 LAYLABIRD/E+/GETTY IMAGES PLUS
LAYLABIRD/E+/GETTY IMAGES PLUS
Strategies for Treating Tongue Tie
A multidisciplinary approach to treating ankyloglossia may potentially improve function and quality of life for affected patients.
This course was published in the July 2021 issue and expires July 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain ankyloglossia, associated issues, and the benefits of and need for collaborative, multidisciplinary care for this patient population.
- Describe the dentist’s role in treating patients with ankyloglossia.
- Discuss strategies to resolve potential conflicts among the extended, multidisciplinary care team when treating patients with ankyloglossia.
Ankyloglossia, more commonly referred to as tongue tie, is a congenital condition in which a neonate is born with an abnormally short, thickened, or tight frenum that hinders mobility of the tongue.1 Considering these patients may present in the dental clinic at various stages of life, knowledge of this condition will help oral health professionals provide collaborative and appropriate care. Understandably, ankyloglossia can pose many challenges throughout the lifespan, such as latch/breastfeeding issues during infancy; feeding issues as the infant transitions to textured foods (including mastication of solids); speech issues; and functional/social issues (eg, orthodontic problems or sleep apnea).
Certain conditions at birth, no matter how minor, may evolve into more significant conditions later in life. These may be preventable through early intervention. For example, stressors prenatally or at delivery—such as amniotic fluid levels, fetus malpositions, birth processes necessitating forceps, vacuum, or suction, and intravenous fluids—can influence latch/breastfeeding response.2 Tensions and force during the birth process can affect the head/neck muscles and bones that exacerbate a preexisting ankyloglossia, causing asymmetries and even cranial nerve effects.
Understanding, evaluating, and treating ankyloglossia may improve function and quality of life for these patients throughout the lifespan. Oral health professionals can help achieve these goals as part of a multidisciplinary team. As such, they need to be aware of the vital roles played by members of the extended care team at various stages of the patient’s development.
BENEFITS OF MULTIDISCIPLINARY CARE
While early intervention may reduce the need for treatment over time and prevent longer treatment periods at later stages of development, at any point in this process therapy may be needed from providers with specific disciplinary expertise—each viewing conditions through a professional lens within his or her scope of practice. For example, a myofunctional therapist or lactation consultant can perform a functional assessment to determine the need for a release procedure. If indicated, an otolaryngologist or a properly trained dentist (or other release provider) can perform the surgery, while a speech-language pathologist assists with aftercare and subsequent oral motor rehabilitation. The team may include other providers with skills that are age-specific to the patient’s needs.
A lactation consultant, for example, has expertise in latch and breastfeeding and might be a stronger team member when working with infants. In another case, a difficult family environment may dictate the services of a social worker/psychologist. Post-partum depression may reduce rates of breastfeeding; similarly, not engaging in breastfeeding may increase the risk of post-partum depression. The bidirectional nature can influence the latch/breastfeeding outcome.3 This example illustrates the need for collaborative care, because ignoring the mother’s post-partum depression and correcting the child’s ankyloglossia will not produce an optimal outcome.
Awareness of the different lenses through which each healthcare discipline views a particular situation can provide a more comprehensive understanding of issues that one practitioner alone may not see. By making proper referrals or facilitating the procedure, each lens of the multidisciplinary team can help illuminate a comprehensive diagnosis and treatment plan that targets the source of the issue, not just the overt symptom.
