 WAVEBREAKMEDIA / ISTOCK/GETTY IMAGES PLUS
WAVEBREAKMEDIA / ISTOCK/GETTY IMAGES PLUS
The Safe Use of Radiography in Children
Pediatric patients are more vulnerable to the effects of radiation, so clinicians must be prudent when capturing radiographs in this population.
Because ionizing radiation can cause biological health risks, oral health professionals must be knowledgeable about radiation safety standards.1,2 While the discussion regarding radiation exposure risk is often focused on the medical field, there is ongoing concern regarding possible health hazards posed by low-dose dental radiographs, as they may be prescribed more frequently than medical images. The As Low As Reasonably Achievable (ALARA) radiation safety principle is important for oral health professionals to adopt—and is even more essential when treating pediatric patients because radiation exposure poses a significant risk to developing organs and tissues.3 While radiographs are critical to diagnosing dental disease and for assessing growth and development in pediatric patients, children’s tissues may be at greater risk of ionizing radiation due to their small size, which puts them closer to the primary beam of radiation. In addition, children usually require a decrease in the exposure settings to produce quality radiographic images because their bone structure is not as dense as adults.4
Campaigns focused on reducing children’s radiation exposure have been developed. In 2007, the Alliance for Radiation Safety in Pediatric Imaging started the global Image Gently® campaign to focus on advocacy to improve safe and effective imaging of children.5 Image Gently provides health professionals and patients with education about radiation safety for children. Organizations such as the American Dental Association (ADA), American Dental Hygienists’ Association (ADHA), and the American Academy of Pediatric Dentistry (AAPD) support and promote the Image Gently campaign.1,5
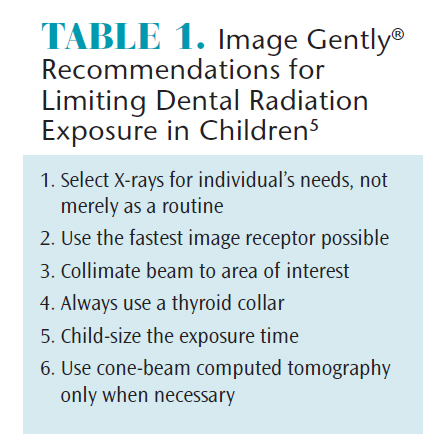
The goal of Image Gently is to promote special considerations for pediatric dental radiography and eliminate unnecessary exposures in children. As such, the campaign utilizes a simple six-step system to increase radiation safety for children (Table 1) and introduces the term, As Low As Diagnostically Achievable (ALADA).5 In recent years, the use of cone-beam computed tomography (CBCT), or three-dimensional imaging, has increased in dental practices. In many cases, CBCT images are being prescribed more frequently than is necessary, which has led to the need for the ALADA principle.5 Oral health professionals can take a pledge on the Image Gently website and print a certificate to display in support of radiation safety guidelines.
RADIOGRAPHIC SELECTION GUIDELINES
Dental hygienists can make preliminary assessments and recommendations for necessary radiographs based on comprehensive clinical examinations and medical and dental histories.4 Evidence-based selection guidelines should be utilized when making decisions about the type, frequency, and quantity of dental radiographs to be taken for adults, adolescents, and children. Revised in 2012 by the ADA, United States Food and Drug Administration, and several dental specialty organizations, the Dental Radiographic Examinations: Recommendations for Patient Selection and Limiting Radiation Exposure should be used when prescribing dental radiographs and when they serve as an aid to limit the number of radiographic exposures. Selection guidelines are incorporated after a complete medical history and thorough clinical examination are conducted.6For children, radiographic frequency depends on several factors, including dentition status, caries risk, and assessment of growth and development.
Dental hygienists can eliminate radiation exposures in children until all primary teeth are fully erupted and inspection of interproximal areas cannot be visualized.4 The only exceptions are if the child has a toothache, presents with growth and development issues, or pathology is suspected.4 After determining what radiographs are diagnostically necessary, dental hygienists should adhere to the ALARA/ALADA principles.2
IMAGE RECEPTOR TYPE
To keep radiation exposure as low as possible in children, oral health professionals should use E- or F-speed film or digital sensors.4,5 While D-speed film is still available, a significant decrease in radiation exposure is seen with faster speed films (E and F) and digital sensors. The degree of image receptor sensitivity determines appropriate exposure setting reductions to produce images with adequate density and contrast necessary for diagnosis. In general, the more sensitive the image receptor to radiation, the less exposure time needed to produce acceptable diagnostic images. Overall, film is the least sensitive receptor to radiation, requiring increased radiation exposure to produce an image. Direct digital sensors based on either charge-coupled device (CCD) or complementary metal oxide semiconductor active pixel sensor (CMOS-APS) technologies are the most sensitive to radiation.7Indirect digital imaging, or photostimulable phosphor plates (PSP) are more comparable to film in regards to degree of sensitivity, but they may be slightly more sensitive than film. Intraoral direct digital sensors allow for maximum decreased radiation exposure compared to both PSPs and film. Direct and indirect digital and film-based extraoral units may not see any difference in radiation exposure reduction compared to intraoral receptors.4 Switching from D speed film to a direct digital sensor may reduce radiation exposure up to 50%, but reductions are less when switching from E or F speed film to digital imaging (PSPs or direct sensors).8 Oral health professionals should use the fastest intraoral image receptor type available. However, it’s also important to decrease exposure factors according to the type of image receptor used.
