 MARK KOSTICH/ISTOCK/GETTY IMAGES PLUS
MARK KOSTICH/ISTOCK/GETTY IMAGES PLUS
Addressing Xerostomia in Patients Undergoing Treatment For Head and Neck Cancer
Educating patients on protective oral measures can help this patient population maintain their oral health and reduce the negative effects of cancer therapy.
This course was published in the July 2021 issue and expires July 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe the prevalence of cancers of the oral cavity and pharynx.
- Discuss the effects of radiation on salivary gland function and how these impact caries risk.
- Identify strategies for helping this patient population maintain their oral health.
Cancers of the oral cavity and pharynx are on the rise, with more than 50,000 cases diagnosed in 2020.1 While the prevalence of these cancers declined in the 1980s due to a decrease in tobacco and alcohol use, the rate of oral cavity and pharynx cancers began to rise in 1999.2 Between 2007 and 2016, oral and pharyngeal cancers increased by approximately 0.6% annually.2 This rapid increase appears to be due to pharyngeal cancers linked to human papillomavirus (HPV) infections located at the base of the tongue, tonsils, soft palate, uvula, and pharyngeal walls. Cancers linked to HPV have been increasing by 2.1% annually, whereas cancers unrelated to HPV have been decreasing by 0.4% annually.3 Cancerous lesions of the oral cavity not associated with HPV are typically located on the lip, floor of the mouth, hard palate, and nasopharynx. The majority of these malignancies require intervention with surgery, radiotherapy, chemotherapy, or a combination of these; however, all of these treatments can cause significant morbidity to the oral cavity. With the increased incidence of oral and pharyngeal cancers and the detrimental effects caused by treatment of these cancers on the oral cavity, the oral healthcare team needs to be prepared to help these patients maintain their oral health.
EFFECTS OF RADIATION ON SALIVARY GLAND FUNCTION
The role of saliva in optimal oral health is multifactorial. It lubricates the mucosal membranes, promotes the buffering capacity and remineralization process, and provides an antimicrobial effect. Patients who undergo head and neck radiotherapy often experience radiation-induced damage to the salivary glands.3,4 This is due to the proximity of the salivary glands to these head and neck tumors. In many cases, the radiation must pass through various salivary glands to effectively treat the tumor, and, in some cases, the tumor exists within the salivary gland itself. Salivary glands are extremely sensitive to even low doses of radiation, resulting in a reduction of saliva flow and alteration of the saliva composition.4 The severity of the salivary changes depends on the dose of radiation therapy administered to the gland.5
During radiation therapy, patients often experience a decrease in production and increased viscosity of their saliva.6 This may be temporary for some patients while others may experience a permanent loss of salivary production as a result of radiation therapy. While exploring changes in the salivary gland function of patients with head and neck cancer after radiation therapy, Lin et al7 found a dramatic decrease in salivary flow during the first month following radiotherapy, with some recovery occurring between the third month and sixth month post-treatment; however, pretreatment flow levels were not often fully achievable. Salivary flow and dental caries are closely related. Decreased flow and increased thickness allows for impaired bacterial clearance from tooth surfaces and an increased caries rate.8

Radiation therapy also affects the composition of saliva, reducing its buffering capacity. Saliva has a normal pH range of 6.5 to 7.5. Enamel is susceptible to demineralization when the pH of the oral cavity is 5.5 or below.3 With the limited amount of saliva combined with decreased buffering capacity, the dentin and enamel are more easily demineralized.4 The influence of radiation therapy on the pH of the oral cavity may linger, with the pH beginning to increase back to normal levels 1-year post radiation therapy.7 Thus, patients with head and neck cancer are more prone to an increase in demineralization after radiotherapy, especially within the first year following radiation therapy.