Diagnosis and multidisciplinary care are active processes, with collaboration and sharing of information critical to determining when, and if, a procedure is necessary. Throughout this process, there is a unified need to understand each provider’s discipline and areas that may (or may not) overlap. Teams that collaborate contribute to stronger and more successful outcomes, as well as more effective decision-making.4
One barrier to collaboration is perceived conflict that may arise when examining a patient from various disciplinary lenses. Conflict can become difficult to overcome if a clear solution does not present itself, the conflict is managed poorly, or if personality differences prohibit objective discussion.5 Managing emotions and personal feelings is essential to reach consensus.6 However, conflict can be effectively managed by separating the issue from the people making the decision, focusing attention on shared interests and desired outcomes, generating multiple solutions to discuss and evaluate, and basing decisions on established objective criteria.7
MULTIDISCIPLINARY TEAM MEMBERS
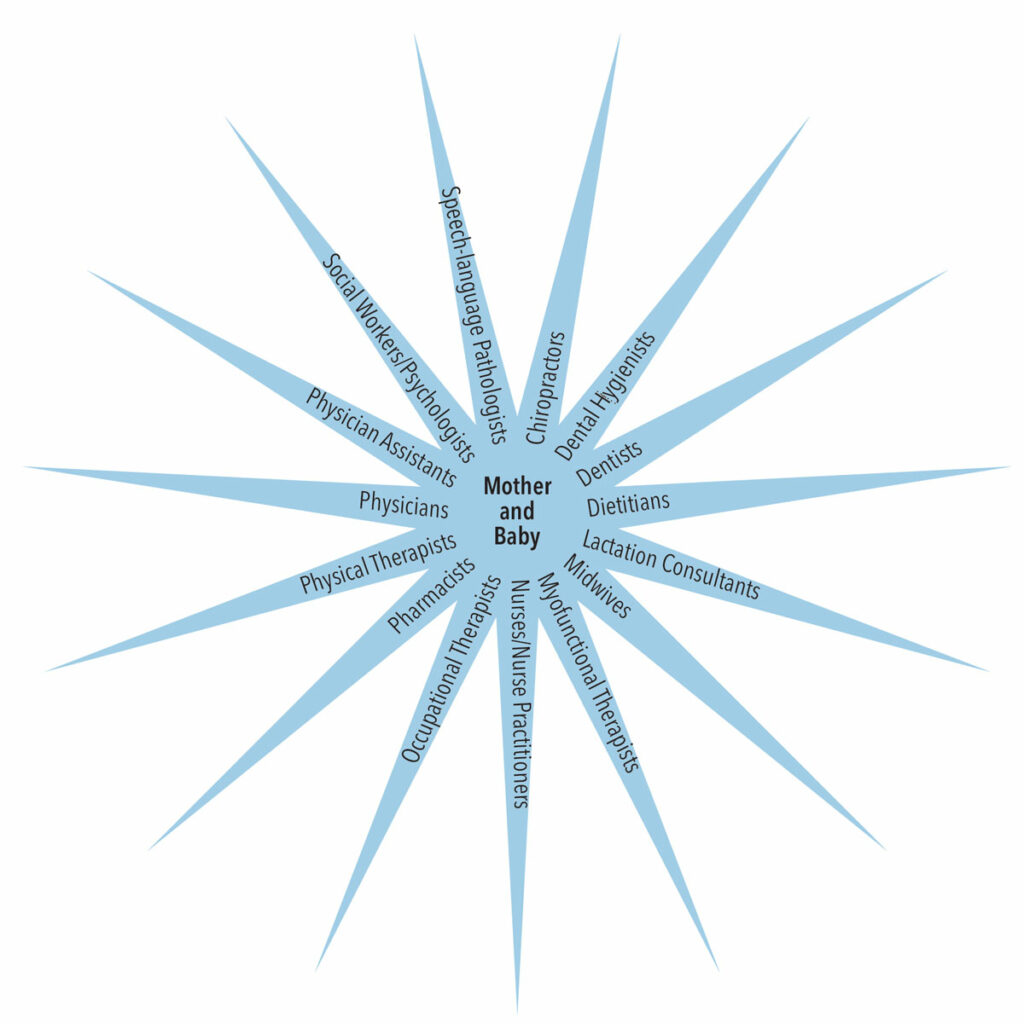
Creating a multidisciplinary team may involve some or all of the following providers (not wholly inclusive): chiropractors, dentists, dietitians, lactation consultants, midwives, myofunctional therapists, nurses/nurse practitioners, occupational therapists, pharmacists, physical therapists, physicians, physician assistants, social workers/psychologists, and speech-language pathologists (Figure 1).
Establishing any and all necessary connections is critical to the proper and timely resolution of any ankyloglossia issues. This requires multiple viewpoints to assess comprehensively, rather than reaching a conclusion based on limited observation from one perspective. From the patient’s infancy though adulthood, team members will change based on the patient’s age, history, and symptoms.