RECTANGULAR COLLIMATION
Position indication devices (PIDs) are currently manufactured as circular or rectangular; however, external rectangular collimators that attach to circular PIDs are available for increased collimation of the X-ray beam. Restricting an X-ray beam size via collimation limits patients’ radiation exposure. Furthermore, rectangular collimation used in dental radiography decreases exposure by five times when compared with circular collimation.9 Many oral health professionals are reluctant to make the change from circular to rectangular collimation because of concerns about an increased chance of centering (cone-cut) errors and the resultant need for retake exposures. Enhanced collimator and image alignment systems are available that convert a circular PID to a rectangular PID and assist in aligning the image receptor to the PID to avoid cone-cut errors. These systems attach to most intraoral dental X-ray machines and can be used with traditional image receptor positioning devices. Research has demonstrated a decrease in centering errors when using enhanced collimator and image alignment systems; however, 35% more radiation was received compared to only using universal collimator devices without image alignment systems.10 Because the radiation exposure reduction is significant, oral health professionals should incorporate rectangular collimation for all patients, especially children. Oral health professionals will need to weigh error reduction (need for retake exposures) and radiation exposure with enhanced collimation devices compared with universal collimators alone.

EXPOSURE SETTINGS
Less radiation is required for the exposure of dental radiographs in children because tissues and bone structures are less dense when compared to adults.11 In many cases, exposure times should be reduced by one-half of an adult exposure setting for children younger than 10 and by one-fourth for children and adolescents ages 10 to 15.4 Most intraoral and extraoral X-ray machines enable the clinician to preset exposure settings for children and adults (Figure 1). These settings can also be altered to consider the size, density, and dentition of the pediatric patient. The exposure time should also be reduced according to the area being exposed. Anterior images do not need as high exposure factors compared with the posterior region due to the decreased density of teeth and supporting bone in the anterior region.12
THREE-DIMENSIONAL IMAGING
CBCT is becoming more common in dental practices and offers improved diagnosis for certain oral conditions. These images expose patients to greater doses of radiation than traditional two-dimensional dental radiology procedures.4 CBCT exposures should only be used when lower-dose techniques, such as two-dimensional intraoral or extraoral radiographs, are not diagnostically acceptable. For children and adolescents, CBCT is considered the standard of care for orthodontic assessment and may offer a similar radiation dose because several two-dimensional extraoral images are necessary for a complete orthodontic examination compared with images obtained with one CBCT scan.1,4,13 To limit radiation exposure for CBCT images, the field of view should be reduced to the area of interest.
THYROID SHIELDING
The thyroid gland is considered one of the most sensitive tissues to ionizing radiation in children.14,15 Because the thyroid gland is in close proximity to the oral cavity, it is more likely to receive unnecessary exposure to radiation during dental radiographs. Both the ADA and the National Council on Radiation Protection & Measurements recommend thyroid shielding in pediatric patients.15 The use of a lead or lead equivalent thyroid collar can reduce the radiation to this organ significantly for intraoral radiographs and by 50% for CBCT images.16 Lead thyroid collars are contraindicated for use when interference with the exposure is likely, as is the case for extraoral panoramic radiographs and some CBCT images. Therefore, the exposure settings must be kept as low as possible when thyroid shielding is not achievable. To provide maximum protection, clinicians must ensure the thyroid collar is positioned and secured properly. Thyroid collars must completely cover the thyroid gland and be tightly secured around the neck by attaching both ends at the back of the neck and base of the skull. A child-size lead or lead equivalent collar should be used for optimal fit (Figure 2). Ill-fitting thyroid collars will not offer full protection from radiation, making it imperative that lead thyroid collars are correctly sized to the pediatric patient.