Reflective of the change in the pH of the oral cavity, acidogenic and cariogenic microorganisms also begin to flourish. From the onset of radiation therapy, more cariogenic bacteria, such as Streptococcus mutans, Lactobacillus, and Candida, are identified in the oral cavity.4 The combination of decreased salivary flow, lowered pH of the oral cavity, and increased cariogenic bacteria significantly increases this population’s risk for dental caries.9 P
XEROSTOMIA-INDUCED DENTAL CARIES
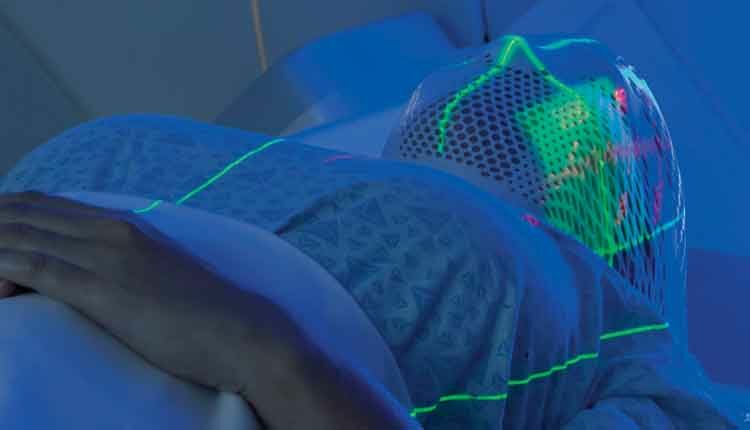
Xerostomia is defined as a dry mouth resulting from reduced or absent salivary flow. Dry mouth can affect speech, taste sensation, and ability to swallow, in addition to increasing the incidence of dental caries.4,10 This deeply impacts quality of life and affects a large percentage of people previously treated for head and neck cancer.11–13 The severity of xerostomia depends on the cumulative dose of ionizing radiation to the major salivary glands (Figure 1).14 Reduction in salivary flow can be observed with ionizing radiation doses as low as 30 Gy.5,15,16 Severe salivary dysfunction is observed at doses of 52 Gy ionizing radiation or greater.13 Head and neck tumors are typically treated at doses of 60 Gy to 70 Gy, which causes a rapid decline in salivary function. Xerostomia can be experienced as early as the first week of radiotherapy, with a 95% reduction in salivary flow experienced by the fifth week.12,13 Salivary dysfunction may be temporary or permanent.11
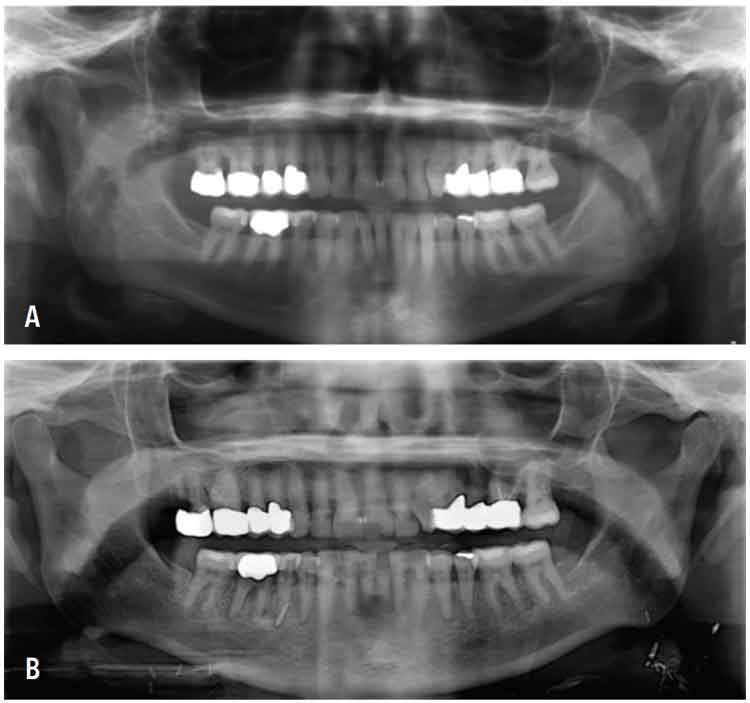
Radiation-induced dental caries can be extremely destructive and often progresses rapidly (Figure 2A and Figure 2B). Clinically, radiation caries present in three different patterns.4 The most common affects the cervical aspect of the teeth, extends into the cementoenamel junction, and creates circumferential decay. The second pattern begins as demineralization on any tooth surface and rapidly progresses. The third pattern, while less common, presents as a darkened color on the teeth. Ultimately, the goal of managing post radiation caries is prevention, and, in this, the dental hygienist plays a critical role.