For example, assuming there is a morphological problem when the patient has full functional capability, or missing a morphological problem when the patient has obvious functional issues, are equally incorrect. Assessment of a frenum by visual evaluation alone (morphology) and not by assessing the patient’s ability of elevation, lateralization, extension, cupping and peristalsis, or questioning activities such as speech, sleep or eating issues, ignores the functional capabilities.
Clinicians should also consider that compensatory efforts may camouflage the patient’s capabilities. Assuming the issue is solely with the infant when the mother has issues might also be an erroneous conclusion. A mother may comment that her baby has ankyloglossia because she is unable to breastfeed. Upon further questioning and evaluation, the mother reveals she has a reduced milk supply, inverted nipples, previous breast surgery, or Raynaud phenomenon. In such cases, collaborative care is critical to correct the mother’s difficulties.
An infant with underlying neuromuscular issues likely will not benefit to the fullest extent from a tongue tie release alone, as this infant has never had the chance for the nerves and muscles to work correctly. Releasing the tongue may be just one step in the process. It is prudent to have pretherapeutic and postsurgical interventions.8,9 A mother with a history of hypothyroidism, diabetes, or nutritional issues presents with a radically different set of circumstances than a mother who has an overabundant milk supply. Similarly, breastfeeding difficulties may be magnified if the milk supply is inadequate, even if the infant only has slight ankyloglossia.
In older children and adults, a dentist may be able to identify ankyloglossia and have the skills to release the tie, but the decision to release requires a more comprehensive investigation. Other professionals can perform functional assessments that can provide the dentist (or other release provider) with evidence the release is necessary. After the procedure is complete, multidisciplinary team members can provide appropriate aftercare and strengthening exercises to prevent reattachment and accomplish functional goals.
Because multidisciplinary collaborative efforts are complex, each team member can provide insights that contribute to positive outcomes. Specifically:
Chiropractors may help in the diagnosis and treatment of mechanical disorders of the musculoskeletal system, especially the spine. These disorders might have an impact on the cranial nerves that enervate the tongue and orofacial muscles. Many infants with ankyloglossia also have torticollis contributing to latch/breastfeeding difficulty.10,11
Dental hygienists are the first oral health professionals to perform an oral assessment, which includes an evaluation of the tongue. They are well suited to note the physical characteristics of ankyloglossia. Dental hygienists also interface frequently with parents/caregivers of toddlers and infants, which may provide insight into possible oral abnormalities such as ankyloglossia.
Dentists have expertise in the oral cavity and tongue, and are familiar with the orofacial muscles and functional movements. Clinicians who are trained in tethered oral tissues and release procedures can perform the tongue tie release that may be necessary.11 Periodontists are often called upon when the tethered tissue causes periodontal problems in young adults and adults. This is often seen as recession, diastemas, and tethered-tissue-influenced malocclusions. Orthodontists are needed when there is an early indication of constricted palates that might need expansion and growth tendencies indicative of ankyloglossia. Sleep apnea may be associated with ankyloglossia. Pediatric dentists are often the first to evaluate infants during the predentate years and may discover tethered issues. Oral surgeons are frequently used to address problems associated with oral tethered tissues and other soft and hard tissue problems.
Dietitians help ensure proper nutritional status of the mother/child dyad. Mother/child allergies, sensitivities, or even specific diets need proper guidance by the dietitian to optimize the health of the dyad; for example, the mother needs extra calories to continue lactogenesis.2
Lactation consultants are instrumental during infancy. There can be many reasons other than tongue tie why a baby is not breastfeeding well, and lactation consultants can identify the situation and create a comprehensive plan that may or may not include surgery. If surgery is necessary, the lactation consultant can make further technique adjustments, help the baby with sucking exercises to improve latch and position technique, and retrain the baby from the bottle back to the breast.8
Midwives are important in helping mothers during labor and delivery and after birth. Long and difficult labor can impact mother’s milk supply or influence the infant’s parasympathetic/sympathetic nervous system response.12
Myofunctional therapists work on the reeducation or normalization of craniofacial structures and function. The goal is to facilitate alterations until breathing, sucking, chewing, swallowing, and speech are improved.13,14 Dental hygienists are highly qualified to become myofunctional therapy practitioners after appropriate training.
