The Safe and Effective Use of Cone-Beam Computed Tomography
This three-dimensional technology offers many advantages but oral health professionals need to be well versed in its indications and technique to use it safely.
This course was published in the September 2019 issue and expires September 2022. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe cone-beam computed tomography technology (CBCT) and how it differs from other dental imaging.
- Describe dental specialties where CBCT imaging is indicated.
- Discuss ways to limit radiation exposure when using CBCT technology.
- Describe advantages and disadvantages of CBCT radiography.
Acquiring high-quality radiographic images is essential to rendering accurate oral diagnosis and treatment. An important advancement in digital radiography is cone-beam computed tomography (CBCT). A radiographic imaging method, CBCT provides accurate, three-dimensional (3-D) imaging of hard tissue structures. CBCT is important to incorporate into specialized dental settings, as it provides a higher standard of care for patients.1 Although two-dimensional (2-D) images have provided diagnostic information in dentistry for many years, they have limitations—such as magnification, distortion, and superimposition of anatomical details—that can lead to misrepresentation of structures.1 As CBCT becomes more commonly used in dentistry, oral health professionals should become familiar with the diagnostic capabilities of this 3-D technology.
CBCT was introduced in Europe in the late 1990s and approved in the United States by the federal Food and Drug Administration (FDA) in 2001.2 Its use in dental settings has grown rapidly over the past two decades, with 11% annual growth expected.2 By 2023, the CBCT market is estimated to reach $960.8 million globally and $360 million in the US.3,4
CBCT continues to advance due to research, developments made by manufacturers, and high demand from dentists who see clear advantages of incorporating this technology into their practices.4 Previously, if 3D imaging was indicated, a CT or magnetic resonance imaging (MRI) was necessary at a medical facility, but with the inception of CBCT, this imaging can be accomplished within the dental practice.5
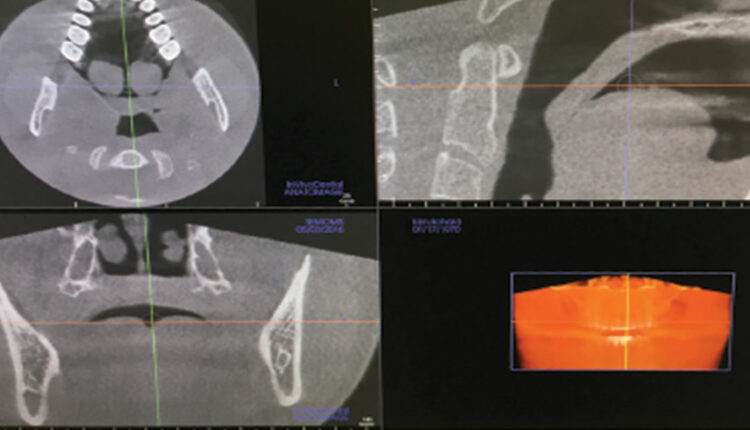
CBCT can be divided into two categories: fan-beam and cone-beam scanners. In fan-beam scanners, the patient is imaged slice by slice, and the system software reconstructs the data from slices into a stacked image to create 2D representations, such as a panoramic radiograph.6 In contrast, a cone-shaped X-ray beam and a 2D sensor that rotates 180° to 360° around the patient’s head to capture hundreds of “basis images” are reconstructed into tomographic images by a computer. Basis images are exposures taken at fixed intervals during the rotation of the cone beam scanner. During the reconstruction phase, the computer software creates 3D images out of the 150 basis images to 600 basis images, reformatting them into axial, sagittal, and coronal orientations (Figure 1).6 CBCT images often provide more detailed information than their 2D counterparts in regards to anatomical structures.1
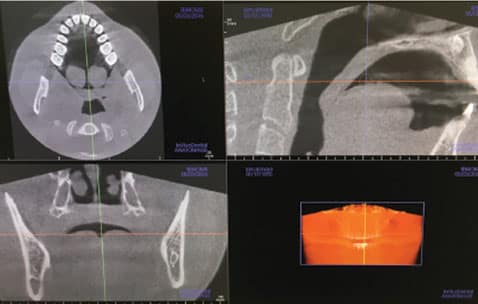
axial, sagittal, and coronal views.