ORAL HEALTH GUIDELINES
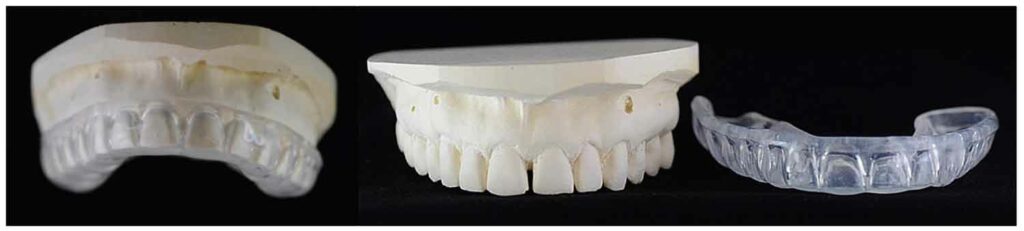
Due to the sequelae of head and neck radiation therapy, this patient population is at increased risk for oral complications and should be monitored closely by their oral healthcare team. Radiation therapy reduces salivary flow and composition, which may cause teeth to rapidly decay if not properly protected. Fabrication of custom fluoride trays is recommended (Figure 3). Patients are instructed to apply prescription-strength fluoride gel (eg, 5,000 ppm) into these trays daily and follow the manufacturer’s instructions for use.17
While radiation-induced xerostomia can improve over time, it rarely resolves completely. As such, these patients should continue to use their fluoride trays daily as long as xerostomia persists. In addition, these oral sequelae place this patient population in the “high” to “extreme” caries risk level according to caries management by risk assessment (CAMBRA) protocol. Therefore, fluoride varnish should be applied at each dental hygiene visit post-radiation therapy.9 Dental hygienists support patients’ self-care by recommending over-the-counter fluoride toothpaste and/or dentifrice with calcium phosphate in addition to fluoride. Not only does fluoride inhibit demineralization and promote remineralization, but in high concentrations, it can also inhibit bacterial plaque growth.18
Dental hygienists are critical members of the oral healthcare team for patients with head and neck cancer, assisting in the management of radiation-induced xerostomia, suggesting prevention strategies to reduce cariogenic activity, and identifying early changes to tooth structures or radiation caries. Increased examination frequency on a 3-month basis is suggested to monitor caries risk and development.9,18 This interval is recommended until the cariogenic activity is stabilized, after which a 6-month interval is indicated.19 Depending on the individual’s caries risk assessment, capturing bitewings/periapical radiographs every 6 months to 12 months may be advised.19 Routinely monitoring the oral cavity closely is an optimal prevention strategy for patients with head and neck cancer.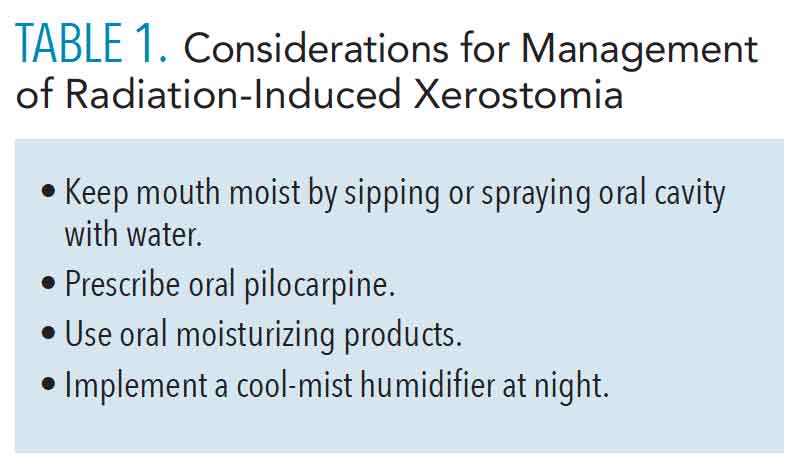
To assist patients in the management of radiation-induced xerostomia, sugar-free gum, lozenges, and oral melts containing xylitol are recommended to help to stimulate saliva production and decrease oral bacterial load (Table 1).13 Oral mucosal lubricants, sprays, and mouth rinses are also available to moisten the oral cavity; however, they typically provide a short duration of dry-mouth relief.6 If dry mouth symptoms cannot be effectively addressed with over-the-counter regimens, a prescription of pilocarpine or other cholinergic agonist may be helpful.6 If extreme xerostomia continues to persist, a referral to a dentist or physician with expertise in the management of salivary disfunction may be warranted. Due to the saliva’s reduction in buffering capacity, patients may want to rinse with a solution of ½ teaspoon baking soda (and/or ¼ teaspoon to ½ teaspoon of table salt) in 1 cup of warm water several times daily.20 Frequent cleaning, lubricating, and buffering the oral cavity will help minimize the effects of radiation-induced xerostomia.
Diet may also influence cariogenic activity of the oral cavity in patients with head and neck cancer. Xerostomia affects food preferences, appetite, and dietary intake; xerostomia is a key factor associated with weight loss after radiation therapy.21 Patients are advised to eat small, high-calorie meals multiple times a day as well as consistent sipping of water. Dental hygienists should suggest prevention strategies to reduce cariogenic activity such as avoiding foods with high sugar content and rinsing with water after eating. In addition, due to the decrease in salivary function, dry and salty foods such as breads and crackers should be avoided (Table 2). Properly managing xerostomia may ultimately improve the nutritional status patients with head and neck cancer, too. 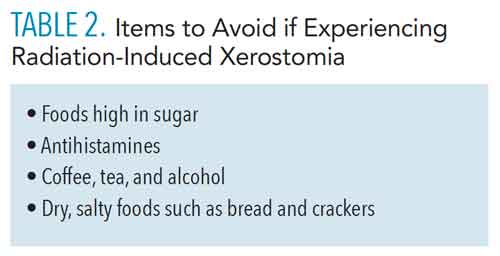
CONCLUSION
To maintain optimal oral health in patients with head and neck cancer, a multidisciplinary care team is required before, during, and after cancer treatment. The dental hygienist plays a significant role on this team. Radiation therapy leads to changes in salivary quantity and quality, ultimately placing this patient population at high risk for xerostomia-induced dental caries. Routine bacterial plaque control, use of products to stimulate salivary flow, use of products that act as a salivary replacement, and daily use of custom fluoride trays with prescription-strength fluoride gel can improve the overall quality of life for these patients.