Nurses in the delivery area and neonatal intensive care unit are some of the first to interact with baby and mother. They are often able to detect issues related to ankyloglossia.12
Occupational therapists can analyze a level of activity or task that is suboptimal and develop a plan to improve performance. But surgery alone does not guarantee performance of the activity; for example, infants often have difficulty in the transition from breast milk or formula to textured foods and solids.12,15
Pharmacists, in concert with physicians, can affect the pre- and post-natal pharmacologic needs of the dyad.
Physical therapists use exercises, hands-on therapy, and equipment to help patients increase mobility and function and facilitate normalization. This can be helpful before and after a release surgery. Significant muscle tension can be alleviated through physical therapy.1
Physicians of various disciplines are the gatekeepers of patient information. They can provide timely input on the infant’s genetic predisposition for ankyloglossia. For example, patients with certain syndromes—such as Smith-Lemli-Opitz, oral-facial-digital, cleft palate or Van der Woude—have a higher incidence of ankyloglossia. The presence of a midline defect constellation should also be considered if there are other issues. Problems with submucous cleft palate and laryngomalacia can also be present with ankyloglossia.
Physician assistants are licensed to diagnose and treat illness and disease and prescribe medications. Many large clinics and remote areas utilize physician assistants who may assist patients with ankyloglossia.
Social workers/psychologists can assist with post-partum depression that could magnify any discomfort at the breast. Mothers with the highest rates of post-partum depression are often the ones who intended to breastfeed, but end up not being able to do so. Dysphoric milk ejection also has been associated with an inability to breastfeed. Social workers/psychologists can help a mother’s feeling about motherhood and her relationship to her newborn.16
Speech-language pathologists work to prevent, assess, diagnose, and treat speech, language, social communication, cognitive communication, and swallowing disorders. Management, intervention, and treatment can be a synergistic benefit with any potential surgical release.11
As various providers work with these patients to resolve issues at different life stages, it becomes clear that coordinated care is not fractionated, disconnected care, but a seamless unity of relationships. That said, these multidisciplinary collaborative efforts are challenged by a lack of standardized protocols.14
BUILDING PROFESSIONAL RELATIONSHIPS
It is advantageous to cultivate relationships among professional colleagues and understand how the dyad can benefit from multidisciplinary collaborative efforts. For example, the infant can benefit from an uncomplicated transition to textured foods and solids.17,18 The young child can benefit from the maturation phases of the phonological processes involved with speech acquisition and speech intelligibility. The adult can benefit from not being challenged by functional/social issues that could otherwise hinder positive peer relationships and acceptance within social and professional circles.
When caring for patients with ankyloglossia, oral health professionals are advised to work with other members of the patient’s extended care team during treatment planning and therapy. Collecting all the information needed to establish a diagnosis, and assessing the historical data, present data, and patient concerns can provide a more complete perspective on the patient’s needs and care. For instance, malocclusion and periodontal issues often reflect the presence of ankyloglossia. Additionally, details about the mother’s health history can provide information about the breastfeeding/latch relationship with the infant. The baby’s transition to textured foods and solids, and subsequent speech acquisition and intelligibility represent developmental steps that could benefit from collaborative care. Similarly, sleep habits and related tendencies provide clues for potential sleep apnea and airway difficulties that may require multidisciplinary treatment.
If a dentist is performing the tongue tie release surgery, the clinician should document color changes of the healing wound (white/yellow/light pink/coral pink) and be mindful of the need for active wound management to prevent readhesion. The classic diamond shape of the wound should be described. Collaborating professionals should understand the difference between primary and secondary intention healing, and the importance of stretches and massages in active wound management.19–21 Post-surgical follow-up instructions should include dietary restrictions and recommendations, oral hygiene measures, pain management options, and potential guidance regarding bleeding.
While in-office post-surgical evaluation is ideal, intraoral photos communicated by a cell phone can provide much-needed positive or negative feedback to patients concerned about their wound management and healing progression. A word of caution, however: patients or parents/caregivers will tend to view or report healing progress with an optimistic filter because they are not anxious to undergo a second (ie, repeat) surgery. Rather than relying on a subjective impression, in-person evaluation provides a more realistic clinical view.
