osseointegration and implant longevity are still being researched. 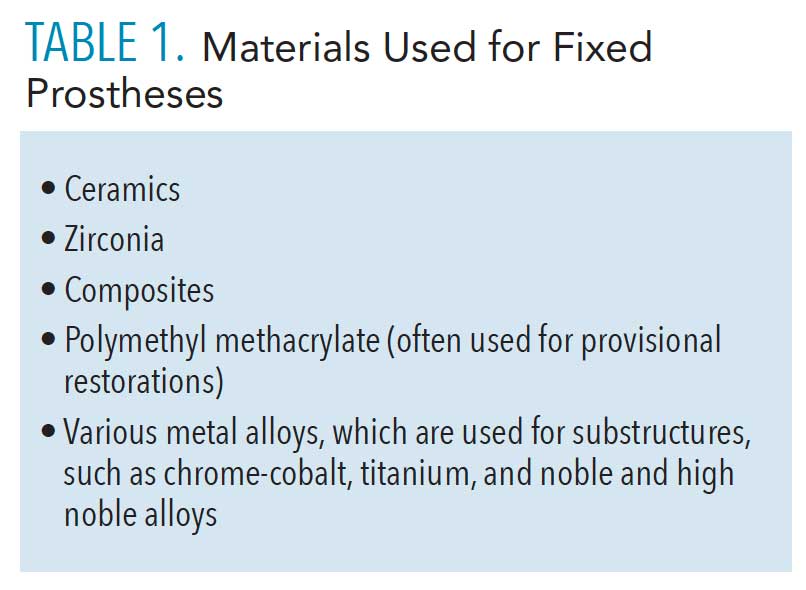
Implant Failures
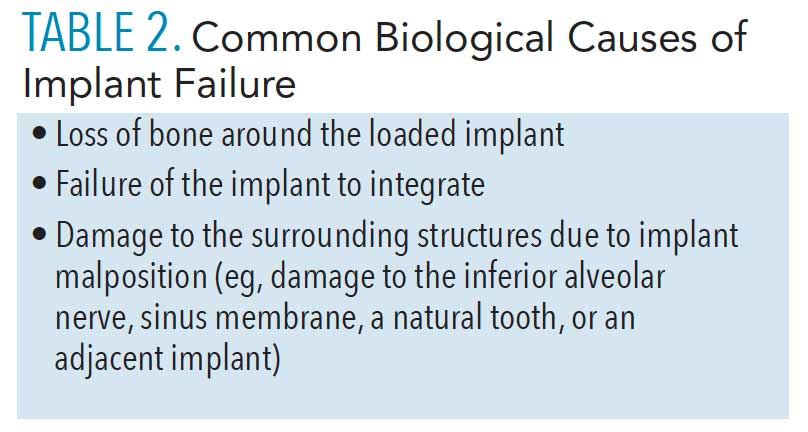
The long-term success of implants and dental prostheses depends on biological and mechanical factors. Biological aspects include the health of the tissue and bone, whereas mechanical elements rely on the stability of the implant parts and the final restorations.21 Table 2 (page 36) lists common biological failures. Implant failures are often initiated by inflammatory processes, leading to peri-implant mucositis and peri-implantitis.21–23 Mechanical failures of implant parts include mobility, fractures, breakage, or implant removal. Implant design, surface treatment, and surrounding bacteria determine how the bone grows to the top of the implant and how the tissue follows the bone.22
Most implant failures can be classified as early failures, occurring before osseointegration, or late failures, after implant integration and loading. Early failures may occur due to the bone overheating at the time of placement, surface contamination at the time of surgery, implant placement at a site where periapical pathology existed on the extracted tooth, overloading provisionalized immediately placed implant, or lack of initial stability (eg, placement in poor-quality bone). Late failures may include implant overload and peri-implantitis. The overload may happen due to incorrect implant or restoration designs, along with patient habits. These could include not enough implants placed to balance the occlusal load, large cantilevers, steep cuspal inclines, poor distribution of force, occlusal interferences, and parafunctional habits such as bruxism and clenching.22
Importance of Dental Hygienists
Dental hygienists play an essential role in customizing oral care to meet patients’ needs during the entire implant treatment process. Applying motivational interviewing techniques to establish suitable oral hygiene habits in order to prevent the formation of biofilm-induced diseases surrounding teeth and implants is key to implant success. Considering that dental implants are a significant investments in oral health, a 3-month recare regimen should be maintained until the patient has demonstrated acceptable oral hygiene around the implants. At each visit, dental hygienists can identify biological (bone and tissue) or mechanical (implant parts) areas of concern. If excess cement is not removed, it can cause peri-implantitis, increase risk of bone loss, and affect the restoration’s longevity. If pain is present, it most likely comes from the areas surrounding the implant rather than the inert implant itself. Inflammation or bone loss may occur due to abutment connection linked to the smooth neck of an implant, excessive stress and strain from occlusion, parafunction, or cantilever length. Other signs of inflammation include mobility, exudate, peri-implant mucositis, or peri-implantitis, which should be examined by light peri-implant probing, assessment of bleeding on probing, and a radiographic examination.23–25
Evaluating fixed or removable implant prostheses requires different hygiene protocols. For removable prostheses, detaching the denture from the implant fixtures allows easier access and care for the implants, denture, and soft tissue. Inflammation, irritation, plaque buildup, and peri-implant diseases around the denture implants may occur. Broken, cracked, or missing attachment pieces should be documented and communicated to the patient.