REFERENCES
- American Cancer Society Cancer Statistics Center. 2021 Estimates. Available at: cancerstatisticscenter. cancer.org/#!/. Accessed June 28, 2021.
- Ellington TD, Henley SJ, Senkomago V, et al. Trends in incidence of cancers of the oral cavity and pharynx—United States 2007–2016. MMWR Morb Mortal Wkly Rep. 2020;69:433–438.
- Deng J, Jackson L, Epstein JB, Migliorati CA, Murphy BA. Dental demineralization and caries in patients with head and neck cancer. Oral Oncol. 2015;51:824–831.
- Gupta N, Pal M, Rawat S, et al. Radiation-induced dental caries, prevention and treatment : a systematic review. Natl J Maxillofac Surg. 2015;6:160–166.
- Braam PM, Terhaard CH, Roesink JM, Raaijmakers CP. Intensity-modulated radiotherapy significantly reduces xerostomia compared with conventional radiotherapy. Int J Radiat Oncol Biol Phys. 2006;66:975–980.
- Shiboski CH, Hodgson TA, Ship JA, Schiødt M. Management of salivary hypofunction during and after radiotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(Suppl 66):e61–79.
- Lin CY, Ju SS, Chia JS, Chang CH, Chang CW, Chen MH. Effects of radiotherapy on salivary gland function in patients with head and neck cancers. Journal of Dental Sciences. 2015;10(3):253–262.
- Dodds MWJ, Johnson DA, Yeh CK. Health benefits of saliva: a review. J Dent. 2005;33:223–233.
- Rechmann P, Kinsel R, Featherstone JDB. Integrating caries management by risk assessment (CAMBRA) and prevention strategies into the contemporary dental practice. Compend Contin Educ Dent. 2018;39:226–233.
- Jawad H, Hodson NA, Nixon PJ. A review of dental treatment of head and neck cancer patients, before, during and after radiotherapy: part 1. Br Dent J. 2015;218:65–68.
- Nyathi M. Ionizing radiation side effects on salivary glands post external beam radiationtherapy of head and neck tumors. Journal of Biology and Medical Research. 2018;2(4):1:4.12.
- Cheng SC, Wu VW, Kwong DL, Ying MT. Assessment of post-radiotherapy salivary glands. Br J Radiol. 2011;84:393–402.
- Porter SR, Scully C, Hegarty AM. An update of the etiology and management of xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:28–46.
- Jensen SB, Pedersen AM, Vissink A, et al. A systematic review of salivary gland hypofunction and xerostomia induced by cancer therapies: prevalence, severity and impact on quality of life. Support Care Cancer. 2010;18:1039–1060.
- Pinna R, Campus G, Cumbo E, Mura I, Milia E. Xerostomia induced by radiotherapy: an overview of the physiopathology, clinical evidence, and management of the oral damage. Ther Clin Risk Manag. 2015;11:171–188.
- Wu VWC, Leung KY. A review on the assessment of radiation induced salivary gland damage after radiotherapy. Front Oncol. 2019;9:1090.
- Epstein JB, Chin EA, Jacobson JJ, Rishiraj B, Le N. The relationships among fluoride, cariogenic oral flora, and salivary flow rate during radiation therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:286–292.
- Featherstone JDB, Chaffee BW. The evidence for caries management by risk assessment (CAMBRA®). Adv Dent Res. 2018;29:9–14.
- Noone J, Barclay C. Head and neck cancer patients – information for the general dental practitioner. Dent Update. 2017;44:209–210, 213–205.
- Kawashita Y, Soutome S, Umeda M, Saito T. Oral management strategies for radiotherapy of head and neck cancer. Jpn Dent Sci Rev. 2020;56:62–67.
- Nuchit S, Lam-Ubol A, Paemuang W, et al. Alleviation of dry mouth by saliva substitutes improved swallowing ability and clinical nutritional status of post-radiotherapy head and neck cancer patients: a randomized controlled trial. Support Care Cancer. 2020;28:2817–2828.
From Dimensions of Dental Hygiene. July 2021;19(7):40-43.



