MCBWORLD/ISTOCK/GETTY IMAGES PLUS
MCBWORLD/ISTOCK/GETTY IMAGES PLUS
The Link Between Orofacial Myofunctional Disorder and Obstructive Sleep Apnea
Strategies for recognizing and managing sleep apnea in the dental setting.
This course was published in the January 2022 issue and expires January 2025. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the link between orofacial myofunctional disorder and obstructive sleep apnea (OSA).
- Identify the dental hygienist’s role in detecting sleep-disordered breathing and OSA.
- List available treatment options for OSA.
Oral health professionals are well positioned to recognize the signs and symptoms of obstructive sleep apnea (OSA) and make the appropriate referrals for medical consultation. The high frequency of prophylaxis appointments makes the dental office the perfect setting to conduct OSA screenings. Dental hygienists, however, often lack enough knowledge about OSA to deliver such screening with confidence.1
Sleep-disordered breathing (SDB) is a dysfunction of the upper airway that occurs during sleep due to increased upper airway resistance and weakened oropharyngeal musculature.2 OSA is characterized by repetitive episodes of upper airway occlusion during sleep,3 which decrease blood oxygen levels and cause fragmented sleep.4 OSA affects both adults and children, and occurs in 15% to 25% of middle-aged and older adults.5 Approximately 70% to 90% of cases remain undiagnosed.5
During sleep, repetitive episodes of total or partial upper airway collapse lead to decreased oxygen levels or hypoxia, which negatively impacts mental and systemic health.6 The effects of hypoxia—which include inflammation, oxidative stress, and increased sympathetic nervous system activity—may be associated with serious comorbidities, such as heart disease, hypertension, type 2 diabetes, Alzheimer disease, and dementia.7 The physiological changes resulting from impaired breathing may also cause low mood; increased automobile, home, and work-related accidents; abnormal dentition development; and even premature death.8–10
The root cause of OSA often stems from improper jaw growth and facial development during childhood.11 Adenotonsillar hypertrophy is a common cause of OSA, particularly in children, however, other anatomical factors may be involved.2 Nocturnal breathing disorders, such as OSA and snoring, impact the developing dental arches. Individuals with SDB and OSA often present with a narrow maxilla, deep palatal height, short mandibular arch, and high prevalence of lateral crossbites.12 Emerging research shows orofacial structures as the predisposing factor involved in the development of SDB; therefore, the relationship between normal breathing and normal orofacial growth is now receiving recognition in the field of sleep medicine.13
Obstructive Sleep Apnea and Orofacial Myofunctional Disorder
Sleep-disordered breathing is an umbrella term that encompasses several sleep-related breathing disorders, including OSA. SDB is caused by an increase in the resistance of the upper airway and pharyngeal collapse, and is characterized by snoring and greater respiratory effort.2
OSA is a sleep disorder that occurs when breathing is interrupted during sleep because the upper airway becomes obstructed repeatedly by the soft palate, base of the tongue, and/or musculature collapse, reducing or completely stopping airflow.4 During sleep, individuals may experience apnea, which is when breathing stops entirely, or hypopnea, which is when breathing is abnormally slow or shallow. Risk factors for developing OSA include a large neck circumference,7 large tonsils, large tongue or uvula, recessed chin, overbite, obesity, improper oral rest posture, and smoking or alcohol use.5
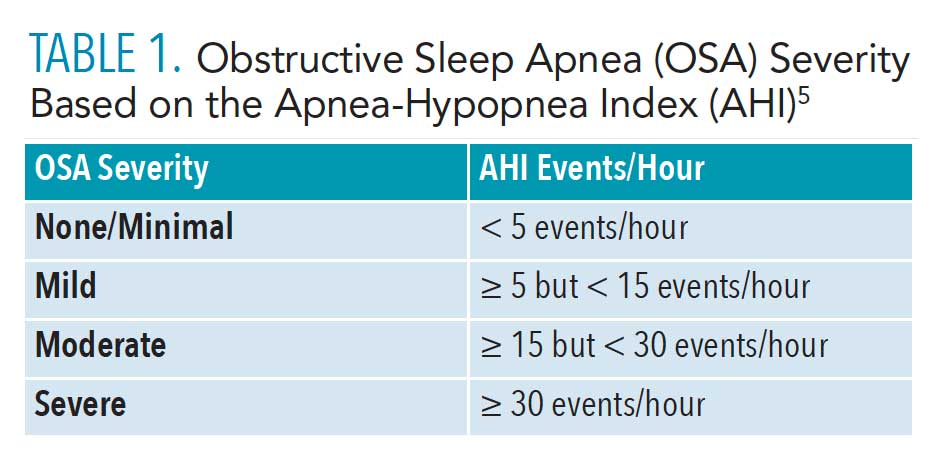