VOXELS, FIELD OF VIEW, AND IMAGE AQUISITION
CBCT imaging has different voxels and field of view (FOV). A pixel is the smallest image in 2D imaging represented by height and width, and a voxel is a volume pixel with width, height, and depth; it adds the third dimension to the image.7 Voxels are represented as a cube or box with sides that are usually 1 mm to 2 mm.5 The smaller the voxel size, the greater the noise, but the higher the spatial resolution. Image quality is dependent on FOV; scan time; number of basis images; and type of detector, tube voltage, and amperage.7 Care should be taken to select the optimal FOV for the diagnostic objective. The width of the FOV can range from 3 cm to 24 cm in height.8 A small, medium, or large FOV can be chosen for the image.
A small FOV scan would be indicated for an area of up to five teeth (approximately 5 cm), such as endodontic procedures. The smaller FOV exposes the patient to a lower dose of radiation, reduces scatter radiation, and increases image clarity. A medium FOV would be indicated for evaluation of one or both arches, scanning 6 cm to 11 cm in height.6 If an image of the temporomandibular joint (TMJ) is needed, a medium FOV should be selected. A large FOV is recommended for imaging of a wide area, such as skeletal anomaly or if orthognathic surgery is planned. The scanned area can range from 11 cm to 24 cm in height and covers most of the craniofacial skeleton.6 The main drawback of the larger FOV is the increase in radiation exposure.

tomography machine in a standing position.
A CBCT scan collects the anatomical data in one rotation, typically in 10 seconds to 40 seconds, and patients can either stand or sit, depending on the unit (Figure 2).9 The quick collection of data reduces the possibility of motion artifacts. The system’s software then reconstructs the collected data to show dimensionally accurate basis images of the scanned area in different planes (Figure 3 and Figure 4). The time needed to build the 3D image ranges from 20 seconds to 6 minutes.6 The software allows manipulation of these images to show different slices at different angles, varying depths and thicknesses, 3D reconstructions, and some soft tissue structures—all without image distortion.
CBCT uses ionizing radiation to penetrate the body tissues, and the digital sensors measure the high- and low-density areas of absorbed X-rays, creating a picture on the computer screen. Structures with the highest density are materials made out of metal, followed by enamel and bone.6 High-density objects diminish the X-ray beam, resulting in a reduction in the number of X-ray photons that strike the detector or sensor. High-density structures display as white or light in the image, while low-density structures that do not diminish the X-ray beam, such as air, display as black or dark.6

tomography imaging of a frontal view of maxillary and
mandibular arches.

