Reduce Radiation With Rectangular Collimation
This underutilized technique can improve the quality of diagnostic radiographs while also reducing radiation exposure.

The goal of dental radiography is to obtain the highest quality images possible, while keeping patients’ exposure risk to the absolute minimum. Since the discovery of X-rays in 1895, radiographic image quality has improved, and radiation exposure to patients and professionals has been reduced due to advancements in technique and equipment. Introduced more than 20 years ago, rectangular collimators further reduce unnecessary radiation exposure and increase the quality of radiographic images and diagnostic yield, compared to cylindrical collimators. Nonetheless, their adoption in practice has been limited. Rectangular collimation deserves a revisit by oral health care practitioners committed to adhering to the “as low as reasonably achievable” (ALARA) principle.
SAFETY REGULATIONS
Concerned with preventing unwarranted exposure to radiation, the American Dental Association (ADA) and the federal Food and Drug Administration (FDA) have set comprehensive guidelines for the prescription of dental radiographs, including radiographic assessments of patient needs, exposure limits to protect patients and operators, and use of proper equipment.1 In addition, the National Center for Radiation Protection (NCRP) recommends that X-ray machines provide a range of exposures suitable for use with the fastest film speed or digital speed.2–4 Regulation of proper equipment includes selection of adequate X-ray field size and collimation devices. Specifically, federal regulations require internal and external cylindrical collimators to restrict the intraoral X-ray beam exiting the position-indicating device (PID) to a diameter of no more than 2.75 inches (7 cm) on the patient’s skin.1,5–8 Rectangular collimation can help practitioners comply with these regulations.
COLLIMATION
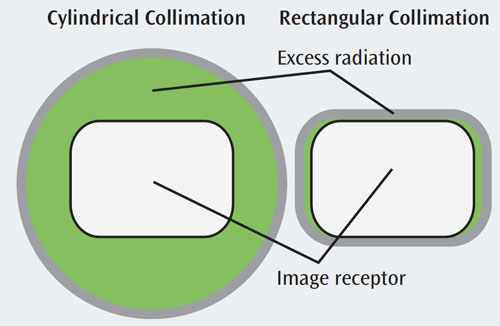
Collimation, the restriction of the cross-sectional area of the X-ray beam to conform to the size of the image receptor, is usually done with a lead collimator (diaphragm) within the tube head or at the end of a lead-lined cylinder. In addition to controlling the size, collimators also shape the X-ray beam. A collimator may have either a cylindrical or rectangular opening. Unlike round collimators, a rectangular collimator further restricts the size of the X-ray beam to the approximate size of an intraoral image receptor—greatly reducing scattered radiation, patient exposure (the measure of intensity of radiation at the patient’s skin), and dose (the amount of energy absorbed by the patient’s tissues).6–8 Scatter radiation, a type of secondary radiation, occurs when the useful beam intercepts any object, causing some X-rays to be scattered.
The larger the amount of tissue the beam is allowed to irradiate, the more scatter radiation is produced. Rectangular collimation greatly reduces the amount of scatter radiation.5–11 Figure 1 compares the scatter radiation produced using a cylindrical vs a rectangular collimator. Figure 2 illustrates the amount of excess radiation (green) reaching the patient’s tissues in relation to the image receptor (white rectangle) when using cylindrical and rectangular collimators. Figure 3A and Figure 3B and Figure 4A and Figure 4B show the exposure area on a patient’s face.
By reducing the beam to the approximate size of the image receptor, rectangular collimation results in a reduction of up to 70% of radiation exposure and absorbed dose.5–10 This reduction is associated with a decrease in malignant changes in the head and neck region, including thyroid gland, facial skin, and active bone marrow.2,11–14


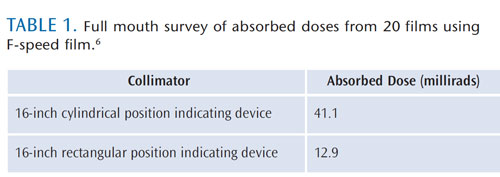
There are other methods to reduce radiation exposure, such as increasing film speed. For instance, a switch from D-speed to F-speed film reduces the absorbed dose by 60%.5–9 When rectangular collimation is added, patient exposure and dose are further reduced by about four times (Table 1).6