Sleep apnea is diagnosed using a polysomnogram (PSG), a formal sleep study that detects abnormal levels of activity in the muscles that control breathing. PSG also monitors blood oxygen levels and brain and heart activity during sleep.10 OSA severity is measured using the Apnea-Hypopnea Index (AHI), indicating the number of times that breathing stops, or slows, during sleep and is expressed as the number of events per hour (Table 1).5
Orofacial myofunctional disorders (OMD) are commonly seen in patients with OSA. A dysfunction of the stomatognathic system, OMD results in alterations to the appearance, posture, and mobility of the lips, tongue, mandible, and cheeks.14,15
Oral dysfunction may begin at birth, and often becomes apparent as speech develops and solid foods are introduced. This dysfunction may affect facial skeletal growth and development, mastication, speech, occlusion, stability of orthodontic treatment, facial esthetics, and upper airway function.16 OMD may lead to abnormal facial development and malocclusion if timely intervention does not occur.14
Most OMDs originate with insufficient nasal breathing as the muscles and orofacial functions adapt to a disordered breathing pattern.14 Those with collapsed airways during sleep often change their body position or head posture, or the position of their tongue and/or mandible in order to breathe. Long-term postural changes impact the developing dental arches because of the positional changes of the head, mandible, and tongue caused by an insufficient airway.12 Those with SDB commonly breathe through their mouth and have a forward head posture in an effort to open the airway. Mouth breathing alters oral rest posture, increasing nasal resistance, causing tongue malposition, exacerbating impaired development, and hampering the growth of the maxilla and mandible.2 Mouth breathing during sleep causes changes in the muscular balance between the tongue and cheeks, leading to a narrow maxillary arch. Increased lip pressure occurs from the low tongue position and forward head posture, leading to a shorter length of the mandible and mandibular crowding.12
![TABLE 1. Obstructive Sleep Apnea (OSA) Severity Based on the Apnea-Hypopnea Index (AHI)]() Importance of Proper Oral Rest Posture
Importance of Proper Oral Rest Posture
Oral rest posture is where the teeth, lips, and tongue lie when a patient is in a neutral resting position. In proper oral rest posture, the distance between the maxillary and mandibular teeth at rest should be 2 mm to 3 mm in the posterior and 2 mm to 5 mm in the anterior, the lips should gently touch, and the apex of the tongue should rest just lingual to the maxillary anterior teeth, on the incisive papilla.17 This posture encourages nasal breathing and allows the lips to act as an outward muscular force on the teeth. Upon swallowing, the tongue has a modelling role on the oral cavity, stimulating intermaxillary synchondrosis, leading to normal orofacial growth and development. Although the maxilla fuses in utero, it continues to grow during childhood, with only about 80% of skull and jaw growth completed by age 6,17 therefore, a low or forward tongue posture, especially in early childhood, can cause a high-vaulted palate, open bite, or posterior cross bites. A low tongue posture can also cause the outward facial appearance to change, resulting in a narrower, longer forehead and nose, closer set eyes, flattened cheekbones, and a recessed chin.17
Poor oral habits, such as prolonged thumb sucking, pacifier use, or tongue thrust, can also cause the tongue to rest in a low position. In children older than 3, non-nutritive sucking habits may cause permanent damage.18 Sucking habits cause a high, narrow palatal vault because the buccal muscular forces are normal, but the tongue is not reciprocating those forces. When the tongue is thrust forward against the teeth when swallowing, a low tongue posture is usually present as well.