APPLICATIONS
CBCT images can assist in treatment planning for a variety of dental specialties, including oral and maxillofacial surgery, orthodontics, endodontics, and periodontics. Research also discusses case-specific use of CBCT imaging for TMJ evaluation and airway analyses for obstructive sleep apnea.1,3,4 Research continues to support and validate the use of CBCT imaging in dental implant placement.4,10,11 CBCT imaging is commonly used for evaluation of root morphology, location of relevant anatomic structures and their relation to implant placement, sinus grafting for pre-implant evaluation, and post-bone augmentation implant planning.12 CBCT imaging provides accurate information on nerves, canals, sinuses, bone height, width, and structure. Software enhancements allow clinicians to virtually place implants and prostheses. It provides greater accuracy in measuring bone compared to 2D imaging and reduces the possibility of malpositioned implants. CBCT imaging also provides a reduction in implant failures by providing precise information regarding bone density, shape of alveolus, and the height and width of the proposed implant site.1
CBCT has many applications in oral surgery.1,13 Images provide the position of impacted teeth, roots, and surrounding structures, and skeletal asymmetries.13 They are useful in the diagnosis of cysts, tumors, fibro-osseous lesions, and paranasal sinuses. Images also provide the exact location and extent of jaw pathologies, pre- and post-surgical assessment of bone grafting, facial and orbital fractures, and planning for orthognathic surgery.1
CBCT imaging is the modality of choice for complex endodontic cases.14 The images are beneficial when diagnosing periapical lesions. Other uses are to diagnose vertical root fractures, detect internal and external root resorption, identify the number and morphology of roots and associated canals.1
Limited research supports the use of CBCT imaging as a routine part of orthodontic treatment; however, it may be useful in some complex malocclusion cases.10,13 Little evidence supports the use of CBCT in periodontics, although it could be indicated for the treatment planning of full-mouth advanced periodontitis cases; periodontal bone defects; implant placement; accurate measurement of intrabony defects; and assessment of dehiscence, fenestrations, and periodontal cysts.1
Some evidence supports the use of CBCT imaging for specific TM disorders.1 It aids in examination of the joint space and the true position of the condyle within the fossa to reveal possible dislocation of the joint. CBCT could be indicated for cases involving trauma, fibro-osseous ankyloses, pain, dysfunction, and condylar vertical erosion and cysts.1 It aids in measurement of the glenoid fossa as well as visualization and location of the soft tissue. However, CBCT does not adequately image the soft tissue so an MRI is recommended for a complete soft tissue evaluation. Additionally, CBCT imaging does not show the position or integrity of the TMJ disk as the disk is not calcified.1 Limited diagnosis of airway conditions is possible with CBCT imaging. It could determine patients with a higher predisposition to obstructive sleep apnea, but a final diagnosis should be done through a medical sleep study.6
RADIATION DOSAGE AND EXPOSURE
One of the greatest benefits of CBCT is that it provides multiplanar imaging with approximately 10 times less radiation compared to a medical CT scan.12 Specifically, typical doses for CBCT imaging of both jaws is 0.068 millisieverts (mSv), 0.6 mSv for a hospital CT scan of both jaws, and 0.08 mSv for a full-mouth series using E-speed film.5 The amount of ionizing radiation will be different according to each CBCT unit, the anatomy being evaluated, and the setting selected to produce a quality image. Radiation dosage is dependent on the FOV, peak kilovoltage, milliamperage, number of basis images, scan time, and degree of rotation.2 Limitation of FOV dimensions of the region of interest can reduce patient radiation dose by up to 82%.14 Smaller voxel sizes are attributed to higher resolution and higher radiation, however, a lower resolution might provide the same diagnostic outcome.15 Shorter scan times resulting in fewer basis images and 180° scans versus 360° scans will also reduce radiation exposure.6,16,17 Although most CBCT scanners are capable of producing a 360° scan, a 180° scan is capable of producing acceptable images.9,17
Oral health professionals need to reduce dosages to a level at which diagnostic quality is not affected.8 In addition, they must adhere to the ALARA (as low as reasonably achievable) principle and exposure guidelines as set forth by the American Dental Association (ADA) and FDA.18 This is achieved through individualized selection of exposures, equipment selection, equipment maintenance, and an ongoing quality assurance program.17 A new concept known as ALADA (as low as diagnostically acceptable) has recently been accepted to stress not only low-dose radiation protocols, but also image quality optimization.17
In order to ensure patient safety, every attempt should be made to reduce radiation, including the use of lead aprons and thyroid collars, especially for children. Professional judgment should be practiced to assure that the lead apron will not be positioned between the X-ray source and the area of interest, which could result in the need to retake images.4,8