Implant-supported fixed restorations—such as hybrid dentures, which cannot be removed—are custom designed with space between the prosthesis and jawbone to improve access and aid cleaning. Food impaction, impingement, and inflammation may occur here.26 Fixed restorations are maintenance intensive and should be checked for excess cement, mobility, loose implant screws, and load distribution.23
Materials used for dental implants tend to be fairy resistant to biofilm accumulation.23 Compared to natural teeth, the calculus formed on the nonporous titanium implant surface tends to be softer and mostly supragingival.27 If daily oral hygiene is inadequate or poor, however, calcified supragingival calculus will form. Research shows that certain instruments and abrasive materials produce scratches on implant surfaces that retain biofilm, which contributes to plaque and calculus buildup.23 Ideally, the instruments used on smooth surfaces should produce minimal or no surface damage, which could cause bacterial colonization and affect implant-soft tissue interface. The use of air polishers with glycine may help preserve smooth and rough implant surfaces. Hand scaling instruments, preferably made from titanium, are most effective; however, they may also damage the surface of the titanium implant by scratching it and should be used with caution.28,29
 Traditional dental hygiene instruments are manufactured in stainless steel and titanium. When these dissimilar metals are used together in an oral environment, they may cause galvanic reaction and corrosion, leading to crestal bone loss. Also, stainless steel instruments will scratch the surface of titanium. Thus, stainless steel instruments are not recommended for use on implants.30 Graphite scalers leave graphite particles behind, irritate the tissue, and scratch the surface. Filled resins are also problematic because glass, fibers, or sand fillers, which make resin stronger, leave tiny particles behind, irritating the tissue and scratching implant parts. The safest and most effective hand implant scaling instruments are unfilled resin scalers that produce no scratches.23,25,30 Yet, plastic instruments are the least effective in removing deposits.31 According to a 2013 study published by the American Dental Hygienists’ Association, “unfilled resin was found consistently to be the least damaging to abutment surfaces, although all scalers of all compositions caused detectable surface changes to polished surfaces of implant abutments.”32 Presently, a titanium implant scaler or titanium ultrasonic insert/tip is recommended to successfully remove the calculus or residue from the implants and prevent any instrument residue left behind on titanium and ceramic implants.33
Traditional dental hygiene instruments are manufactured in stainless steel and titanium. When these dissimilar metals are used together in an oral environment, they may cause galvanic reaction and corrosion, leading to crestal bone loss. Also, stainless steel instruments will scratch the surface of titanium. Thus, stainless steel instruments are not recommended for use on implants.30 Graphite scalers leave graphite particles behind, irritate the tissue, and scratch the surface. Filled resins are also problematic because glass, fibers, or sand fillers, which make resin stronger, leave tiny particles behind, irritating the tissue and scratching implant parts. The safest and most effective hand implant scaling instruments are unfilled resin scalers that produce no scratches.23,25,30 Yet, plastic instruments are the least effective in removing deposits.31 According to a 2013 study published by the American Dental Hygienists’ Association, “unfilled resin was found consistently to be the least damaging to abutment surfaces, although all scalers of all compositions caused detectable surface changes to polished surfaces of implant abutments.”32 Presently, a titanium implant scaler or titanium ultrasonic insert/tip is recommended to successfully remove the calculus or residue from the implants and prevent any instrument residue left behind on titanium and ceramic implants.33
The lateral pressure exerted during instrumentation must also be considered because excessive force or trauma to the perimucosal seal can increase the risk of peri-implant biofilm disease. Thus, unnecessary pressures to the surface of the post, abutment, and restoration should be avoided.23,30 Further, to reduce the risk of implant part fractures, occlusal guards are recommended when parafunctional habits are present.34