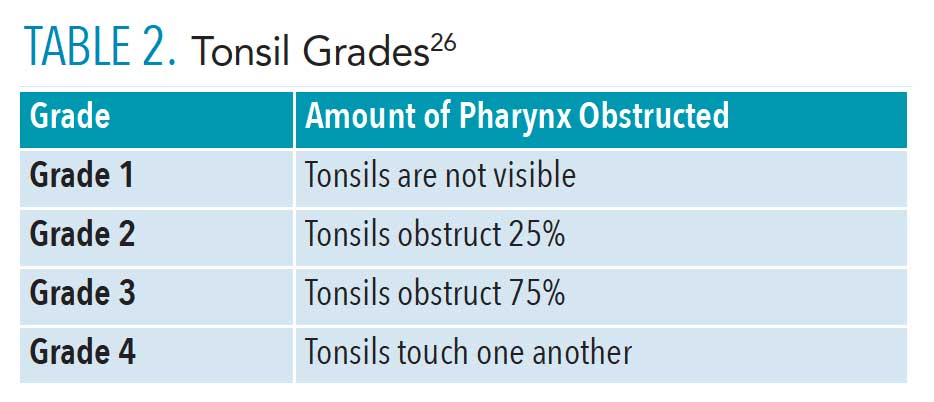
![TABLE 2. Tonsil Grades]() Role of the Dental Hygienist
Role of the Dental Hygienist
Due to the amount of time that dental hygienists spend with patients and the frequency of prophylaxis appointments, the dental office is an ideal setting to conduct OSA screenings.1 Most dental hygienists routinely perform extra/intraoral examinations during dental hygiene appointments, although the current emphasis of this procedure is usually on oral cancer detection. Evaluating the oral cavity for anatomical variations indicative of OSA is a practical addition to this routine assessment. Standardized OSA screenings can be easily incorporated into clinical practice.1
Dental hygienists can screen for OSA by identifying associated comorbid conditions, recognizing craniofacial and oral risk factors, using OSA-related health questionnaires, and referring patients to their primary care physicians as indicated. Additionally, dental hygienists can provide support and education to patients with OSA by discussing behavior modifications, such as tobacco cessation and nutritional counseling.5 Only a physician can legally diagnose OSA, but dental hygienists can promote awareness, recognize and screen for signs and symptoms, and make referrals to appropriate medical professionals for a definitive diagnosis.4 Research shows that how well an individual breathes, both during the day and at night, significantly impacts craniofacial, neurological, and airway development.12
Dental hygienists should conduct an airway screening on every patient, and should include:
Patient history. Medical history review may provide evidence of OSA symptoms, such as medication use, attention deficit hyperactivity disorder, frequent ear infections, throat infection, hypertension, cardiac incidents, or depression.4 Patients who are overweight are more likely to have OSA, especially if there is excess fat stored around the neck and waist.19 Questions such as “Do you snore at night?” or “Do you stop breathing for short periods during sleep?” should be asked. Additional questions include whether the patient is restless during sleep, difficult to rouse in the morning, or, for pediatric patients, if behavior issues are present.4
Questionnaires. The Epworth Sleepiness Scale, which assesses daytime sleepiness, can be integrated into the screening process.20 Additional tools used to identify OSA risk include the STOP (snoring history, tired during the day, observed stopped breathing during sleep, high blood pressure); STOP-BANG (snoring history, tired during the day, observed stopped breathing during sleep, high blood pressure, body mass index more than 35 kg/m2, age older than 50, neck circumference more than 40 cm and male gender); and BEARS (bedtime, excessive daytime sleepiness, awakening during the night, regularity, and duration of sleep and snoring), which is for children, questionnaires.21–23
Extra/intraoral examination. A forward neck posture is common among patients with SDB because it helps to open the airway. Facial changes related to airway issues may include a long face and nose, close set eyes, flattened cheekbones, and venous pooling under the eyes. Additionally, dental hygienists can look for signs of sleep deprivation or mouth breathing.19 Areas of the mouth that can provide evidence of SDB include the tissues, teeth, tongue, throat, and tonsils. The teeth may show signs of occlusal wear from bruxism; caries on the anterior teeth due to mouth breathing; and a high, narrow maxillary arch, class II malocclusion, or deep overbite. A crowded dentition may also be evident with linguoverted teeth, and/or crossbites.24 The tissues may show evidence of mouth breathing by appearing inflamed and erythematous.