IMAGING TECHNIQUES
To limit the amount of exposures, oral health professionals must avoid the need for retakes due to technique error. The same imaging techniques and principles used in adults can be used in pediatric patients, but may require some modifications. Children may have a small oral cavity, low palatal vault, hypersensitive gag reflex, lack of tongue control, and sensitive oral mucosa due to erupting permanent teeth. A smaller image receptor size and modifications to image receptor positioners may be necessary for the pediatric patient. External aiming devices may be too heavy for children. Adapting the image receptor holders may be necessary, such as using a bitewing tab as a periapical image receptor holding device.4 Additionally, vertical angulation may need to be slightly increased to accommodate image receptors in children with a low palatal vault.4
Pediatric radiographic technique is based on clinical assessment and examination of oral structures. If the paralleling technique cannot be tolerated by a child, the bisecting technique can be considered. Though the images may be more distorted, this technique could still produce reasonably acceptable images for diagnosis and treatment. For either technique, the external aiming rings of image receptor positioning devices should be as close to the patient’s skin as possible, and the PID should be close to the external aiming ring to avoid increased radiation exposure to sensitive organs and tissues. The occlusal technique may be implemented when no other techniques can be tolerated.4
Because of varying levels of cooperation, communication is essential when working with pediatric patients. The clinician must confidently describe the procedure to the child so that he or she knows what is expected. This also encourages cooperation to successfully obtain diagnostic images. The “tell-show-do” technique can be successful when communicating with children. In this method, the clinician shows the child the image receptor and positioners while explaining the procedure before taking radiographs. If implementing the modeling technique, the child can also observe radiographs being taken on another patient, such as the parent or sibling.4 These approaches can reduce the risk of retake errors. If the oral health professional cannot obtain cooperation from the child, it may be necessary to postpone the radiographic assessment until a diagnostic image is achievable. Good judgment on pediatric patients’ cooperation levels is required when assessing the need for dental radiographs and the size and number of images.4
CONCLUSION
Prevention of dental disease is of utmost importance during childhood because of increased risk for dental caries and faster disease progression.17 All radiographic examinations should be individualized to patient need. The exposure to dental radiographs must have diagnostic benefits that outweigh the risk of radiation exposure for children. Oral health professionals need to incorporate clinical judgment, the prior medical and dental history of the child, intraoral examinations, and selection guidelines when assessing the need for two- or three-dimensional dental radiographs. Using the fastest image receptor possible, rectangular collimation, decreased exposure settings, thyroid shielding, and technique modifications to reduce radiographic imaging errors will significantly lower the amount of ionizing radiation exposure to children.
REFERENCES
- White SC, Scarfe WC, Schulze RK, et al. The Image Gently in Dentistry campaign: promotion of responsible use of maxillofacial radiology in dentistry for children. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:257–261.
- Bruhn AM, Newcomb TL, Tolle SL. Ensuring safe practice in dental radiology. Dimensions of Dental Hygiene. 2015;13(12):30–33.
- Fogarty WP, Drummond BK, Brosnan MG. The use of radiography in the diagnosis of oral conditions in children and adolescents. N Z Dent J. 2015;111:144–150.
- Thomson EM, Johnson ON. Essentials of Dental Radiography for Dental Assistants and Hygienists. 10th ed. Upper Saddle River, New Jersey: Pearson; 2018.
- The Alliance for Radiation Safety in Pediatric Imaging. Image Gently Campaign. Available at: imagegently.org. Accessed on January 20, 2017.
- American Dental Association and Food and Drug Administration. Dental Radiographic Examinations: Recommendations for Patient Selection and Limiting Radiation Exposure. Available at: fda.gov/downloads/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures/MedicalImaging/MedicalX-Rays/UCM329746.pdf. Accessed January 20, 2017.
- Wenzel A, Moystad A. Work flow with digital intraoral radiography: A systematic review. Acta Odontoloica Scandinavica. 2010;68:106–114.
- United States Food and Drug Administration. Dental Radiography: Doses and Film Speed. Available at: fda.gov/RadiationEmittingProducts/RadiationSafety/ NationwideEvaluationofX-RayTrendsNEXT/ucm116524.htm. Accessed January 20, 2017.
- Ludlow JB, Davies-Ludlow LE, White SC. Patient risk related to common dental radiographic examinations: the impact of 2007 international commission on radiological protection recommendations regarding dose calculation. J Am Dent Assoc. 2008;139:1237–1243.
- Johnson BK, Mauriello SM, Ludlow JB, Platin EP. Technical performance of universal and enhanced intraoral imaging rectangular collimators. J Dent Hyg. 2015;89:238–246.
- Chugh T, Jain AK, Jaiswal RK, Mehrotra P, Mehrotra R. Bone density and its importance in orthodontics. J Oral Biol Craniofac Res. 2013;3:92–97.
- Rondon RHN, Pereira YCL, do Nascimento GC. Common positioning errors in panoramic radiography: A review. Imaging Sci Dent. 2014;44:1–6.
- Miles DA, Danforth RA. A Clinician’s Guide to Understanding Cone Beam Volumetric Imaging (CBVI). Tulsa, Oklahoma: Academy of Dental Therapeutics and Stomatology; 2008:1–15.
- Sinnott B, Ron E, Schneider AB. Exposing the thyroid to radiation: a review of its current extent, risks, and implications. Endocr Rev. 2010;31:756–773.
- National Council on Radiation Protection and Measurements. Radiation Protection in Dentistry. Available at: ncrppublications.org/reports/145. Accessed January 20, 2017.
- Qu XM, Li G, Sanderink GC, Zhang ZY, Ma XC. Dose reduction of cone beam CT scanning for entire oral and maxillofacial regions with thyroid collars. Dentomaxillofac Radiol. 2012;41:373–378.
- Moynihan P, Petersen PE. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 2004;7:201–226.
From Dimensions of Dental Hygiene. February 2017;15(2):24-27.