Throughout treatment, oral care instructions should include detailed verbal and visual guidance. Afterward, the patient’s oral upkeep should be reevaluated during regularly scheduled hygiene visits. It’s also important to remember that mechanical plaque control is contraindicated during post-surgical oral care during the healing period; instead, chemical agents (eg, chlorhexidine) are recommended.27 Once implants fully heal, dental hygienists can promote brushing at least twice a day with a soft toothbrush or power toothbrush in conjunction with professionally recommended antimicrobial mouthrinse and interproximal cleaning using interdental brushes with plastic-coated wires, soft picks, rubber tip stimulators, or air/water flossers, as they are safe and effective.35 However, patients should avoid ordinary dental floss because leftover threads may lead to peri-implant disease.36
Many factors contribute to the success of implant-related treatments. Professional oral care remains vital in the delivery of biofilm management therapy. In addition to providing analytical oral assessments and evaluation, documentation, identification, resolution of potential problems, development of patient-specific oral hygiene, self-care regimen, and recare schedule, dental hygienists deliver essential education, training, and motivation for their implant patients.23
Conclusion
The demand for the long-term survival of dental implants continues to evolve as patients seek innovative solutions to replace missing teeth. Developments in modern dentistry and oral hygiene, new trends in material science, surgical and fabrication techniques, and innovative technologies are solving some of the most complex oral problems. When adequately executed, 98% of dental implants last a lifetime and offer the best investment of any dental restorations.37
Advanced knowledge and skills elevate the ability of dental hygienists to deliver the best oral care. Implementation of the latest expertise and research findings along with patients’ compliance are key to well-functioning, successful, and long-lasting implant treatments.
References
- American Academy of Implant Dentistry. Types of Implants and Techniques. Available at: aaid-implant.org/what-are-dental-implants/types-of-implants-and-techniques/ Accessed December 14, 2021.
- American College of Prosthodontists. Facts and Figures. Available at: gotoapro.org/facts-figures. Accessed December 14, 2021.
- National Institute of Dental and Craniofacial Research. Tooth Loss in Seniors. Available at: nidcr.nih.gov/research/data-statistics/tooth-loss/seniors. Accessed December 14, 2021.
- Saghiri MA, Freag P, Fakhrzadeh A, et al. Current technology for identifying dental implants: a narrative review. Bull Natl Res Cent. 2021;45:7.
- Mazda J. Know your implant options: Understanding the implications of various strategies help inform optimal treatment plans. Inside Dental Techology. 2021;12(3):6–11.
- Galvis OD. A plethora of options for Implants: everyday abutment selection and bar designs. Inside Dent Tech. 2020;11:38–41.
- Terracciano-Mortilla L. Advanced dental implant care concepts 1 assessment. Available at: youtu.be/aUS_xr4ir8s. Accessed December 14, 2021.
- Cionca N, Hashim D, Mombelli A. Zirconia dental implants: where are we now, and where are we heading? Periodontol 2000. 2017;73:241–258.
- Petrungaro, P., S. Implant Esthetics in an Immediate Restoration Protocol: Incorporating a one-piece ceramic implant design to manage compromised soft tissue volume and quality. Inside Dentistry. 2021;17(6):28–29.
- Kendall C. Dental implant surface treatments: what you need to know. Available at: nobelbiocare.com/blog/news/dental-implant-surface-treatments-what-you-need-to-know/. Accessed December 15, 2021.
- Zeynep O, Ender K. Zirconia dental implants: a literature review. J Oral Impl. 2011;37:367–376.
- Wang G, Li J, Lv K, et al. Surface thermal oxidation on titanium implants to enhance osteogenic activity and in vivo osseointegration. Sci Rep. 2016;6:31769.
- Birdi B, Barrie A, Ouriques F, Chay C. Innovations in Implantology: Advances in surfaces, perio-prosthetic platforms, digital workflow, and materials from the single molar to the full arch. Inside Dentistry. 2021;17(6):18–26.
- Gold-Anodizing Titanium Abutments. Available at: obriendentallab.com/videos/?wchannelid=jz9lql9gw9&wmediaid=e8vf0ql6jh. Accessed December 15, 2021.