Periodontal conditions are also common in patients with SDB. The underlying mechanism explaining this association is not clear, nor is the direction of the association. Periodontitis may reflect an inflammatory burden that results in a robust host response to bacterial plaques among those with OSA. As with other cardiovascular and metabolic diseases, both OSA and periodontitis pathophysiology involve oxidative stress, chronic inflammation, and elevated C-reactive protein levels.25
The size, placement, and movement of the tongue should be evaluated. Macroglossia and a scalloped tongue are indicators for OSA, mostly in adults. Ankyloglossia is also a common finding, as it prevents the tongue from pressing into and shaping the maxilla, resulting in a high vaulted palate.17 The tonsils may be enlarged, and frequent throat infections may be reported. Tonsils vary in size and are classified accordingly (Table 2).26 The pharynx should be evaluated for signs of irritation. The tonsillar pillars may appear red and edematous from snoring or recurrent infections.
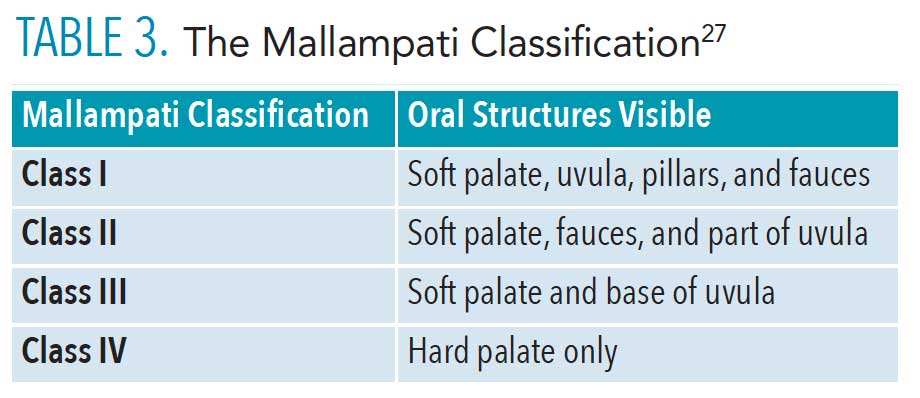
The Mallampati Classification can be used to evaluate the size and anatomy of the airway, using visual inspection to evaluate the distance from the base of the tongue to the soft palate, and to classify the opening of the airway based on what oral structures are visible (Table 3).27 Mallampati class is assessed with the head in full extension, the mouth wide open and the tongue extruded with the patient in an upright position with and without phonation.28 Patients with a class III and IV Mallampati may be more prone to airway obstruction.27 When evaluating the pharynx, those with a restricted airway may display common airway protective reflexes such as making a “gnn” sound as opposed to an “ahh” sound when depressing the tongue or pushing the tongue against the dental mirror.27
![TABLE 3. The Mallampati Classification]() Treatment of Obstructive Sleep Apnea
Treatment of Obstructive Sleep Apnea
Integrating sleep medicine and dental sleep medicine improves patient care, reduces treatment costs, and improves physician education. An integrated, multidisciplinary approach to OSA management is the most effective.29 Several treatment options are available to manage OSA.The most common and effective is continuous positive airway pressure (CPAP). CPAP devices use positive airflow to keep the airway open during sleep, allowing for sufficient oxygen intake. Patient compliance with CPAP machines may be low because the device is cumbersome, and many patients find its use uncomfortable during sleep.4
Dentist-fabricated oral appliances, such as mandibular advancement and tongue-retaining devices, are designed to open the upper airway. They prevent occlusion of the airway by holding the mandible and tongue in a forward position. Oral appliances are most effective for patients in the AHI range of 5 to 30 (mild-moderate).4 Sleep testing should be completed prior to fabrication. Not every patient is a good candidate for an oral appliance; therefore, a thorough examination of the temporomandibular joint, bony structures, gingiva, and teeth is required.4