SUMMARY
Ankyloglossia can affect many areas of health, function, and development throughout the patient’s lifespan. Thus, it is important for professionals across multiple disciplines to collaborate when caring for these patients. Optimal outcomes are achieved when this condition is assessed and treated comprehensively from structural and functional perspectives.
Ultimately, the time, support, and empathy provided to these patients contribute to positive results. Additionally, these efforts help build multidisciplinary relationships that will improve care for other cases that would benefit from collaborative treatment. As Kluender22 notes, “There is no better time than now to cultivate a comprehensive and efficient team approach to care.”
REFERENCES
- Francis D, Chinnaadurai S, Morad A, et al. Treatments for ankyloglossia and ankyloglossia with concomitant lip-tie. U.S. Agency for Healthcare Research and Quality. Available at: https://www. ncbi.nlm.nih.gov/books/NBK299120/. Accessed June 11, 2021.
- Campbell SH, Lauwers J, Mannel R, Spencer B. Core Curriculum for Interdisciplinary Lactation Care. Burlington, Mass: Jones & Bartlett Learning; 2018.
- Pope CJ, Mazmanian D. Breastfeeding and postpartum depression: an overview and methodological recommendations for future research. Depress Res Treat. 2016;2016:4765310.
- Sinclair AL. The effects of justice and cooperation on team effective-ness. Small Group Research. 2003;34:74–100.
- Cramer D. Linking conflict management behaviours and relational satisfaction: The intervening role of conflict outcome satisfaction. J Soc Pers Relat. 2002;19:425–432.
- Wilmot WW, Hocker JL. Interpersonal Conflict. 10th ed. New York, NY: McGraw Hill; 2018.
- Fisher R, Ury W, Patton B. Getting to Yes. New York, NY: Random House; 1999.
- Hazelbaker AK. Tongue-Tie — Morphogenesis, Impact, Assessment and Treatment. Columbus, Ohio: Aidan and Eva Press; 2010:183.
- Mohrbacher N. Breastfeeding Answers Made Simple. Plano, Texas: Hale Publishing; 2010:727–769.
- Hawk C, Minkalis A, Webb, C, Hogan O, Vallone S. Manual interventions for musculoskeletal factors in infants with suboptimal breastfeeding: a scoping review. J Evid Based Integr Med. 2018;23:1–14.
- Baxter DM. Tongue-Tied. Pelham, Ala: Alabama Tongue-Tie Center; 2018.
- Amir LH, Kelso G, Moorhead AM. Accreditation of midwife lactation consultants to perform infant tongue tie release. Int J Nurs Prac. 2011;17:541–547.
- Kotlow L. SOS 4 TOTS. New York, NY: Troy Book Makers; 2016.
- Boop C, Smith J. The Practice of Occupational Therapy in Feeding, Eating and Swallowing. Available at: https://ajot.aota.org/article.aspx?articleid=2652875. Accessed June 11, 2021.
- Hamaguchi P. Childhood Speech, Language, and Listening Problems. 3rd ed. Hoboken, NJ: John Wiley and Sons; 2010.
- Hurst CG, Reno R, Lefmann T. Committing to breastfeeding in social work. Social Work. 2018;63:252–260.
- Newman J. Breastfeeding Empowering Parents. North York, Ontario: International Breastfeeding Centre; 2018:182–197.
- Lauwers J, Swisher A. Counseling the Nursing Mother. 6th ed. Boston, Mass: Bartlett Learning; 2015.
- Suter VG, Bornstein MM. Ankyloglossia: facts and myths in diagnosis and treatment. J Periodontol. 2009;80:1204–1219.
- Tecco S, Baldini A, Mummolo S, et al. Frenulectomy of the tongue and the influence of rehabilitation exercises on the sEMG activity of masticatory muscles. J Electromyogr Kinesiol. 2015;25:619–628.
- Tsaousoglou P, Topouzelis N, Vouros I, Sculean A. Diagnosis and treatment of ankyglossia: A narrative review and a report of three cases. Quintessence Int. 2016;47:523–534.
- Kluender R. Collaborative leadership in multidisciplinary treatment. Decisions in Dentistry. 2021;7(5)10–11.
From Dimensions of Dental Hygiene. July 2021;19(7):36-39.