GUIDELINES
CBCT imaging should not be used routinely. It is an adjunctive procedure that is recommended for cases in which clinical examination and traditional 2D intraoral and extraoral radiography cannot supply adequate diagnostic information.17 The American Academy of Oral and Maxillofacial Radiology (AAOMR) released best practice guidelines for CBCT usage in 2008.3,19 In an effort to reach further consensus on the clinical indications of CBCT, other professional dental organizations contributed to additional guidelines in recent years to address patient selection criteria specific to each specialty, dose, and diagnostic or treatment needs to help prevent excessive use of this growing technology.4
TRAINING
The safe and effective use of CBCT requires adequate training, continuing education, and expertise to differentiate various maxillofacial structures and pathology of the head and neck.5,6,8 In cases where the entire jaw is imaged or for small nondentoalveolar FOV, the clinical evaluation and report should be made by a specially trained dentomaxillofacial radiologist or medical radiologist.1,17 Telediagnostic tools and software have made it much easier to obtain an opinion from a radiologist if need be.8 Care must be taken to avoid missed pathology that could result in litigation against the practitioner.5
When using a small FOV, it is relatively easy to become disoriented when reviewing and rotating the images.5,8 For example, direction of depth could be accidentally reversed, or the right and left may be transposed. When reviewing images, intraoral radiographs, panoramic radiographs, intraoral photographs, and study casts should be referenced to assure correct orientation.8 New installations of CBCT equipment will require some practice prior to use to assure proper acquisition. This can be done using manikins in a demonstration mode without irradiation to learn different imaging methods, selecting appropriate FOV, positioning, and adjusting exposure dose.8 The dentist will need to practice using the software with demonstration cases in which brightness, contrast, zoom, and section thickness can be manipulated. Rotating the axes, measuring distances, saving images, and interpreting and confirming anatomic structures should also be applied. Lastly, the dentist should practice creating thorough clinical reports.8
ADVANTAGES AND DISADVANTAGES
The main advantage of CBCT technology is the production of 3D images and its ability to create cross-sectional images, improving diagnostic capabilities. The images have increased accuracy, higher resolution, lower radiation, and reduced costs compared with other volumetric imaging.3,6 CBCT imaging enables treatment planning with a higher degree of prediction, as oral health professionals are able to analyze areas of the head and neck without the superimposition or distortion of structures found with 2D imaging.
CBCT imaging provides high-quality, accurate 3D representation of the osseous features of the oral and maxillofacial region, and is superior to conventional 2D images in demonstrating the quantity and quality of bone, in addition to the spatial relationship of an object relative to the adjacent anatomical structures.20 If an office already has a panoramic machine, the unit can be upgraded to one that has both panoramic and CBCT capabilities.
Although CBCT technology offers many advantages, there are also some disadvantages. There is an increased radiation dose over panoramic radiographs and the possibility of artifacts due to scatter radiation, resulting in shading or streaking. Due to the size of these machines, renovations may be needed to the dental office. The initial cost of buying the equipment is high, as well as the time and effort needed to train clinical staff on how to use and interpret the information. The cost of the CBCT machine is approximately $100,000, and although pricing may be slowly decreasing, many dental offices cannot justify the investment of this specialized technology.21 There may be software updates, integration and support costs, and a different system may be needed to store the images. Additionally, it is predominantly a bone-imaging technology and does not significantly differentiate soft tissue structures, such as muscles, glands, and vascular supply.
CONCLUSION
CBCT is an exceptional tool that provides 3D imaging and has become more accessible and increasingly common in dental practices. However, it does not replace standard dental radiographic images and should be used as a complementary tool for specific cases, not for routine cases. When indicated, this advanced technology enables oral health professionals to see all aspects of the head and neck structures in ways never thought possible with 2D radiographs. With a better understanding of 3D technology and how it works, this advancement in radiography provides pertinent diagnostic information to the dental professional, as well as patient education, so the patient may better understand and accept recommended treatment. Future advancements in CBCT digital radiography technology will continue to improve and enhance patient care in the dental office.