Myofunctional therapy (MFT) is a noninvasive treatment option that uses an interdisciplinary approach. MFT works with the orofacial muscles and their related functions, such as breathing, sucking, chewing, swallowing, and speech, and can improve facial esthetics and improve the airway.30 Myofunctional therapists work collaboratively with other health professionals to treat both OMD and OSA. When initiated early, myofunctional therapy can prevent the evolution of improper development, restore correct stomatognathic function and nasal breathing, and re-establish tongue position. It can be used with other treatments to avoid residual OSA. Dental hygienists can learn to perform MFT.30
Additional treatment options include lifestyle changes and surgery. Increasing physical activity and weight loss reduce the risk of OSA. Smoking cessation and eliminating or reducing alcohol consumption also decreases OSA risk. Surgical procedures that remove the soft tissues in the posterior pharynx can expand the size of the airway.4
Conclusion
Implementing an interprofessional approach will help optimize treatment for SDB and OSA. The most common referrals for these disorders are a physician, ear nose and throat specialist, sleep specialist, orthodontist, and myofunctional therapist.2 Dental hygienists can be trained to identify physical, behavioral, and birth history clues that can lead to diagnosis and proper intervention.4 Unhealthy sleep patterns negatively impact performance in all aspects of development and education, therefore, dental hygienists should routinely screen for airway disorders. Dental hygienists can serve as the first line of defense for those vulnerable to sleep disruption. As such, incorporating a screening protocol that uses a comprehensive, whole-body approach is appropriate.
References
- Reibel Y, Pusalavidyasagar S, Flynn P. Obstructive sleep apnea knowledge: attitudes and screening practices of Minnesota dental hygienists. J Dent Hyg. 2019;93:29–36.
- Villa MP, Evangelisti M, Martella S, Barreto M, Del Pozzo M. Can myofunctional therapy increase tongue tone and reduce symptoms in children with sleep-disordered breathing? Sleep Breath. 2017;21:1025–1032.
- Guimarães KC, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filho G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2009;179:962–966.
- Agarwal T, Shahidi H. Treating obstructive sleep apnea in the dental setting: clinical and practice management considerations. Dental Academy of Continuing Education. 2018;1-10.
- An SL, Ranson C. Obstructive sleep apnea for the dental hygienist: overview and parameters for interprofessional practice. Canadian Journal of Dental Hygiene. 2011;45(4):238–252.
- Rohra AK, Demko CA, Hans MG, Rosen C, Palomo JM. Sleep disordered breathing in children seeking orthodontic care. Am J Orthod Dentofacial Orthop. 2018;154:65–71.
- Hakes H. Sleep apnea: a growing health concern hygienists need to know about. Available at: todaysrdh.com/sleep-apnea-a-growing-health-concern-hygienists-need-to-know-about/. Accessed December 20, 2021.
- American College of Cardiology. Sleep apnea and high blood pressure a dangerous pair. Available at: cardiosmart.org/news/2015/5/sleep-apnea-and-high-blood-pressure-a-dangerous-pair. Accessed December 20, 2021.
- Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–1014.
- Maspero C, Giannini L, Galbiatti G, Rosso G, Farronato G. Obstructive sleep apnea syndrome: a literature review. Minerva Stomatol. 2015;64:97–109.
- Hodge M. Obstructive sleep apnea: how lifetime care can change everything. Available at: dentaleconomics.com/science-tech/article/16391716/obstructive-sleep-apnea-how-lifetime-care-can-change-everything. Accessed December 20, 2021.