A reduction in excessive scatter radiation increases image contrast (the difference in the degrees of blackness between adjacent areas) and reduces noise/fog (gray film).2–4 Adopting rectangular collimation assists in not only reducing patient radiation exposure, but also in obtaining quality images that lead to improved diagnoses and treatments.
IMPLEMENTING THE TECHNIQUE
Despite its advantages, rectangular collimation has been underutilized in practice. Among the concerns cited are difficulties in using rectangular collimators, high number of cutoff errors, and cost of acquiring new equipment. Given the smaller size of the rectangular collimator, alignment may require more precision. Hence, practitioners may experience difficulty aligning the collimator with the receptor. Nonetheless, the recommended technique is the same for both cylindrical and rectangular collimation, namely the use of the paralleling technique, beam alignment devices, and image receptor holders.6–9 To improve the technique, radiographers can review the basic concepts of the paralleling technique, the receptor and placement procedures used, and the required equipment.
Cutoff errors may occur more frequently when a rectangular collimator is used. These cutoff errors render the radiograph undiagnostic, requiring retakes and defeating the purpose of reducing unnecessary radiation exposure and dose. Although cutoff errors appeared more frequently when a rectangular collimator was used, studies found it was a result of poor technique, eg, the PID was misaligned and the X-ray beam was not centered over the image receptor. More importantly, these studies found that despite the cutoff errors, most of the radiographs were diagnostically acceptable and retake was not required.6,12,14–16
Cutoff errors can be prevented with the use of image receptor holding devices. For instance, new extension cone paralleling (XCP) instruments align the image receptor and provide a visual reference point. Compatible with rectangular and cylindrical open-ended PIDs, the new XCP instruments have shorter arms that fit all intraoral X-ray units, and guide PIDs for proper alignment.
Some beam alignment devices or precision film holders include collimating shields and film-holding devices that restrict the size of the X-ray beam to the size of the receptor. Design innovations in beam alignment devices help practitioners achieve the ALARA principle and increase quality of diagnoses. There are affordable options to reduce the cost of switching to rectangular collimation. For instance, instead of replacing the whole X-ray tubehead, the cylinder PID can be replaced by a rectangular PID. The use of universal adaptors to convert a standard cylindrical PID to rectangular collimation is another affordable step.
Although many dental X-ray manufacturers sell machines that come with standard cylindrical PIDs, rectangular PID options are also available.
SUMMARY
Dental X-rays are an integral assessment tool when planning individualized comprehensive oral care, but radiography carries a small risk of radiation exposure. Reducing radiation exposure to patients and producing consistently high quality radiographic images are not mutually exclusive goals. The ADA, NCRP, and American Academy of Oral and Maxillofacial Radiology all recommend the use of rectangular collimation for periapical and bitewing radiography in order to reduce further radiation exposure and dose to patients.4,17–19
Despite its advantages, rectangular collimation has been underutilized in practice. To ease the transition to rectangular collimation, practitioners should review the basic concepts of the paralleling technique, ensure the proper alignment of PIDs, and purchase inexpensive adaptors, instead of new equipment.
Dental practitioners are responsible for protecting patients from excessive radiation by regularly updating the equipment, reexamining practices and techniques, and following recommendations for standards of care. Thus, purported reasons for failing to use rectangular collimation need to be investigated further and strategies to increase its utilization developed.
REFERENCES
- United States Food and Drug Administration.Guidelines for Prescribing Dental Radiographs.Available at: www.fda.gov/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures/ MedicalImaging/MedicalX-Rays/ ucm116506.htm. Accessed January 18, 2013.
- Rohlin M, White SC. Comparative means of dose reduction in dental radiography. Curr OpinDent. 1992;2:1–9.
- Ludlow JB, Davies-Ludlow LE, White SC.Patient risk related to common dental radiographic examinations: the impact of 2007International Commission on RadiologicalProtection recommendations regarding dose calculation. J Am Dent Assoc.2008;139:1237–1243.
- Mupparapu M. Radiation protection guidelines for the practicing orthodontist. Am J Orthod Dentofacial Orthop. 2005;128:168–72.
- Frommer HH, Stabulas-Savage JJ. Radiology for the Dental Professional.St. Louis: Mosby; 2011.
- Iannucci JM, Howerton LJ. Dental Radiography:Principles and Techniques. 4th ed. St. Louis:Saunders Elsevier; 2012.
- Thomson E M, Johnson ON. Essentials of Dental Radiography for Dental Assistants and Dental Hygienists.8th ed. Upper Saddle River, NJ:Pearson Education; 2012.
- Wilkins EM. Clinical Practice of the DentalHygienist. 11th ed. Philadelphia: Lippincott Williams & Wilkins; 2013.
- Langland OE, Langlais RP, Preece JW. Principles of Dental Imaging. Baltimore: Lippincott Williams & Wilkins, 2002.
- White SC, Pharoah MJ. Oral Radiology:D Principles and Interpretation. 6 ed. St. Louis:Mosby; 2000.
- Goren AD, Bonvento MJ, Fernandez TJ, et al. Evaluation of radiation exposure with Tru-Align intraoral rectangular collimation system usingOSL dosimeters. N Y State Dent J. 2011;77:24–27.
- Horton PS, Sippy FH, Nelson JF, Kohout FJ,Kienzle GC. A comparison of rectangular and cylindrical collimation for intraoral radiographs.J Dent Educ. 1983;47:771–773.
- Rush ER, Thompson NA. Dental radiographytechnique and equipment: how they influence the radiation dose received at the level of the thyroid gland. Radiography. 2007;13(3):214–220.
- Zhang W, Abramovitch K, Thames W, LeonIL, Colosi DC, Goren AD. Comparison of the efficacy and technical accuracy of different rectangular collimators for intraoral radiography.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:e22–e28.
- Parks ET. Errors generated with the use ofr ectangular collimation. Oral Surg Oral Med Oral Pathol. 1991;71:509–513.
- Parrott LA, Ng SY. A comparison between bitewing radiographs taken with rectangular and circular collimators in UK military dental practices: a retrospective study. Dentomaxillofac Radiol. 2011;40:102–109.
- Report No 145—Radiation Protection in Dentistry. Bethesda, Md: National Council onRadiation Protection and Measurements; 2003.
- American Dental Association Council onScientific Affairs. The use of dental radiographs:update and recommendations. J Am Dent Assoc.2006;137:1304–1312.
- Miles DA, Langlais RP, National Council onRadiation Protection and Measurement. NCRPreport No 145: New dental X-ray guidelines:their potential impact on your dental practice.Dent Today. 2004;23:128–134.
From Dimensions of Dental Hygiene. February 2013; 11(2): 46, 48–50.