REFERENCES
- Alamri HM, Sadrameli M, Alshalhoob MA, Sadrameli M, Alsehri A. Applications of CBCT in dental practice: A review of the literature. Gen Dent. 2012;60:390–400.
- Abramovitch K, Rice DD. Basic principles of cone beam computed tomography. Dent Clin North Am. 2014;58:463–484.
- Rios JF, Borgnakke WS, Benavides R. The use of cone-beam computed tomography in management of patients requiring dental implants: An American Academy of Periodontology best evidence review. J Periodontol. 2017;88:946–959.
- Kim IH, Singer SR, Mupparapu M. Review of cone beam computed tomography guidelines in North America. Quintessence Int. 2019;50:136–145.
- Macleod I, Heath N. Cone-beam computed tomography (CBCT) in dental practice. Dent Update. 2008;35:590–598.
- Scarfe WC, Li Z, Aboelmaaty W, et al. Maxillofacial cone beam computed tomography: essence, elements and steps to interpretation. Aust Dent J. 2012;57:46–60.
- White SC, Pharoah MJ. Oral Radiogology: Principles and Interpretation. St. Louis: Mosby/Elsevier; 2014.
- Hayashi T, Arai Y, Chikui T, et al. Clinical guidelines for dental cone-beam computed tomography. Oral Radiology. 2018;34:89–104.
- Pauwels R, Araki K, Siewerdse JH, Thongvigitmanee SS. Technical aspect of dental CBCT: state of the art. Dentomaxillofac Radiol. 2015;44:20140224.
- Mandelaris GA, Scheyer ET, Evans M, et al. American Academy of Periodontology best evidence consensus statement on selected oral applications for cone-beam computed tomography. J Periodontol. 2017;88:939–934.
- Garlapati K, Babu G, Chaitanya NC, Guduru H, Rembers A, Soni P. Evaluation of preference and purpose of utilisation of cone beam computed tomography (CBCT) compared to orthopantomogram (OPG) by dental practitioners: a cross-sectional study. Pol J Radiol. 2017;80:248–251.
- Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008;52:707–730.
- Li Y, Sun J, Zhang Y, Li W, Hu B, Song J. 3D reconstruction images of cone beam computed tomography in dental medicine application: a case study and mini-review. J Xray Sci Technol. 2016;24:673–680.
- Panmekiate S, Rungwittayathon P, Suptaweeponboon W, Tangtraitham N, Pauwels R. Optimization of exposure parameters in dental cone beam computed tomography using a 3-step approach. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;126:545–552.
- Spin-Neto R, Gotfredsen E, Wenzel A. Impact of voxel size variation on CBCT-based diagnostic outcome in dentistry: a systematic review. J Digit Imaging. 2013;26:813–820.
- Pauwels R, Jacobs R, Bogaerts R, Bosmans H, Panmekiate S. Determinations of size-specific exposure settings in dental CBCT. Eur Radiol. 2017;27:279–285.
- Bornstein M, Horner K, Jacobs R. Use of cone beam computed tomography in implant dentistry: current concepts, indications and limitations for clinical practice and research. Periodontol 2000. 2017;73:51–72.
- American Dental Association and Food and Drug Association. Dental radiographic examinations: recommendations for patient selection and limiting radiation exposure. Available at: fda.gov/media/84818/download. Accessed August 21, 2019.
- Carter L, Farman AG, Geist J, et al. American Academy of Oral and Maxillofacial Radiology executive opinion statement on performing and interpreting diagnostic cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:561–2.
- Adibi, S, Zhang W, Servos T, O’Neill P. Cone beam computed tomography in dentistry: what dental educators and learners should know. J Dent Ed. 2012;76:1437–1442.
- Christenson, G. Do you need cone beam radiography? Available at: dentaleconomics.com/science-tech/article/16392463/do-you-need-cone-beam-radiography. Accessed August 21, 2019.
From Dimensions of Dental Hygiene. September 2019;17(8):44–47.