- Pirila-Parkkinen K, Pirttiniemi P, Nieminen P, Tolonen U, Pelttari U, Lopponen H. Dental arch morphology in children with sleep-disordered breathing. Eur J Orthod. 2009;31:160–167.
- Guilleminault C, Sullivan SS. Towards restoration of continuous nasal breathing as the ultimate treatment goal in pediatric obstructive sleep apnea. Available at: semanticscholar.org/paper/Towards-Restoration-of-Continuous-Nasal-Breathing-Dm-Guilleminault/405bc102b4f26bd93124f7f7dd27706e80b8e24f. Accessed December 20, 2021.
- Folha GA, Valera FCP, Felício CMD. Validity and reliability of a protocol of orofacial myofunctional evaluation for patients with obstructive sleep apnea. Eur J Oral Sci. 2015;123:165–172.
- Andrade RAD, Cunha MDD, Da Costa Dos Santos Reis A. Morphofunctional analysis of the stomatognathic system in conventional complete dentures users from the Integrated Health Center. Revista CEFAC. 2017;19:712–725.
- D’onofrio L. Oral dysfunction as a cause of malocclusion. Orthod Craniofac Res. 2019;22(S1):43–48.
- D’Urso N. Muscle memory: a review of tongue muscles and its functions and dysfunctions. Dental Academy of Continuing Education. 2018;1–10.
- Wilkins, EM. Clinical Practice of the Dental Hygienist. 13th ed. Philadelphia: Lippincott Williams & Wilkins; 2021.
- Bewley B. The role of the dental hygienist in screening for sleep apnea. J Dent Hyg. 2014; 88:5.
- Fabbie P. Myofunctional analysis and its role in dental assessments and oral health. Available at: dentalacademyofce.com/courses/2925/PDF/1508cei_Fabbie_WEB.pdf. Accessed December 20, 2021.
- Kornegay E, Brame J. Obstructive sleep apnea and the role of dental hygienists. J Dent Hyg. 2015;89:286–292.
- Pavarangkul T, Jungtrakul T, Chaobangprom P, et al. The STOP-BANG questionnaire as a screening tool for obstructive sleep apnea induced hypertension in Asian population. Neurol Int. 2016;8:6104.
- Ebrahim A, Babak G, Alimohammad A, Shabnam J, Alireza A, Forough F. High prevalence of sleep problems in school- and preschool-aged children in tehran: a population based study. Iran J Pediatr. 2013;23:45–52.
- Schroeder K, Gurenlian JR. Recognizing poor sleep quality factors during oral health evaluations. Clin Med Res. 2019;17:20–28.
- Billings ME. Putting some teeth into it: connecting periodontitis with sleep apnea. Sleep. 2015;38(8):1153–1154.
- Cahali MB, Soares CF, Dantas DA, Formigoni GG. Tonsil volume, tonsil grade and obstructive sleep apnea: Is there any meaningful correlation? Clinics. 2011;66:1347–1352.
- Kandray D, Juruaz D, Yacovone M, Chang A. Inter-rater reliability of the mallampati classification for patients in a dental hygiene clinic. J Dent Hyg. 2013;87:134–139.
- Khan ZH, Eskandari S, Yekaninejad MS. A comparison of the Mallampati test in supine and upright positions with and without phonation in predicting difficult laryngoscopy and intubation: a prospective study. J Anaesthesiol Clin Pharmacol. 2015;31:207.
- Nakai T, Matsuo A, Takata Y, Usui Y, Kitamura K. Chikazu D. Role of dental sleep medicine in management of patients with obstructive sleep apnea disorders using a team approach. Acta Odontologica Scandinavica. 2018;76: 605–611.
- Academy of Orofacial Myofunctional Therapy. What is Myofunctional Therapy? Available at : aomtinfo.org/myofunctional-therapy/. Accessed December 20, 2021.
From Dimensions of Dental Hygiene. January 2022;20(1):38-41.