- Archibald J. The timeless art of troubleshooting: why is your zirconia breaking? Inside Dental Technology. 2020;11(5):30–34.
- Implant designs and treatments. Inside Dentistry. 2021;17(6):38.
- Šimůnek A., Kopecká D, Strnad J. Alkali treatment: new concept of titanium implant surface modification. Clin Oral Impl Res. 2004;15:4.
- Tranquillo E, Bollino F. Surface modifications for implants lifetime extension: an overview of sol-gel coatings. Coatings. 2020;10(6):589.
- Barfeie A, Wilson J, Rees J. Implant surface characteristics and their effect on osseointegration. Brit Dent J. 2015;218:E9.
- Bullis G, Shah S. Implant surface treatments: a literature review. Available at: glidewelldental.com/education/inclusive-dental-implant-magazine/volume-5-issue-2/implant-surface-treatments-a-literature-review/. Accessed December 15, 2021.
- Pirc M, Dragan IF. The key points of maintenance therapy for dental implants: a literature review. Compendium Cont Edu Dent. 2017;38:e5–e8.
- Froum SJ, Rosen PS, Wang H. Why do implants fail? Compendium Cont Edu Dent. 2017;38:360–364.
- Terracciano-Mortilla L. Advanced dental implant care concepts part 2 maintenance. Available at: youtu.be/Xyf-X3lk1xQ. Accessed December 15, 2021.
- Lineberry J. Implant crown restorations: considerations for deciding between cement- and screw-retained options. Inside Dental Technology. 2020;11(3):24–30.
- Renvert S, Hirooka H, Polyzois I, Kelekis-Cholakis A, Wang H. Diagnosis and non-surgical treatment of peri-implant diseases and maintenance care of patients with dental implants—consensus report of working group 3. Intern Dent J. 2019;69:12–17.
- Oral Hygiene for Implants: Oral Hygiene Challenges. Dimensions of Dental Hygiene. Available at: dimensionsofdentalhygiene.com/oral-hygiene-implants. Accessed December 15, 2021.
- Gulati M, Govila V, Anand V, Anand B. Implant maintenance: a clinical update. Int Sch Res Not. 2014;908534.
- Louropoulou A, Slot DE, Barendregt DS, van der Weijdent FA. Prevention and treatment of peri-implant diseases: current evidence on cleaning of titanium dental implant surfaces. Int Journal of Evidence-Based Practice for Dental Hygienists. 2017;3(2):128–141.
- Hatfield S. Implant maintenance: an overview. Available at rdhmag.com/patient-care/implant-maintenance/article/14073139/implant-maintenance-getting-past-the-fear. Accessed December 15, 2021.
- Suzuki JB, Terracciano-Mortilla LD, Misch CE. Maintenance of Dental Implants. Available at: pocketdentistry.com/34-maintenance-of-dental-implants. December 15, 2021.
- Van Witzenburg M. Implant maintenance: getting past the fear. Available at: rdhmag.com/patient-care/implant-maintenance/article/14073139/implant-maintenance-getting-past-the-fear. Accessed December 15, 2021.
- Hasturk H, Nguyen DH, Sherzai H, et al. Comparison of the impact of scaler material composition on polished titanium implant abutment surfaces. J Dent Hyg. 2013;87:200–211.
- Wingrove S. Long-term prevention of peri-implant complications: assessment, maintenance and home-care protocols. Available at: straumann.com/en/discover/youtooth/article/preventive/2021/susan-wingrove-long-term-prevention-peri-implant-complications-assessment-maintenance-home-care-protocols.html. Accessed December 15, 2021.
- Najafi-Abrandabadi S, Quader RO. Classification and selection criteria for dental ceramics. Inside Dental Technology. 2021;12(4):16.
- Wingrove S. What about ceramic implants? Available at: img1.wsimg.com/blobby/go/e1bdb267-2b47-421f-828c-9270a3991a05/downloads/Susan%20Wingrove%20%20Pages%20from %20DDHK%20MagLayout%202-2-.pdf. Accessed December 15, 2021.
- Dimensions of Dental Hygiene. Oral Hygiene for Implants: Importance of Self-Care. Available at: dimensionsofdentalhygiene.com/oral-hygiene-implants. Accessed December 15, 2021.
- Kois Center. What Are Dental Implants? Available at: koiscenter.com/patient-education/bite-and-jaw-health/dental-implants/. Accessed December 15, 2021.
From Dimensions of Dental Hygiene. January 2022;20(1):34-37.



